Why peroxide is still a good choice for lens care
Go down the eye care aisle at your local pharmacy or big box retailer and take a look at the contact lens care solutions. The choices can seem quite daunting to patients who have been given no recommendations before heading to the store.
Go down the eye care aisle at your local pharmacy or big box retailer and take a look at the contact lens care solutions. The choices can seem quite daunting to patients who have been given no recommendations before heading to the store.
There are a multitude of products available, yet they fall into two categories: multi-purpose solutions (MPS) and hydrogen peroxide (H2O2). MPS all have the same general mode of action: they disrupt microbial cell membranes and lead to cell death.1 We often think of H2O2 as a fairly harmless chemical compound because it breaks down into oxygen and water, yet H2O2 is a strong oxidizing agent and acts on proteins, lipids, and microbial DNA, all of which lead to cell death. Hydrogen peroxide provides excellent antimicrobial efficacy. It works by penetrating the lens material and cleans by expanding the lens matrix and oxidizing microbes. Because of its hypotonic nature and pH of 4.00, H2O2 is also able to break protein and lipid bonds and remove trapped debris.2 H2O2 is highly effective against all microorganisms when used in a 3 percent concentration but is non-selective in its activity.
Examining the symptoms, causes, and treatments of contact lens discomfort
Hydrogen peroxide has been in use as a contact lens disinfecting agent since the 1970s and remains a viable option for a reason-it works extremely well. Three percent H2O2 effectively disinfects the contact lens against a wide variety of pathogens that may adhere to a contact lens during a normal wearing cycle.3,4 The human body is well equipped to metabolize H2O2 in low concentrations (up to 800 ppm in topically applied ophthalmic drops).5,6 Because H2O2 is a common byproduct of human physiology, both the tear film and the ocular surface tissues have an abundance of enzymes capable of rapidly neutralizing dilute H2O2.5,7
Biofilm formation
Hydrogen peroxide can also penetrate bacterial biofilms. Biofilms are microbial communities adhering to a surface, and bacteria in biofilms have increased resistance to antimicrobials and host immune responses.8 One explanation for contact lens-induced infection despite good lens wear and care compliance is the ability of organisms to form biofilms on lens surfaces.9 A study by