Vision therapy: A top 10 must-have list
My name is Marc, and I am a vision therapy graduate. I was your typical kid, except that I could not pay attention in school and hated to read. Luckily, my second grade teacher requested that I get an eye examination, and the optometrist recognized that I needed more than glasses. I was referred to an optometrist that specialized in learning-related vision problems, including visual efficiency and processing disorders. I immediately started a vision therapy program and saw tremendous improvement in my symptoms and success in school.
My name is Marc, and I am a vision therapy graduate. I was your typical kid, except that I could not pay attention in school and hated to read. Luckily, my second grade teacher requested that I get an eye examination, and the optometrist recognized that I needed more than glasses. I was referred to an optometrist who specialized in learning-related vision problems, including visual efficiency and processing disorders. I immediately started a vision therapy program and saw tremendous improvement in my symptoms and success in school. When I entered optometry school, despite my background, I did not instantly gravitate toward the vision therapy department. It was during my first job after graduation that the light bulb went off; I realized my true calling. Vision therapy has the potential to help so many people, to change lives.
More from Dr. Taub: Treating patients with brain injuries
Over my 10-plus years in practice I have developed a core set of equipment that I cannot live without. While some would be considered basic, others are more complicated. It is this mixture of high and low tech that keeps patients interested and enables the uploading and downloading of activities to meet therapeutic needs. I hope that my top 10 pieces of vision therapy equipment will quickly become yours.

Figure 1. Wolff wands
1. Wolff wands
It is amazing that a simple design can be so powerful. Created by Bruce Wolff, the wands are two 1-foot-long metal rods with either a gold or silver ball at the end (Figure 1). These wands can be used for activities related to tracking and convergence, but most importantly, they are crucial for an activity known as eye control. In any successful program of vision therapy, the patient must understand where his eyes are pointing in relation to his body. Eye control is performed early in therapy and aimed at achieving this understanding. It is the reflective nature of the balls on the wand that make them irreplaceable. If the patient sees his reflection, he knows that he is pointing his eyes at the intended target.
