Blood-derived serum tears go beyond conventional therapy
A recent patient’s experience highlights how autologous serum tears can help heal the ocular surface and provide relief of dry eye symptoms.
Case presentation
A 53-year-old female presents on referral from her rheumatologist for a dry eye consultation. She has been under the care of her rheumatologist for rheumatoid arthritis (RA) and Sjögren’s syndrome (SS). She reports that she has been under the care of another eye doctor for several years. However, despite trying a number of different dry eye treatments, she continues to struggle with intermittent blurred vision and burning throughout the day. Extended hours on the computer exacerbate her symptoms.
Risk factors for her dry eye disease include:
• Post-menopausal female
• Medications with a known drying effect Zoloft (sertraline, Pfizer) and Benadryl (diphenhydramin,e Johnson & Johnson)
• Autoimmune disease (RA and secondary SS)
• >4 hours of electronic device use each day.
Her current treatment regimen includes preservative-free Systane Ultra (Alcon) q3h, Systane Gel (Alcon) qhs, Restasis (cyclosporin, Allergan) bid, FML (fluorometholone, Allergan) 0.1% bid, and six-month extended-duration plugs in the lower punctum OU inserted approximately four months ago.
Related: 3 updates to treating Sjögren’s syndrome and dry eye
She reports trying scleral contact lenses in the past, but she was unable to wear them for any extended period of time. Insertion and removal was challenging, so she ultimately gave up on them.
She also reports being prescribed Xiidra (lifitegrast, Novartis), but she says it was cost prohibitive.
The patient’s entrance testing showed best-corrected visual acuity (BCVA) of 20/20- OU. Meibography exhibited mild tortuous gland morphology but no gland dropout. Tear osmolarity scores were abormal (314 OD, 323 OS). The patient also had a positive Schirmer tear test without use of topical anesthetic.
Biomicroscopy revealed scant (concave) tear film in both eyes. Lissamine green staining was positive for both the nasal and temporal conjunctiva as well as the central cornea OU with grade 2 staining (Figure 1).
The patient has 2-3+ central punctate epithelial keratitis (PEK) OU which was most evident with fluorescein. Remnants of the extended-duration plugs were evident in lower puncta in both eyes. Blink reflex was complete in both eyes.
Discussion
After I completed my assessment, I explained the severity of her condition and educated her on my recommended treatment.
Based on Dry Eye Workshop (DEWS) II guidelines, on a severity scale of 1 to 4, she would be considered to have Grade 3 dry eye disease.
While her autoimmune disease is the primary underlying cause of her signs and symptoms, her dry eye is likely exacerbated-at least to some degree-by the use of Zoloft and Benadryl.
Related: Offer IPL as a treatment for MGD and dry eye disease
Given her past and current therapies, and given her persistent signs and symptoms, I felt that autologous or allogenic serum eye drops, otherwise known as “serum tears” may be a good next step for her. I explained how important our own natural tears are to our ocular surface and corneal health.
Our natural tears are composed of key components not found in artificial tear products, such as epidermal growth factor (EGF), fibronectin, and vitamin A, which support the proliferation, maturation, migration, and differentiation of corneal and conjunctival epithelia.1
We also know that serum contains IgG, lysozymes and complement, which have bacteriostatic properties. If these factors are low or missing, there is increased risk of persistent epithelial defects, blurred vision, infection, and scarring.
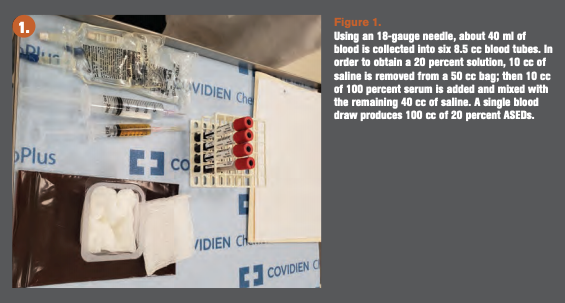
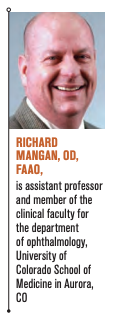
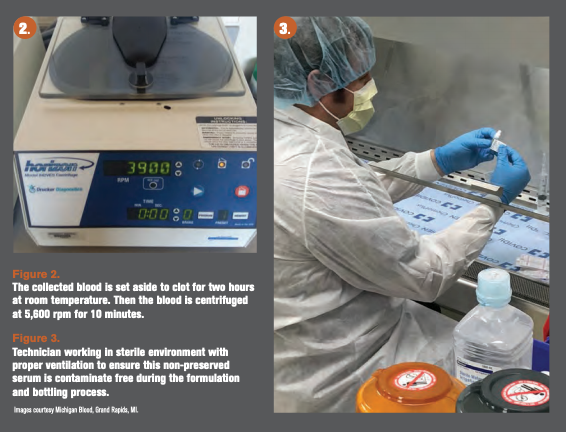
I explained that serum is derived from whole blood after the blood is donated by the patient (autologous serum), a family member (allogenic serum), or a blood donor (fresh frozen plasma [FFP] or ABO-ready allogeneic serum]. Using a variety of methods of blood collection, storage, centrifugation, filtration, and dilution, we are able to formulate serum tears in which the serum components closely mimic our own natural tears.