Loretta Szczotka-Flynn and associates showed that clinical and reference strains of Pseudomonas aeruginosa, Serratia marcescens, and Staphylococcus aureus formed biofilms on contact lenses. Of the solutions her group tested (five MPS and one peroxide system), only the H2O2 solution (Clear Care, Alcon) showed activity against all three strains.10 In another study, her group also found that only peroxide systems were effective against fungal biofilms of Fusarium oxysporum and Fusarium solani on the three lens types tested.11
Corneal infiltrates
While corneal infiltrates have long been a recognized problem with extended wear contact lenses, they can be seen in daily wear patients who have hypersensitivity concerns. H2O2 lens disinfection is a good option in this patient cohort. Chalmers and colleagues published a large-scale retrospective study involving thousands of lens wearers, and H2O2 had a lower rate of corneal infiltrates than the multipurpose solutions as a group. The authors speculated that, “even though hydrogen peroxide solutions do not carry a rubbing step, the volume of solution required and agitation created by the oxidation process may provide a less antigenic lens surface.”12
10 reasons contact lens care is important
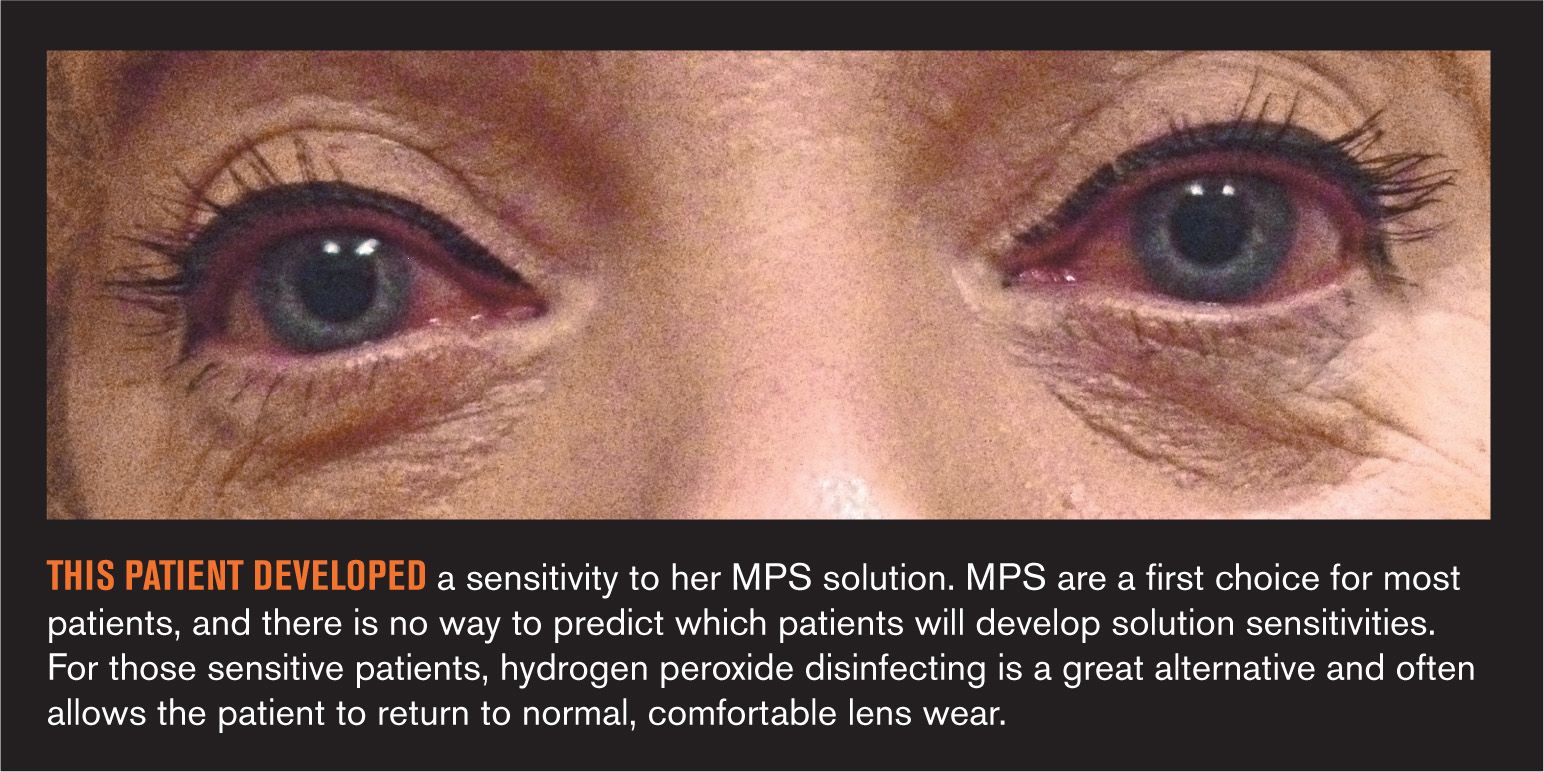
Comfort
Hydrogen peroxide care systems are preservative-free and are often used by contact lens wearers who may be sensitive to preservatives found in multi-purpose contact lens solutions. Patients who experience contact lens discomfort often benefit from changing to a H2O2 solution. Many patients in my practices who have discontinued contact lens wear can return to comfortable wear when they change to a H2O2 solution. In fact, I will change patients presenting with nonspecific comfort complaints to a H2O2 system before changing the lens type.
Hydrogen peroxide brands available
I found two name brands of peroxide systems in the eye care aisles I visited, along with several generics: Clear Care and PeroxiClear (Bausch + Lomb). Clear Care solution combines a surfactant cleaner and functional wetting agent with peroxide in a single bottle. It has a six-hour neutralization period and disinfected lenses can be stored for up to seven days. It has been FDA cleared for use with silicone hydrogel lenses. PeroxiClear allows for a four-hour neutralization cycle, vs. the six-hour cycle of other systems. It also features a redesigned basket system and includes Triple-Moist Technology which helps to provide up to 20 hours of moisture.