Next: Hart charts
2. Hart charts
Hart charts can be used for accommodation, eye movements (saccades), and visual attention. There are two charts of rows of letters, one small and one large (Figure 2). The patient typically stands 10 feet from the distance chart and holds the smaller chart in her hand. If working on accommodation, there are three levels to be accomplished: near chart at arm’s length, slowing moving toward the patient while reading, and as close as possible before becoming blurry. The patient alternates reading a line from the distance and near charts during the activity. The activity can be made more challenging by alternating charts every half of a line.
Video: Questions to ask in vision therapy
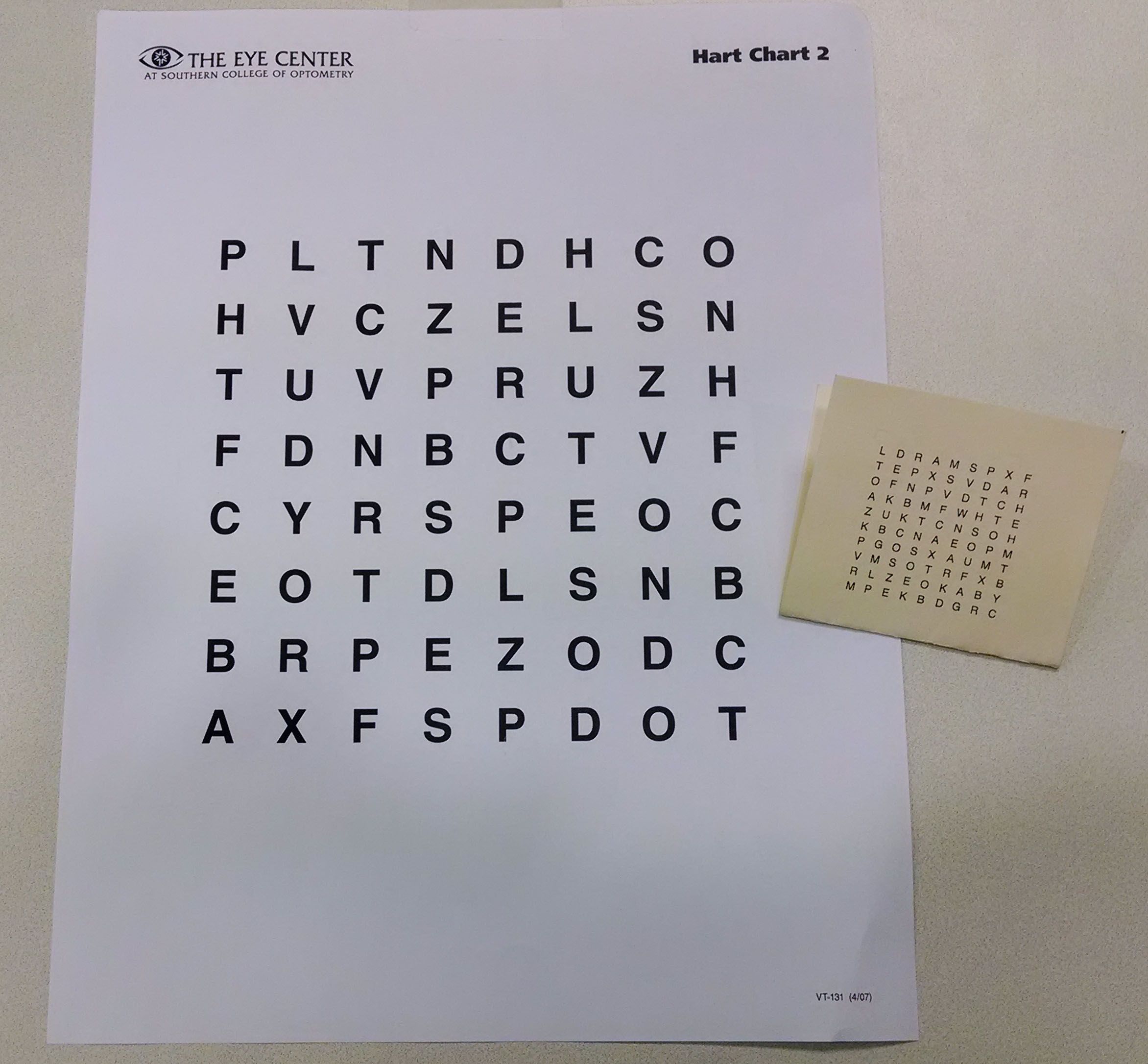
Figure 2. Hart chartsFor saccadic work, only the distance chart is used. The patient is instructed to read the outside two columns, one letter at a time, alternating between the two columns. As she becomes more proficient, she begins to read the columns in the same manner moving inward, eventually reading the two most inner columns.
Next: Brock string

Figure 3. Brock string
3. Brock string
No, despite what everyone says, using the Brock sting cannot treat conjunctivitis, but it is unbelievably useful on so many levels in the therapy room. A key component to a therapy program is the appreciation of physiological diplopia. The different colored beads (red, yellow, and green) can be placed anywhere along the string (Figure 3), depending upon the area of fusion. When focused on one of the beads, the patient should appreciate two of each of the other beads. Once physiological diplopia is appreciated, the patient can jump between the beads or do a controlled Bug on a String. The position of the crossing of the strings provides feedback for the patient, as well as the therapist. Suppression is easily detected if two strings do not enter and exit the bead. Red/green glasses can also be used because the red and green beads will cancel and not be seen by both eyes.