Autologous serum has been used for ocular surface disease since the mid 1980s with a track record for a variety of different ocular surface conditions, including SS-related dry eye disease.2-4
However, there is debate about whether patients with secondary SS should use their own serum. Some evidence suggests that pro-inflammatory cytokines may be re-introduced to the eye-higher amounts of serum inflammatory markers have been identified in patients with secondary SS as compared to those with primary SS or age-matched controls.5
I explained that, in my experience, there have been many success stories with autologous serum in secondary-SS patients, but there may be merit to considering allogenic serum.
The patient indicated that she had no family members in the immediate vicinity, and the thought of asking one of them to donate blood for her serum tears every three months would be an unreasonable request. This led to discussing FFP allogenic serum eye drops.
FFP serum tears are formulated from whole blood that is acquired through general blood donations at a blood bank or center. Unlike autologous serum, each donor is required to complete a blood donor questionnaire, and each donation is typed, cross-matched, and tested for infection (See box).
Testing is negative prior to the product being shipped. There also must be no previously detected red blood cell antibodies.
While donors can be male or female, female donors must have no history of pregnancy or they must be HLA antibody negative. Donors must be medication free, including aspirin.
Once a request is submitted for serum, which must include the patient’s blood type (A, B, AB, or O), a match is made and serum tears are shipped to the patient’s regional collection facility for dispensing. This takes on average about two weeks. Approximately 650 single-use ampules will arrive packed in dry ice. Each ampule holds approximately six drops of serum.
Related: Dry eye protocol for any practice
According to Harritshøj and colleagues: “The eye is an immunologically privileged site, and ABO substances and HLA antigens are present on the cornea and conjunctiva. In this context, serum may contain high amounts of clinically relevant antibodies, such as ABO and HLA antibodies, which upon immune complex formation might activate complement and initiate inflammation.
Furthermore, serum may contain high amounts [of] ABO substances that again might act as antigens and initiate immune complex-mediated inflammation. Therefore, we decided to produce allogeneic serum drops covering all four ABO types and providing patients with ABO-identical eye drops.”6
I explained to the patient that the cost of FFP serum is about twice the cost of autologous serum for a three-month supply of tears. The advantage to allogenic serum is that she would not have to personally give blood every three months.
After weighing the risks, benefits, and alternatives, we mutually agreed to start with 25 percent autologous serum eye drops (ASEDs) and re-assess after three months. Initial dosing will be QID, but I may need to increase it to Q2 to three hours, or switch to 50 percent ASEDs. If we determine serum tears are beneficial and worth staying on for an extended period of time, we can revisit the idea of FFP allogenic serum tears.
The patient can expect to receive approximately 10 5mL bottles (3 to 4 mL fill) of ASEDs. Each bottle should last for seven to 10 days depending on the dosing regimen.
She was instructed on the importance of keeping her unused ASEDs stored in the freezer and keeping her active bottle stored in the refrigerator to reduce the risk of contamination. Under no circumstances is she allowed to share her ASEDs with others.
Once she starts ASEDs, she can discontinue Systane Ultra and Restasis. She can use her Systane Ultra, however, if she is traveling for a short period of time or if she runs out of serum. She was asked to decrease FML to once a day and continue Systane Gel at bedtime.
While she was not asked to stop Zoloft or Benadryl use, she was educated on the adverse effects anti-depressants/anxiety agents and oral antihistamines can have on the ocular surface. She will discuss alternatives with her primary-care physician.
Follow-up visit was scheduled for six weeks.
Related: How to help patients who are depressed
Follow-up
The patient presented for follow-up as directed. She indicates that her blood draw and collection of serum tears went smoothly. She started the ASEDs approximately one month prior to the follow-up visit. She says that she takes one bottle to work with her and stores it in the refrigerator there. She uses the drops about every three hours because they are soothing to her eyes.
She says that she can already tell a difference in her comfort level and for the first time in a long time, she is “less aware of her eyes” than before. Her eyes still feel dry, but it is more tolerable.
Slit-lamp biomicroscopy showed modest improvement in surface staining of the conjunctiva and cornea. However, at her three-month follow-up visit, there was marked improvement in surface staining OU. While she still exhibited some central corneal staining, there was at least a 30 to 40 percent improvement OU.
The patient reported an improvement in the quality of her vision and says it does not fluctuate as much. Given this, the patient elected to stay the course with her current treatment regimen, including another round of 25 percent autologous serum.
