Vision loss diagnosis presents potential complications
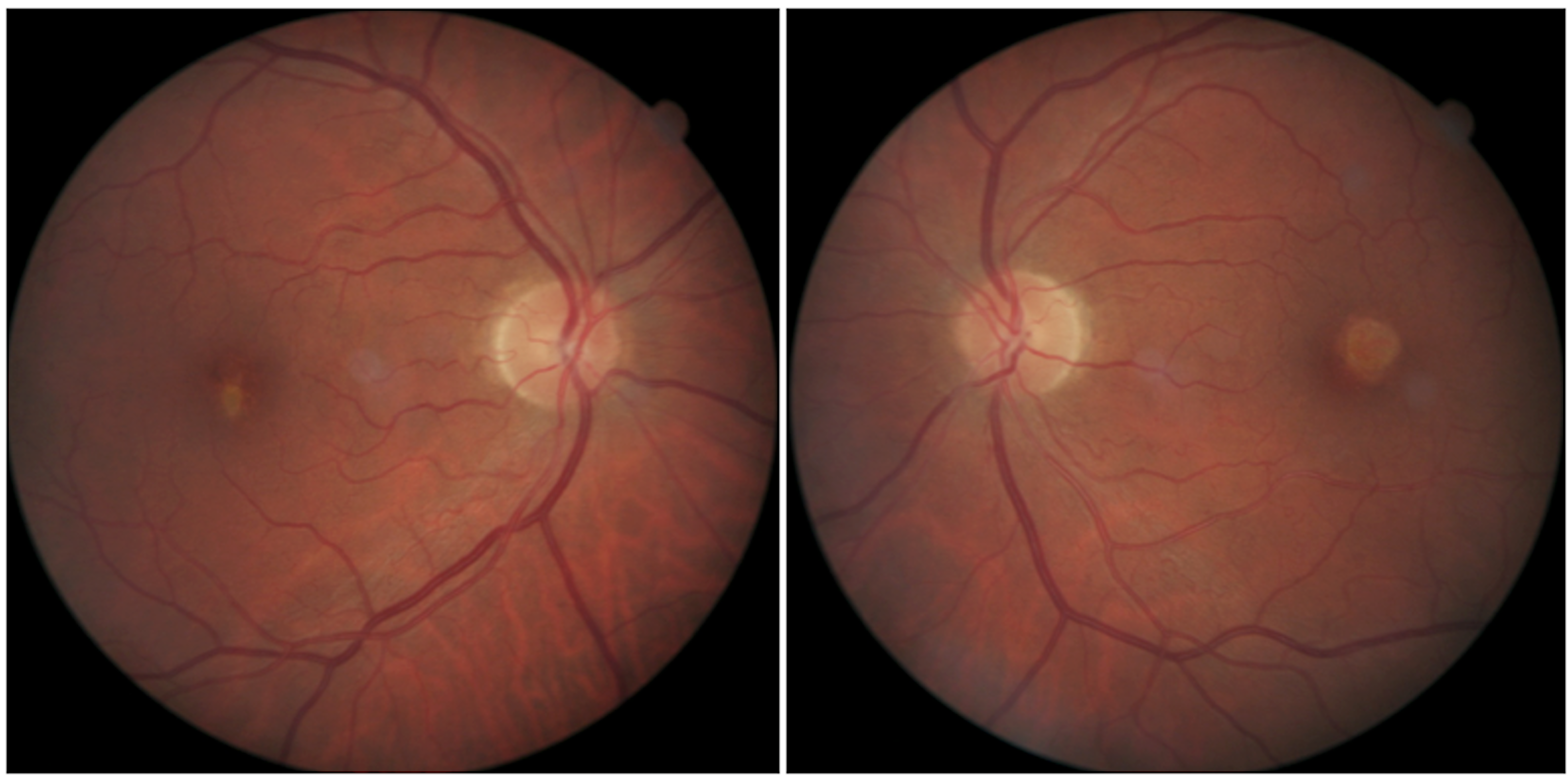
Figure 1. The right and left fundus images of the case. Note that the area of involvement is greater in the left eye, and on stereoscopic examination the lesion did not show elevation.

A 55-year-old white male attended the clinic for evaluation with a vague chief complaint of reduced vision in each eye. He reported that this problem was mild, had been present for an undetermined period of time, the situation was approximately equal in each eye, and the “blur” was similar at distance and near. He denied eye pain of any sort as well as flashes, floaters, and discharge.
There are a number of pertinent items in this patient’s history.
At the time of his visit, he was homeless and domiciled at a shelter. He had served time in prison and been involved in multiple fights. He reported taking no medications, denied the use of any alcohol or illicit or recreational drugs, and used over-the-counter reading glasses for near visual tasks.
Previously by Dr. Semes: Case: New protocol for macular hole treatment
Examination
Visual acuity was measured at 20/20 OD and 20/25 OS, not improving with pinhole or refraction. Evaluation of pupillary responses to light, extraocular muscle movements, and gross estimation of anterior chamber depth was normal. Slit-lamp examination of the anterior segment failed to reveal abnormalities.
Following pupillary dilation, the lens of each eye showed cortical changes that appeared premature for the patient’s chronological age.