Next: Marsden ball
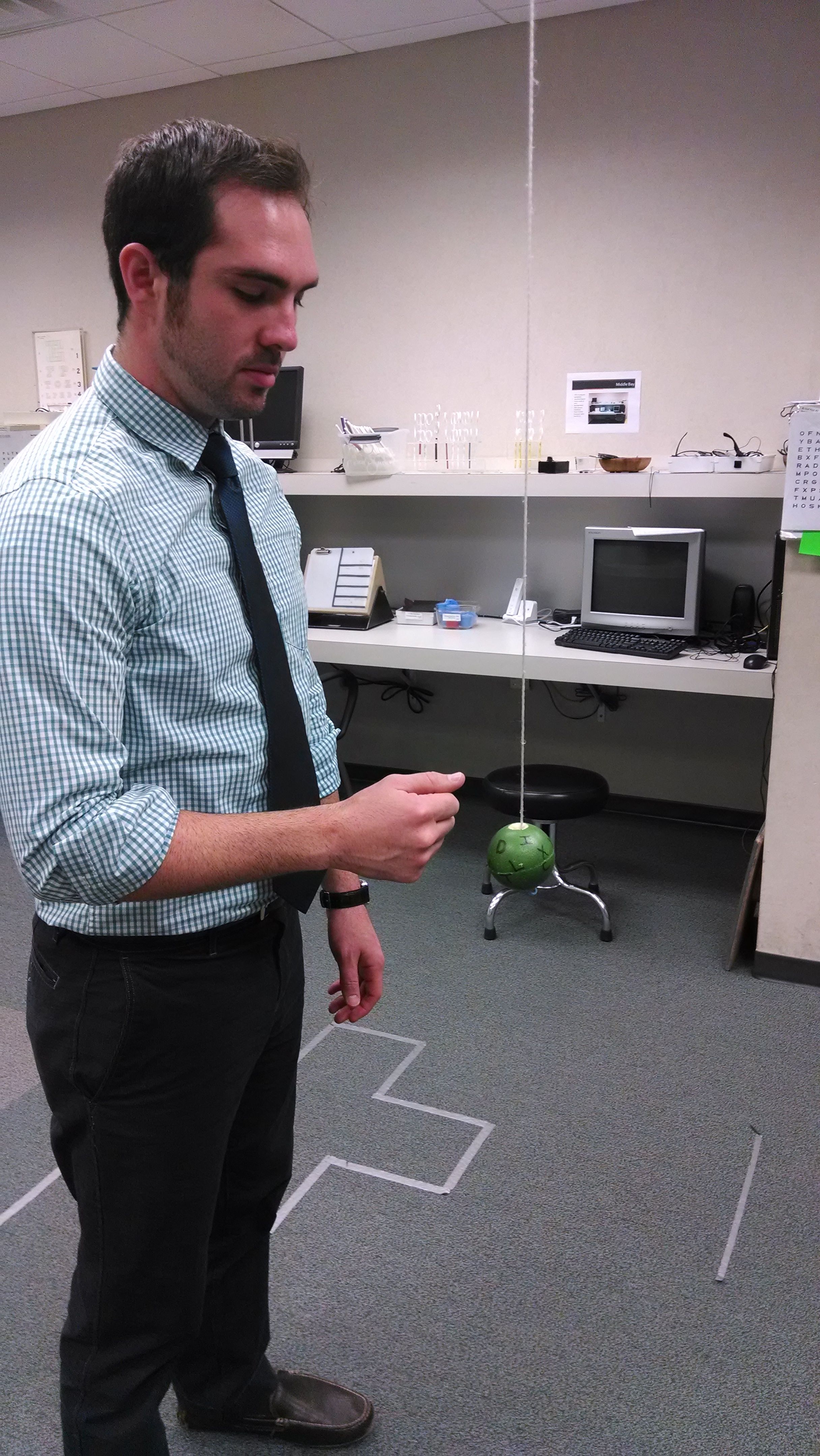
Figure 4. Marsden ball
4. Marsden ball
Activities that are performed with the Marsden ball are fun and perhaps the most desired in the therapy room. We have become experts at making our own balls using a Pinky ball and a baseball glove repair kit. Writing letters on the ball with a Sharpie allows for the activities to focus on visual attention. The ball is hung from the ceiling and can be bunted with a dowel, and hit/caught with the thumbs, palms, and fists (Figure 4).
Next: Vectographs
5. Vectographs
There are many different vectographs, which can be confusing for the novice therapist, but each one has a purpose in the sequence of therapy. Whereas tranaglyphs are red/green and are subject to lighting problems, the polarized vectographs are easily visible and not as finicky. The different vectographs have differing visual demands and target sizes. For example, the Quiot and Gem (Figure 5) are great peripheral targets with no central demand, while the Spirangle, Clown, and Vortex contain both peripheral and central demands (letters). All of the vectographs enable the patient to appreciate the SILO (small in/large out) phenomenon, which is a key aspect of a successful therapy program.
