Why you should add upper lid eversion to your comprehensive exam
Comprehensive ocular examinations can provide an OD with an inside look into a patient's health. Mile Brujic, OD, and David Kading, OD, discuss the importance of using upper eyelid eversion during the exam to unleash significant information about a patient's ocular surface and systemic health.
The views expressed here belong to the author. They do not necessarily represent the views of Optometry Times or UBM Medica.
ODs identify a number of conditions while performing a comprehensive ocular examination. Undiagnosed diabetes, hypertensive retinopathy, or other systemic condition may be identified during a patient’s eye exam.
A common slit lamp evaluation technique that may help uncover both local ocular and systemic problems-upper eyelid eversion (UEE). It is so important that we perform it on every patient. This provides significant information about patients’ ocular surface and systemic health.
Previously from Dr. Brujic and Dr. Kading: Work with patients to combat contact lens obsolescence
Palpebral conjunctiva health
Everting the upper eyelid gives ODs an indication of the health of the palpebral conjunctiva. In a normal contact lens-wearing individual, we expect to see a smooth tarsal surface. In a patient who is abusing his contact lenses, the normally smooth, healthy tarsal surface may develop significant irritation and hyperemia.
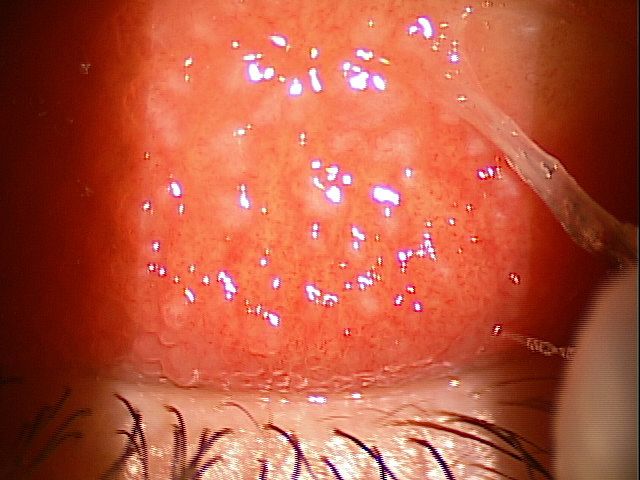
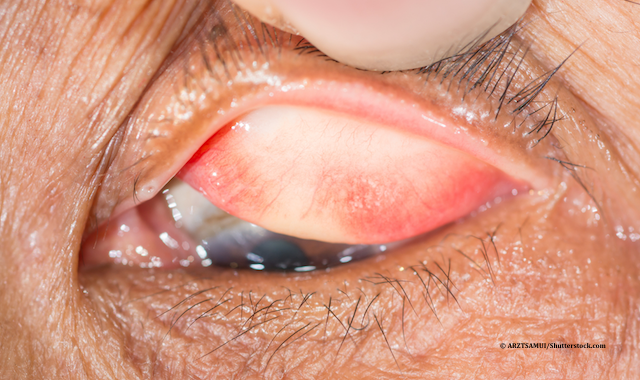
Figure 1. Giant papillary conjunctivitis (GPC)
In some individuals, this may lead to giant papillary conjunctivitis (GPC). In the most severe forms, GPC is identified by the patient’s symptoms which may include fluctuating vision, uncomfortable contact lenses, and also lenses that seem to move significantly with the blink. This may occur because the large papillae formed will adhere to the lenses and may cause significant movement with the blink.
Early to moderate forms of GPC present in a more subtle way. Most patients complain about comfort. Often this will lead the clinician to refit contact lenses to optimize comfort when in fact it is a problem with the health of the palpebral conjunctiva. By performing an upper eyelid eversion on every patient, you may easily uncover GPC and provide better treatment options for patients.