Generic hydrogen peroxide contact lens systems are appearing on store shelves. Patients often make choices based on cost alone, yet they may not get what they are paying for. There are significant differences in formulations among apparently similar products, and for that reason alone I believe it is important to recommend name-brand H2O2 care systems as well as MPS systems. Don’t assume your patients are using what you recommend. Constant reinforcement is necessary to make sure patients understand they need to use the care system we recommend.
Not the end all
One problem with H2O2 systems is that after the hydrogen peroxide has been neutralized, the solution remaining in the lens case has no disinfecting ability. It is possible the case and contacts can become contaminated if the case is opened and used to store contact lenses without adding fresh disinfecting solution. Patients also need to be careful that they do not apply hydrogen peroxide directly to the eyes.
H2O2 can be toxic to the epithelium, so we must instruct our patients about the importance of full neutralization of the peroxide. Emphasize to your patients this can be achieved only with the special case enclosed with the system. What remains after neutralization is unpreserved saline; patients should apply their lenses directly from the case. Rinsing the contact lenses with sterile saline is acceptable. The rare accidental instillation of full-strength 3 percent H2O2 usually produces temporary conjunctival injection and corneal epithelial staining and edema with ocular discomfort. While this incident alarms the patient, rinsing the eye, use of artificial tears, and discontinuing lens wear for a short while usually resolves the presentation. It is important to reassure the patient that no permanent damage is done.
Hydrogen peroxide-based contact lens disinfection systems are known for their exceptional disinfecting ability and compatibility with the ocular surface. It is these characteristics that have allowed hydrogen peroxide disinfection to remain an important option for our contact lens patients. In my practice, patients using H2O2 are the most loyal to that solution than any I have seen, and patient satisfaction is our ultimate goal.
References
1. Willcox M. Hydrogen peroxide versus multipurpose disinfecting solutions, what are the differences? July 2008. Available at: www.siliconehydrogels.org/editorials/jul_08.asp. Accessed 8/14/2014.
2. Gromaki SJ. Hydrogen peroxide disinfection. CL Spectrum. 2006;21(12):19.
3. Hiti K, Walchnik J, Faschinger C, et al. One- and two-step hydrogen peroxide contact lens disinfection solutions against Acanthamoeba: how effective are they? Eye(Lond). 2005 Dec;19(12):1301-5.
4. Kobayashi T, Gibbon L, Mito T, et al. Efficacy of commercial soft contact lens disinfectant solutions against Acanthamoeba. Jpn J Ophthalmol. 2011 Sep;55(5):547-57.
5. Chalmers RL. A review of the metabolism of hydrogen peroxide by external ocular structures. Intl Contact Lens Clin. 1995 Jan;22(8):143-7.
6. Chalmers RL. Hydrogen peroxide in anterior segment physiology: a literature review. Optom Vis Sci. 1989 Nov; 66(11):796-803.
7. Riley MV, Wilson G. Topical hydrogen peroxide and the safety of ocular tissues. CLAO J. 1993 Jul;19(3):186-90.
8. Zegans ME, Shanks RM, O’Toole GA. Bacterial biofilms and ocular infections. Ocular Surf. 2005 Apr;3(2):73–80.
9. Donlan RM, Costerton JW. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev. 2002 Apr;15(2):167–93.
10. Szczotka-Flynn LB, Imamura Y, Chandra J, et al. Increased resistance of contact lens-related bacterial biofilms to antimicrobial activity of soft contact lens care solutions. Cornea. 2009 Sep;28(8);918-26.
11. Retuerto MA, Szczotka-Flynn L, Ho D, et al. Efficacy of care solutions against contact lens-associated Fusarium biofilms. Optom Vis Sci. 2012 Apr;89(4):382-91.
12. Chalmers RL, Wagner H, Mitchell GL, et al. Age and other risk factors for corneal infiltrative and inflammatory events in young soft contact lens wearers from the Contact Lens Assessment in Youth (CLAY) Study. Invest Ophthalmol Vis Sci. 2011 Aug 24;52(9):6690-6.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.