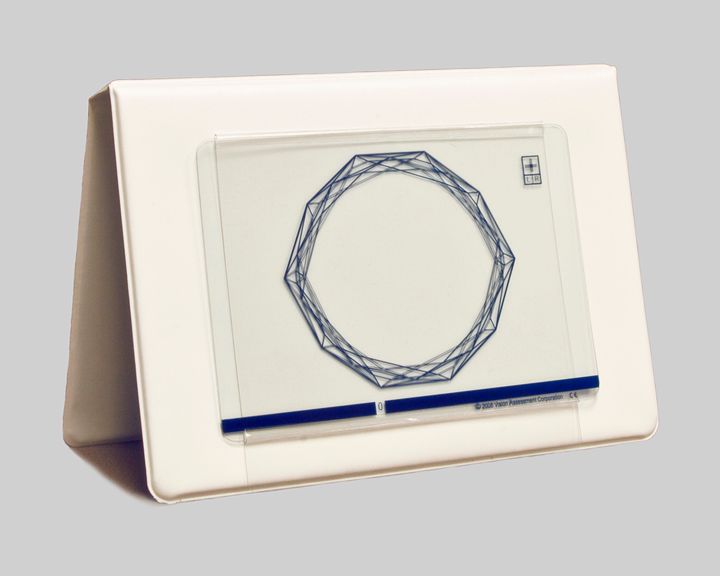
Figure 5. Vectograph
Next: Balance board
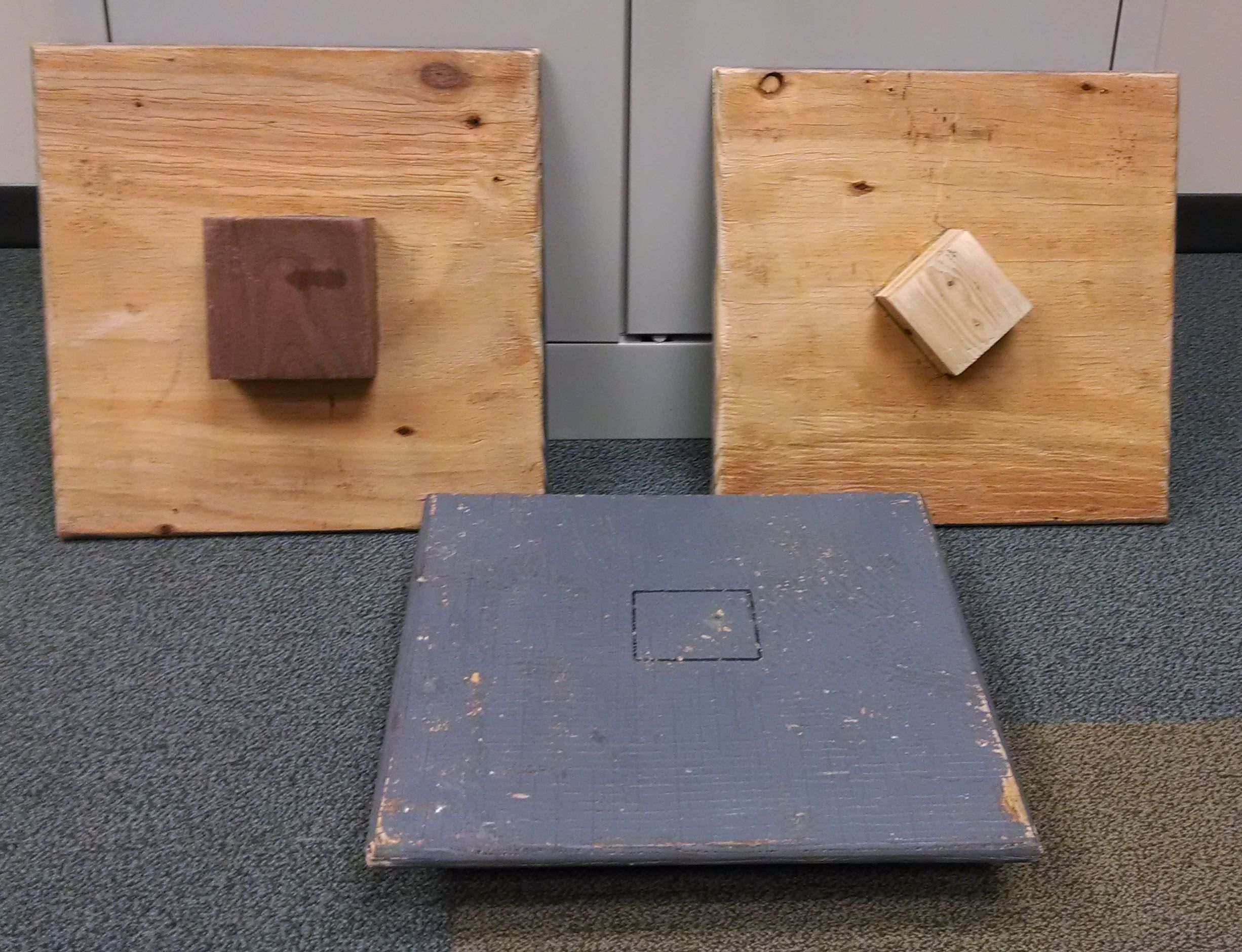
Figure 7. Balance board
6. Balance board
The balance board addresses the concept that while the eyes are part of the body, they must move independently of the head and the body. Eye movements are deemed inefficient if there is accompanying body and/or head movement. The balance board is a square wooden board with a base (Figure 7). The base can be square or round and there are several levels of difficulty. The patient stands on the board and attempts to shift his hips only from side to side. It is harder than it seems, and some patients have to start at a lower level and stand on the board or perform the activity holding the therapist’s hands.