Examination of the retina in each eye revealed the findings shown in Figure 1.
What appeared to be geographic atrophy in the right eye was incongruent with the clinical picture and visual acuity of the left eye. I was unable to reconcile the visual complaints and acuity reduction with retinal findings alone and discounted significant contribution from the lens changes.
Related: The case of the blurred disc margins
Best disease
Ruling out geographic atrophy and questioning the patient regarding practices such as sungazing with denial, I considered the diagnosis of early adult-onset vitelliform macular dystrophy (AOVMD)-also known as Best disease.
The clinical presentation spectrum of this disorder is varied-as is its terminology-and not all diagnosed patients suffer vision loss.1-5
this case, the disorder manifested lipofuscin deposition deep in the retina. This could be seen in the right eye when evaluated with optical coherence tomography (OCT) (Figure 2, see right).
This presentation was consistent with a case reported recently by Seanna Grob, MD, MAS, and colleagues.3 The left eye showed apparent absence of photoreceptors and retinal pigment epithelium (RPE) centrally.
There is, however, a variety of presentations that may show visual complications as well as the characteristic vitelliruptive form commonly seen in patients with Best disease.1,2,4,6
Related: Clinical findings supported by new OCTA technology
Better prognosis
While the presentation of Best disease in younger patients is more common and devastating visually, the adult-onset form appears to have a somewhat better prognosis.7 However, that is not to say that the adult form is without potential complications.
Along with neovascularization and macular edema, macular-hole associated retinal detachment has been reported as a consequence.4,5,8
In the present case, which was the first identification, there is no apparent indication of macular thinning-which portends a better prognosis than if macular thinning had been identified.1,5
While the prognosis remains guarded for this patient, the current visual status is encouraging.
Related: Why in-person care and technology must partner
AOVMD has been characterized by imaging modalities. The consensus diagnostic characteristics from OCT include a hyper-reflective area at the outer retina with no material visible between the photoreceptor cells and RPE layers.3,8
Each of these manifestations occurs in the present case. The pathophysiology has been proposed to include photoreceptor outer segment hypoplasia and impaired phagocytosis.9
Phenotypes, while varied, may have commonality with other ocular disorders as diverse as vitreomacular traction, age-related macular degeneration (AMD) pseudodrusen, and central serous chorioretinopathy (CSR).8
Conclusion
While this patient reported no previous symptoms consistent with a diagnosis of previous CSR, it may be tempting to speculate that it was a component of this presentation, along with other unknown factors.
Management of AOVMD includes explanation of the guarded prognosis to the patient, regular monitoring for complications that may be amenable to treatment, and genetic counseling.
This last item is significant, as the age of onset may be as young as 40 years. Finally, ODs can play a role in visual rehabilitation in cases of vision loss.
Read more by Dr. Semes
References:
1. Pierro L, Tremolada G, Introini U, Calori G, Brancato R. Optical coherence tomography findings in adult-onset foveomacular vitelliform dystrophy. Am J Ophthalmol. 2002 Nov;134(5):675-80.
2. Benhamou N1, Souied EH, Zolf R, Coscas F, Coscas G, Soubrane G. Adult-onset foveomacular vitelliform dystrophy: a study by optical coherence tomography. Am J Ophthalmol. 2003 Mar;135(3):362-7.
3. Grob S, Yonekawa Y, Eliott D. Multimodal imaging of adult-onset foveomacular vitelliform dystrophy. Saudi J Ophthalmol. 2014 Apr;28(2):104-10.
4. Bhakhri R. Spectral domain optical coherence tomography and auto-fluorescence findings in adult-onset vitelliform dystrophy. Clin Exp Optom. 2015 May;98(3):292-3.
5. Querques G, Zambrowski O, Corvi F, Miere A, Semoun O, Srour M, Souied EH. Optical coherence tomography angiography in adult-onset foveomacular vitelliform dystrophy. Br J Ophthalmol. 2016 Dec;100(12):1724-1730.
6. Balaratnasingam C, Hoang QV, Inoue M, Curcio CA, Dolz-Marco R, Yannuzzi NA, Dhrami-Gavazi E, Yannuzzi LA, Freund KB. Clinical Characteristics, Choroidal Neovascularization, and Predictors of Visual Outcomes in Acquired Vitelliform Lesions. Am J Ophthalmol. 2016 Dec;172:28-38.
7. Jun I, Lee JS, Lee JH, Lee CS, Choi Si, Gee HY Lee MG, Kim EK. Adult-Onset Vitelliform Macular Dystrophy caused by BEST1 p.Ile38Ser Mutation is a Mild Form of Best Vitelliform Macular Dystrophy. Sci Rep. 2017 Aug 22;7(1):9146.
8. Chowers I, Tiosano L, Audo I, Grunin M, Boon CJ. Adult-onset foveomacular vitelliform dystrophy: A fresh perspective. Prog Retin Eye Res. 2015 Jul;47:64-85.
9. Tewari R, Kumar V, Ravani R, Dubey D, Chandra P, Kumar A. Macular hole-associated retinal detachment in Best vitelliform dystrophy: Series of two cases and literature review. Indian J Ophthalmol. 2018 May;66(5):708-711.

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.