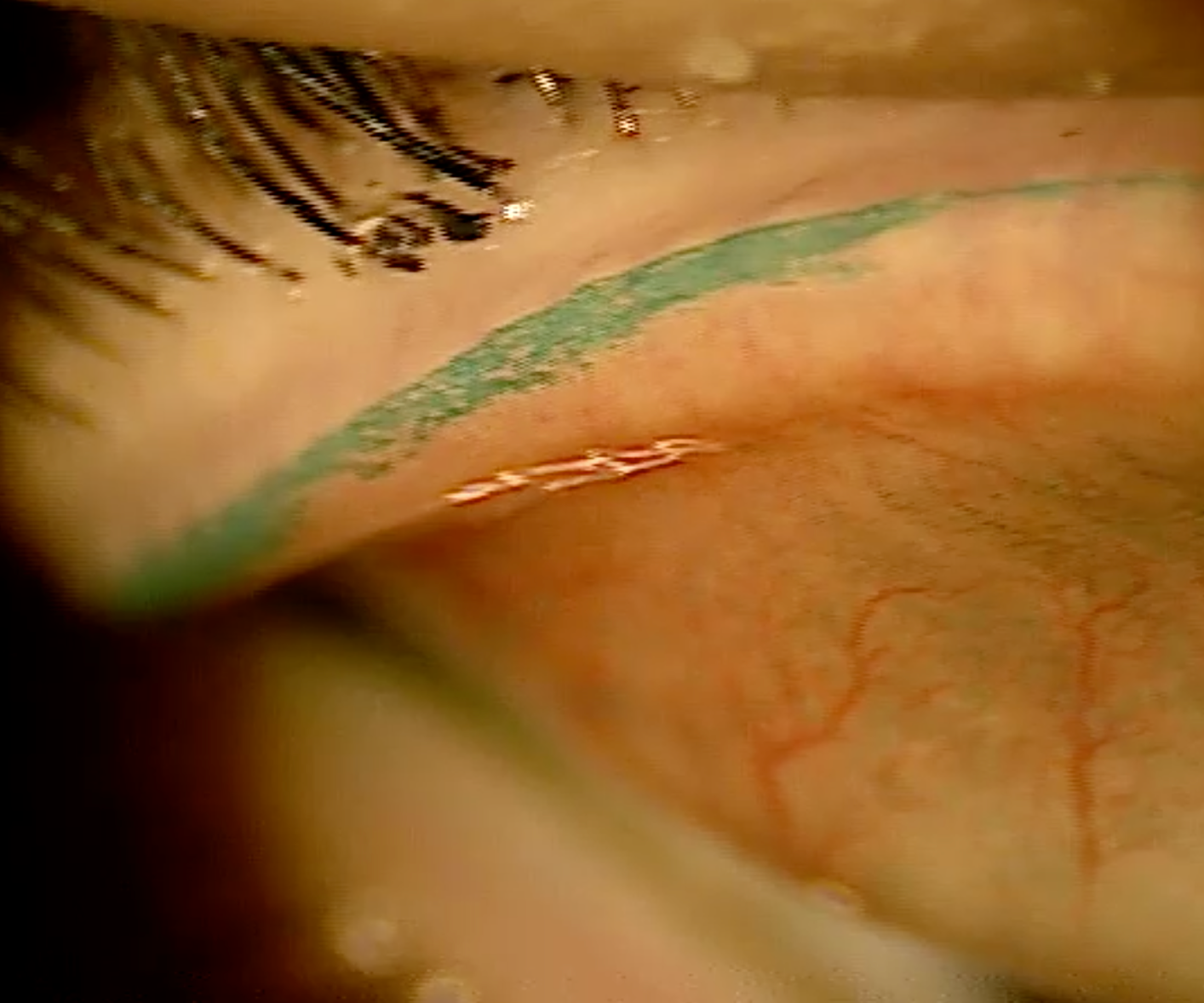
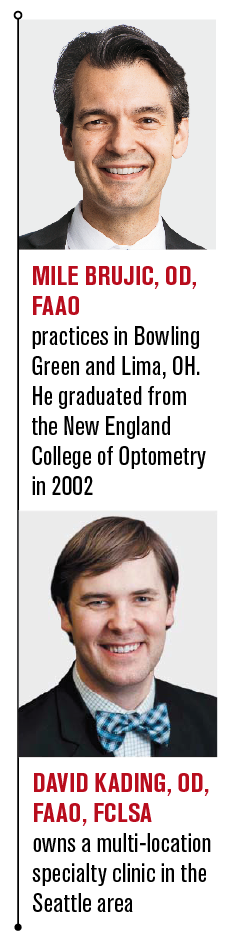
Figure 2. Lid wiper epitheliopathy (LWE)
LWA becomes visible
Also visible upon UEE is the lid wiper area (LWA). This is the small tissue located posterior to the meibomian glands on the upper eyelid. The LWA is responsible for physically “wiping” along the ocular surface during the blink. In the presence of poor tear film, increased friction occurs between the LWA and the ocular surface. In this instance, vital dyes applied to the eye will be absorbed in the irritated tissue. This is termed lid wiper epitheliopathy (LWE).
Dyes that will stain this region are:
• Fluorescein
• Lissamine green
• Rose bengal
LWE is a critical diagnostic sign in dry eye disease and one we monitor over time. LWE may present with different severity (See Figures 1-4). Without UEE, this cannot be seen.