Next: Rotator
7. Rotator
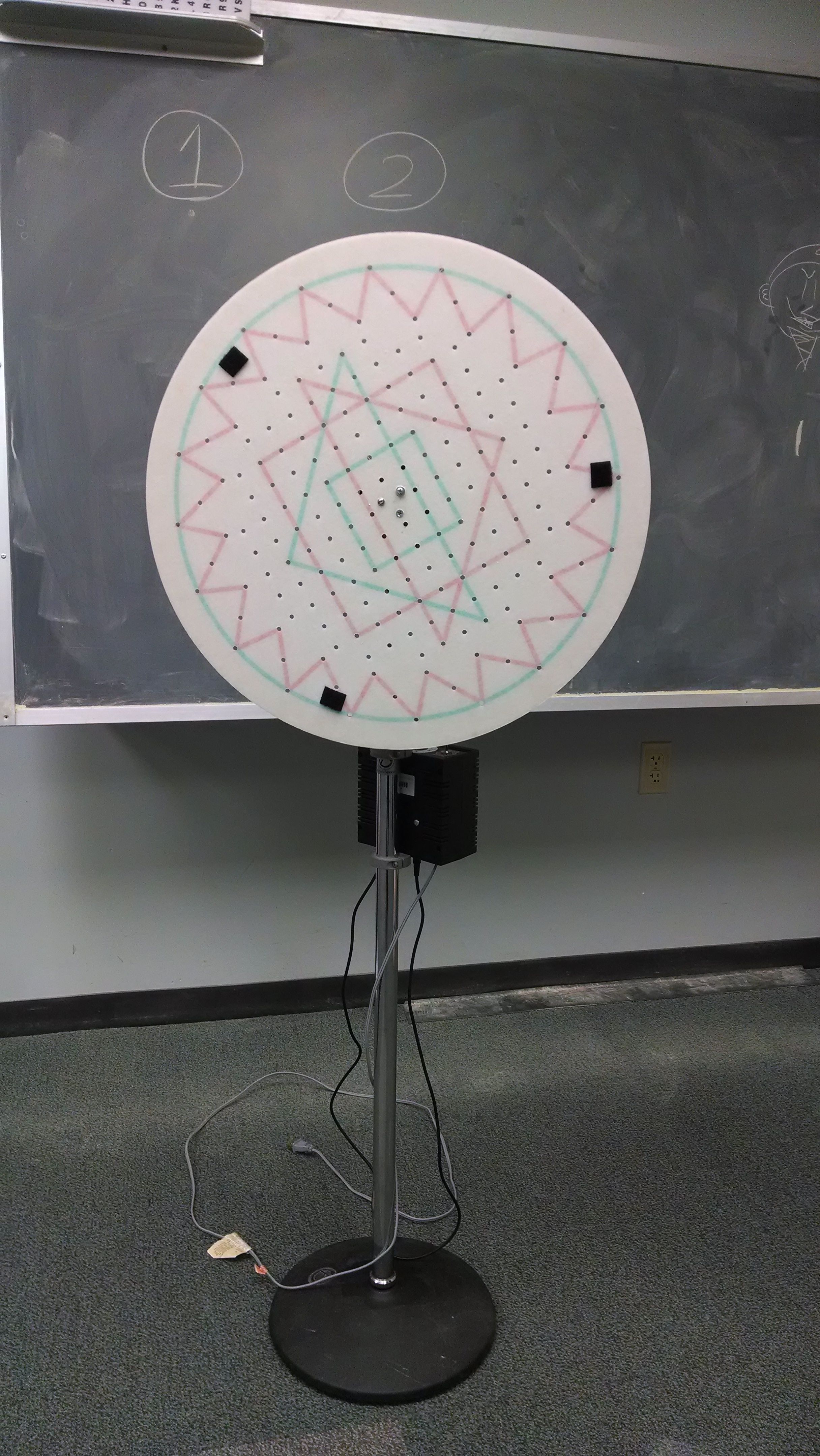
Figure 8. RotatorAs discussed earlier, efficient eye movements are crucial to reading and the learning process. The standing (Figure 8) or tabletop rotator is used to address concerns related to poor fixation, pursuits, and visual attention. Numerous plates aimed at various purposes can be used with the device. Some have more peripheral vs. central targets, while others have designs in red/green to address suppression. The speed of the rotator can be controlled and the demand altered based on speed and target location.
