Why keratometry is important
Keratometry (K) is the measurement of the corneal curvature; corneal curvature determines the power of the cornea. Differences in power across the cornea (opposite meridians) results in astigmatism; therefore, keratometry measures astigmatism. It can be acquired with a variety of instruments either manually or via automated methods.
Keratometry (K) is the measurement of the corneal curvature; corneal curvature determines the power of the cornea. Differences in power across the cornea (opposite meridians) results in astigmatism; therefore, keratometry measures astigmatism. It can be acquired with a variety of instruments either manually or via automated methods. Measurements can be very sophisticated, such as with topographers, that measure a cornea across a broad number of points, or it can be measured in a more finite area of the cornea, for example with a manual keratometer or with the IOL Master (Carl Zeiss Meditec). The IOL Master also measures the axial length and other ocular parameters (such as anterior chamber depth and white-to-white measurements) and includes K readings.
Manual vs. automated
Personally, I prefer manual keratometry because it provides a clear understanding of the integrity of the pre-corneal tear film, a dynamic view of the surface of the cornea. With manual keratometry, you have a direct visualization of the reflections generated by the tear film. You can recognize areas of corneal surface irregularity or compromise. If the tear film is oily or disrupted, or the cornea has subtle dystrophy or degeneration, it will be reflected in the quality of the measurements (akin to the changes of a pebble tossed into a placid lake). You have a much better understanding of the quality and accuracy of your measurements.
With automated measurements, acquisition is static. The measurements are acquired at a moment in time and computer generated. As the instrument operator, you have no appreciation of the accuracy of the “measured moment.”
Keratometry is a critical measurement in cataract surgery because errors in measurements are matched 1:1 to refractive outcomes. If you’re 1.00 D off in your K readings, you will have a 1.00 D refractive surprise. If your K is inaccurate, you will have an unexpected refractive surprise post-operatively. In this generation of cataract surgery and premium intraocular lenses (IOLs), a refractive miss outcome is very disappointing to the doctor and the patient. Correcting residual ammetropia in cataract postoperative patients may require a second surgical procedure, be it IOL exchange, piggy-backing of an additional IOL, or a surface procedure.
If there’s any doubt in your K readings, they should be redone on another day. We will repeat K readings if there is any indication of a problem or if the measurement is difficult to acquire. I typically measure the right eye, then the left eye, then repeat to verify.
If I’m uncomfortable with any aspect of my measurement-if the patient has dry eye disease or comes in wearing contact lenses, for example-I will have the patient return after dry eye treatment and no contact lenses wear for 1 to 3 weeks, depending on the lens type. Your first K measurement may not be the one you use for surgery. If you’re taking measurements for cataract surgery, it’s the first thing you want to do before instilling drops, performing gonioscopy, or anything that may compromise the corneal surface.
Although it’s not hard to learn, it takes a little practice to be sure you have accurate measurements in manual K. You need to be confident in your measurements before you put your findings down on a piece of paper. At Omni Eye Surgery, only doctors, including residents, will perform keratometry for patients planning cataract surgery.
Some surgeons prefer the most updated automated K for their surgeries. It’s smart to compare manual with automated to get a better idea because each method measures different areas of the cornea; however, measurements should correlate. Also, you should expect correlation of the measured corneal cylinder with the patient’s spectacles.
Next: The importance of an accurate reading
The importance of an accurate reading
Managing the corneal surface before ocular surgery is very important. Sometimes patients are referred for cataract surgery; however, the cataract is not the primary problem, the corneal surface is. In some cases, patients who have had their corneal surface rehabilitated have opted out of cataract surgery because the problem was more so poor corneal surface than the cataract. Clinical clues can be picked up during keratometric measurements that help you identify more subtle cornea degeneration, such as basement membrane dystrophy, that can be more difficult to identify and easy to overlook via slit lamp examination. Patients with corneal dystrophy need to be educated that although their vision will be better after cataract removal, a corneal concern remains that may affect their post-operative vision.
Any time an operator has difficulty generating a measurement, immediately try to identify why. It could be dry eye, a compromised cornea, meibomian gland dysfunction, corneal disease, or even poor patient positioning or fixation during examination.
It is of the utmost importance to be proficient in keratometry. With the responsibility of those measurements, the surgeon is putting the patient's surgical outcome in your hands. It’s up to you to make sure they’re clean and raise a flag if they’re not.
Keratometric measurements are also critical in fitting contact lenses, particularly gas permeable lenses, for monitoring corneal pathology and for identifying keratoconus. Often you first identify your keratocones with keratometry.