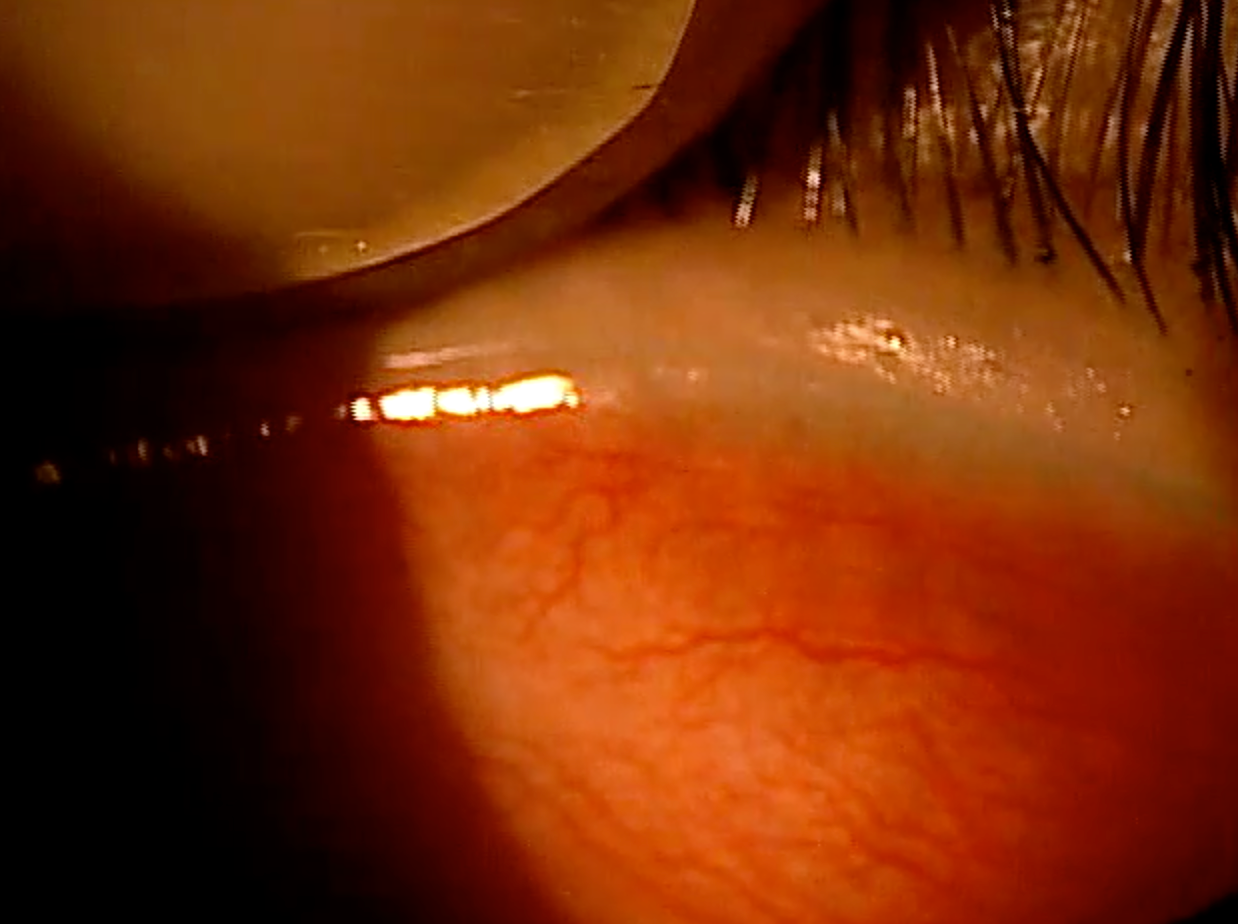
Figure 3. Lid wiper epitheliopathy (LWE)
Identify floppy eyelid syndrome
Everting the upper eyelid is also critical in identifying floppy eyelid syndrome (FES). Individuals with FES may present with general ocular discomfort very similar to a dry eye patient. In more severe forms, patients may come in with acute conjunctivitis, including conjunctival hyperemia, corneal staining, and a papillary response on the palpebral conjunctiva.
Related: 3 tips to better fit keratocones with sclerals
FES patients may have lower levels of elastin in their upper eyelids, causing upper eyelids that more easily evert than in the normal individual. It is very evident in these individuals to identify FES upon attempted UEE. It is critical to rule FES out if you suspect dry eye may be causing the symptoms in order for these patients to be treated properly. Typical defense may include ocular lubricants, some form of eye shield in the evening, and in more severe forms an upper eyelid resection.

Figure 4. Lid wiper epitheliopathy (LWE)
FES and sleep apnea
FES is critical to identify in patients because of its association with sleep apnea. Often patients forget to report sleep apnea upon initial medical history questioning. When we identify FES and ask about obstructive sleep apnea (OSA), these patients tend to admit to sleep apnea treatment.
Knowing if a patient has OSA is important because they may be prone to FES. OSA patients are frequently treated with continuous positive airway pressure through masks worn in the evening.1
For those patients not currently diagnosed with sleep apnea, it is important to educate them about the association of FES with OSA and potentially further investigate his health with his physician.
Everting unveils upper eyelid findings
Everting the upper eyelid is critical to identifying several conditions. If you do not evert the eyelid, it may be difficult to appreciate the influence of the upper eyelids on the ocular surface and the link with certain systemic conditions.
References
1. McNab, AA. Floppy eyelid syndrome and obstructive sleep apnea. Ophthal Plast Reconstr Surg. 1997 Jun;13(2):98-114.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.