Next: Lenses and prism
8. Lenses and prism
Lenses and prisms are absolutely essential, and it confounds me that these items might not be on someone’s top 10 list. While lenses and prisms are used early on in the therapy program with the introduction of a single lens or prism, they are also used in a facility-type manner later on. Lens blanks are used to facilitate an understanding that the patient, not the lens, controls her accommodation. She must clear a minus lens with the lens in place and blur the image without the lens in place. As the program progresses, lenses are used in a bi-ocular and then binocular fashion in the form of flippers.
Related: Researchers use video games to treat amblyopia
Prism is used to facilitate an understanding of the eye moving in a specific direction. Strabismics often have difficulty with this basic task. Teaching a patient with esotropia what it feels like when his eye is pointing inward is a necessary step. Prism facility flippers are used to increase flexibility in the vergence system as the patient alternates between convergence and divergence demands.
Next: Rotator glasses

Figure 9. Rotator glasses
9. Rotator glasses
These glasses come in powers ranging from 2^ to 45^. The direction of the prism can be rotated enabling either yoked (same direction) or dissociated (different direction) prism (Figure 9). Yoked prism is very useful when working with patients with special needs, including autism and developmental delay, as well as those who have suffered a traumatic brain injury. When performing an activity with yoked prism, the patient has to reorient his visual system to coordinate successful completion. The ability to alter input is a needed aspect of a therapy program.
10. Computer programs
It is amazing how far computer programs have come in the 30 years since I personally went through a therapy program. Yes, many of the basic concepts are still in place, but the intricacy and variety of programs is outstanding. Computer-based activities can be performed both in the office, at home to support office-based therapy, and as a stand-alone home-based program. The office-based approach to therapy has been shown to be more successful,1 but these programs allow greater access for patients who cannot attend weekly sessions. Depending on the program selected, activities can stress vergence, accommodation, eye movements, and visual information processing. Each program is unique, and each practice should investigate which ones work best for its model of vision care.
Next: Bonus

Figure 10. Sanet Vision Integrator
Bonus: Sanet Vision Integrator
Yes, I already covered my top 10, but the Sanet Vision Integrator is knocking on the door to that list and is a hit with the patients. It is a 52-inch touch screen (Figure 10) that can be used with any variety of patients. Activities are aimed mostly at eye movements but with a twist: the tactile aspect of the touch screen brings in eye-hand coordination. The target size, color, location, and contrast can all be controlled, which is an asset when working with brain injury patients or those with amblyopia. This is quickly becoming one of the most-used therapy activities in my repertoire.
Related: Reviewing pediatric primary care optometry
Even though vision therapy is not just for children, a high percentage of participants are in fact young. On the surface, some of these activities are more exciting than others and, unfortunately, that is just how it is sometimes. That does not mean that the activities cannot be made fun by using incentives or creating a competition between the therapist and the patient or even between patients. I suggest trying to space the higher energy, more fun activities throughout the therapy session to keep the child’s attention. Also, keep in mind that younger children and those with attention challenges will need shorter-duration activities to keep them engaged. If needed, the activity can be broken into two shorter parts. Vision therapy is all about engaging the patient to enact meaningful and long-lasting change, so do not be afraid to take off the white coat, get on the floor, and have fun!ODT
References
1. Convergence Insufficiency Treatment Trial Study Group. Randomized clinical trial of treatments for symptomatic convergences insufficiency in children. Arch Ophthalmo. 2008 Oct;126(10):1336-49.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.





.png&w=3840&q=75)