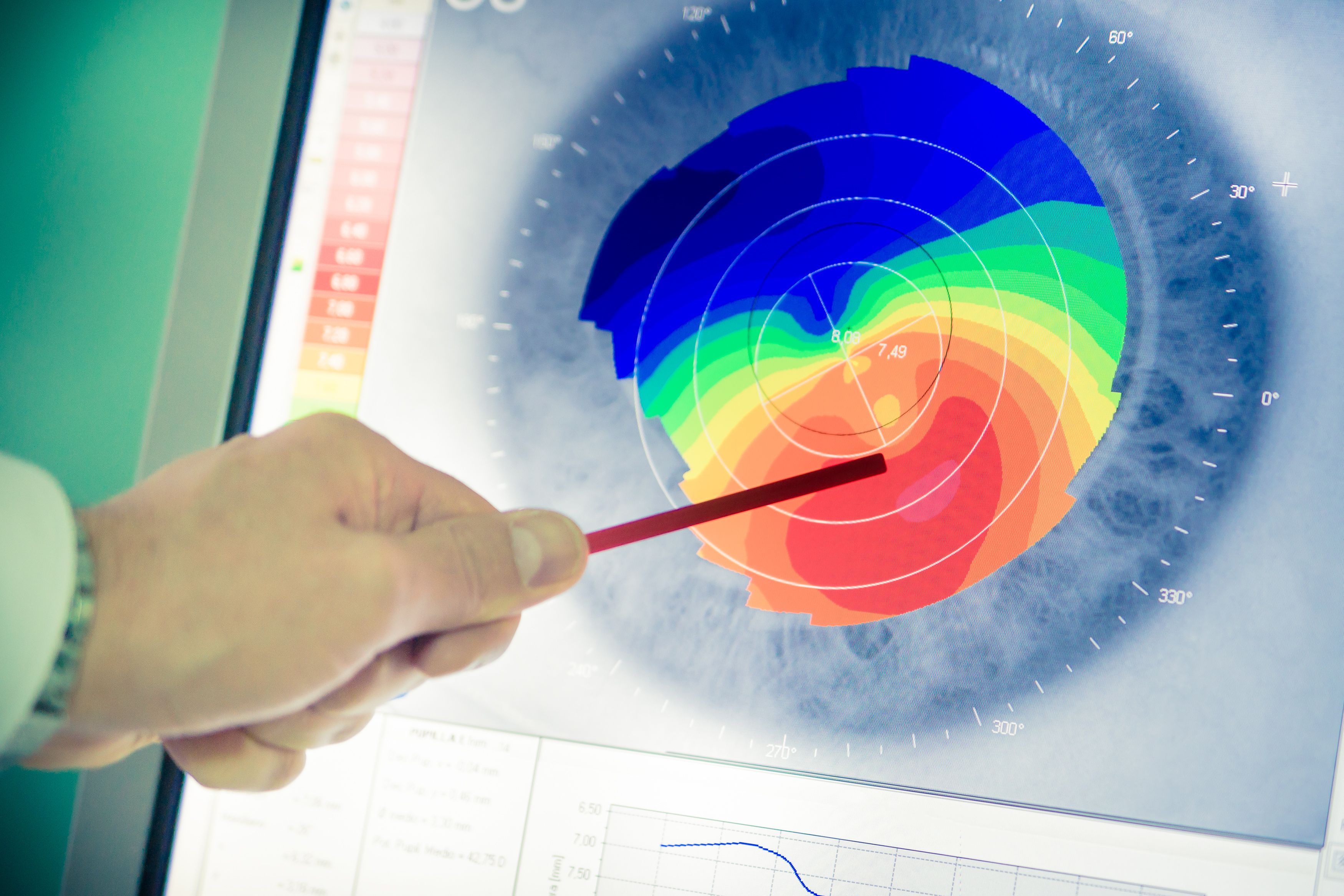
Keratoconus
Keratoconus is a degenerative disease of the cornea causing abnormal and irregular steepening (and irregular astigmatism) of the cornea that results in reduced vision, scarring, and potential perforation of the cornea. Sometimes a patient will come in with unexplained reduced vision until the tech takes K readings. Then we learn that the cornea is completely abnormal, which is responsible for the reduced vision. Treatment options for keratoconus include corneal crosslinking, gas permeable contact lenses, Intacs (embedded stromal rings), and penetrating keratoplasty (corneal transplant).
If the K readings are outside of what is considered a normal range or if there is irregularity in the mires, that instantly clues you into the potential pathology of keratoconus. Now with corneal crosslinking, the sooner we identify it, the sooner we can slow down the progression of corneal steepening.
Practitioners prefer automated, some prefer manual keratometry. The most important thing is that we have several ways to acquire these measurements. They should all correlate and make sense. If they vary wildly, the measurements should be retaken and reviewed in order to rule out other pathology.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.