Conclusion
Human serum contains a plethora of bioactive elements naturally released by activated platelets, which has been shown to offer a regenerative effect of corneal layers by stimulating cell growth.
The concept of using serum as an eye drop is based on the understanding that there are biochemical similarities between an individual’s serum and natural tears.7
There have been a number of studies demonstrating the wound healing effects of ASEDs.8,9
But it has been the work of rheumatologist Robert Fox, MD, PhD, and ophthalmologist Kazuo Tsubota, MD, that has driven renewed interest in ASEDs for severe dry eye disease. They were among the first to study and report notable clinical improvement in both signs and symptoms related to severe dry eye in SS patients using ASEDs.1,10
The use of human serum eye drops continues to evolve. Through continued research, we are learning more about the positive effects of alternative blood products such as platelet-rich-plasma,11 umbilical cord serum,12 and allogenic albumin,13 to name a few.
More studies are being conducted in an effort to standardize protocols in procurement and compounding of these products.
Access to serum tears also continues to evolve. While more compounding pharmacies are working with blood centers to efficiently produce serum tears, companies such as Vital Tears have mobile blood units that cover just about every ZIP code in the United States. In some cases, Vital Tears can arrange to collect blood at the patient’s home residence, then ship or deliver the final product within one to two weeks.
Who knows where we will be 10 years from now with blood-derived products in the fight against dry eye disease? What we do know is that currently, despite variability in how serum is derived or prepared, most clinical studies on autologous or allogenic serum confirm that serum eye drop therapy is effective in corneal healing and reducing ocular symptoms. When conventional therapy has not met expectations for moderate to advanced dry eye patients, serum tears may make the difference.
More by Dr. Mangan: Branded vs generics: You make the call
References:
1. Tsubota K, Goto E, Fujita H, et al. Treatment of dry eye by autologous serum application in Sjögren’s syndrome. Br J Ophthalmol. 1999 Apr;83(4):390-5.
2. Higuchi A. Autologous serum and serum components. Invest Ophthalmol Vis Sci. 2018;59:DES121–DES129.
3. Geerling G, Maclennan S, Hartwig D. Autologous serum eye drops for ocular surface disorders. Br J Ophthalmol. 2004 Nov;88(11):1467-74.
4. Semeraro F, Forbice E, Nascimbeni G, Taglietti M, Romano V, Guerra G, Costagliola C. Effect of autologous serum eye drops in patients with Sjögren syndrome-related dry eye: clinical and in vivo confocal microscopy evaluation of the ocular surface. In Vivo. 2016 11-12;30(6):931-938.
5. Hwang J , Chung SH, Jeon S, Kwok SK, Park SH, Kim MS. Comparison of clinical efficacies of autologous serum eye drops in patients with primary and secondary Sjögren syndrome. Cornea. 2014 Jul;33(7):663-7.
6. Harritshøj LH, Nielsen C, Ullum H, Hansen MB, Julian HO. Ready-made allogeneic ABO-specific serum eye drops: production from regular male blood donors, clinical routine, safety and efficacy. Acta Ophthalmol. 2014 Dec;92(8):783-6.
7. Quinto GG, Campos M, Behrens A. Autologous serum for ocular surface diseases. Arq Bras Oftalmol. 2008 Nov-Dec;71(6 Suppl):47-54.
8. Poon AC, Geerling G, Dart JK, Fraenkel GE, Daniels JT. Autologous serum eyedrops for dry eyes and epithelial defects: clinical and in vitro toxicity studies. Br J Ophthalmol. 2001 Oct;85(10):1188-97.
9. Jeng BH, Dupps WJ. Autologous serum 50% eyedrops in the treatment of persistent corneal epithelial defects. Cornea 2009 Dec;28(10):1104-8.
10. Fox RI, Chan R, Michelson JB, Belmont JB, Michelson PE. Beneficial effect of artificial tears made with autologous serum in patients with keratoconjunctivitis sicca. Arthritis Rheum. 1984 Apr;27(4):459-61.
11. Lee JH, Kim MJ, Ha SW, Kim HK. Autologous Platelet-rich Plasma Eye Drops in the Treatment of Recurrent Corneal Erosions. Korean J Ophthalmol. 2016 Apr; 30(2): 101-7.
12. Alio JL, Rodriguez AE, Ferreira-Oliveira R, Wróbel-DudziÅska D, Abdelghany AA. Treatment of dry eye disease with autologous platelet-rich plasma: a prospective, interventional, non-randomized study. Ophthalmol Ther. 2017;6:285-93.
13. Seki JT, Sakurai N, Moldenhauer S, Dam J, Atenafu EG, et al. Human albumin eye drops as a therapeutic option for the management of keratoconjunctivitis sicca secondary to chronic graft-versus-host disease after stem-cell allografting. Curr Oncol. 2015 Oct;22(5):e357-63.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.