Do ODs take chronic inflammation seriously?
With an advanced understanding of the ocular surface and inflammation levels, ODs can optimize the management of patients’ clinical outcomes and promote wellness of the ocular surface.

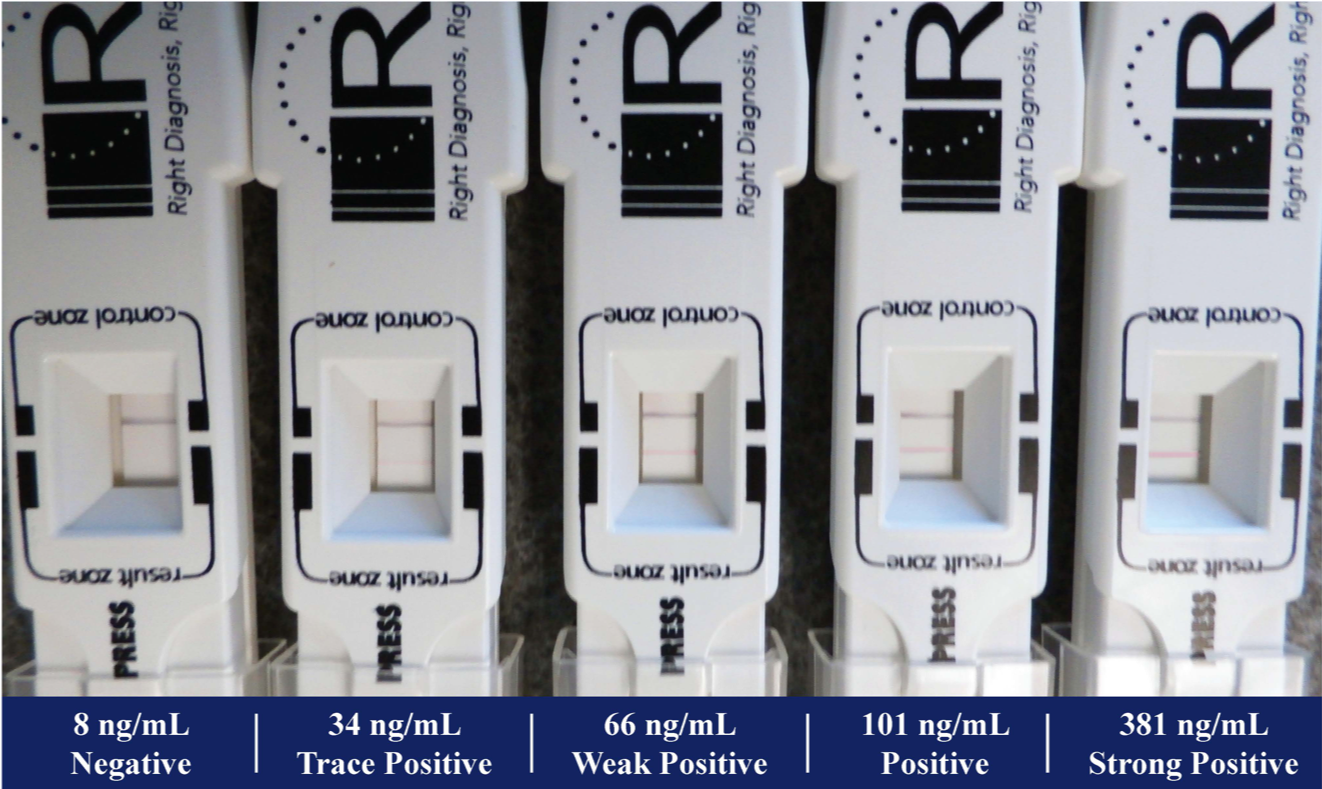
Figure 2 - Grading scale
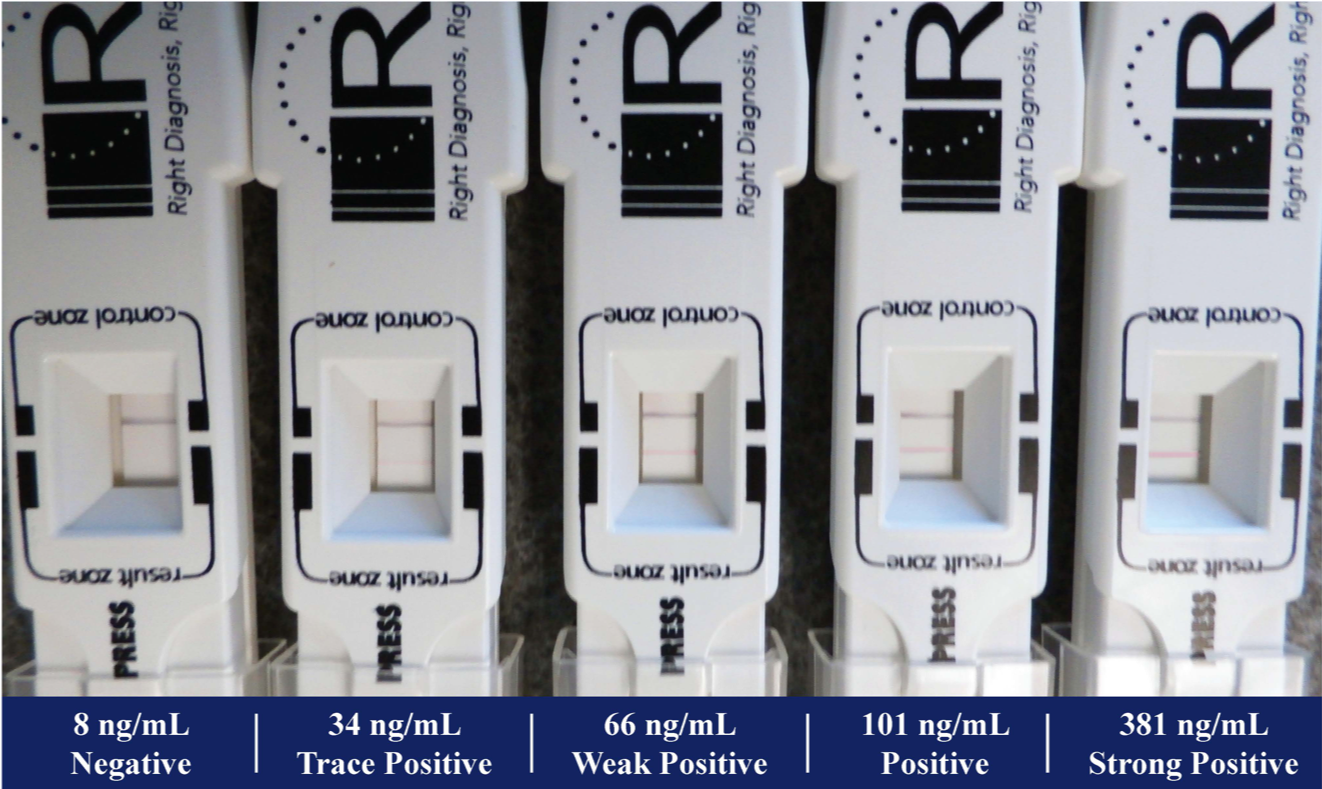
Figure 2 - Grading scale
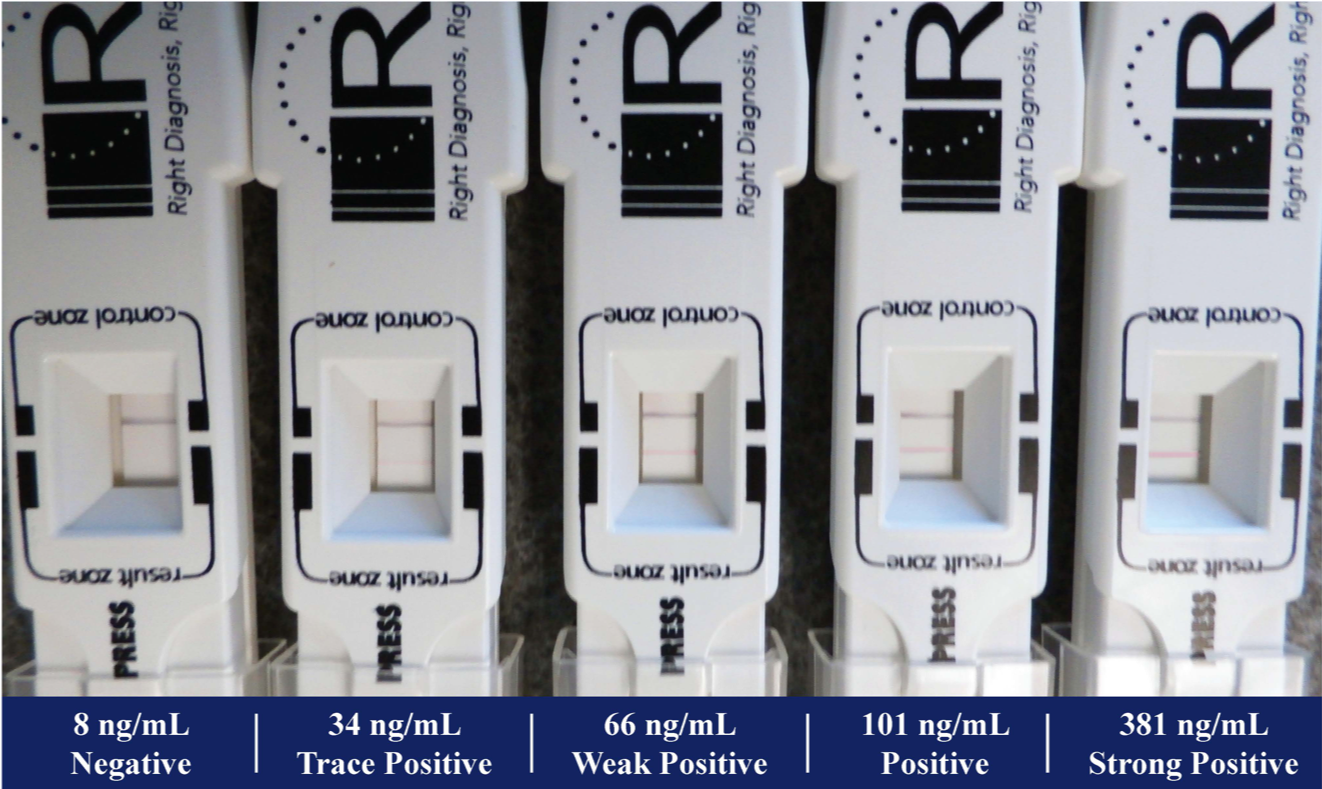
Figure 2 - Grading scale
With an advanced understanding of the ocular surface and inflammation levels, ODs can optimize the management of patients’ clinical outcomes and promote wellness of the ocular surface.
The views expressed here belong to the authors. They do not necessarily represent the views of Optometry Times or MJH Life Sciences.
Optometrists understand the importance of inflammation in medicine, respect its severity, and try to avoid it because of the potential long-term deleterious implications to human tissue. When someone has an autoimmune condition, ODs understand the potential long-term implications to his health.
Often, attempts at reducing inflammation with a rheumatologist’s close management is critical in long-term tissue damage of the affected organ. Additionally, patients are often placed on chronic medications in attempts to control inflammation. Ironically, some of these medications are known to have potential sight-threatening consequences.
Related: Understand the science and art of managing chronic conditions
Chronic inflammation
Chronic inflammation in long term systemic diseases is respected and treated accordingly.
In eye care, there is a growing body of evidence that shows the link between Ocular Surface Disease (OSD) and chronic inflammation. The Tear Film and Ocular Surface Society (TFOS) Dry Eye Workshop II (DEWS) report defines dry eye as the following: “Dry eye is a multi-factorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface in-flammation and damage, and neurosen¬sory abnormalities play etiological roles.”1
Loss of homeostasis
In the DEWS II new definition of Dry eye, there is the notable addition of the phrase, “loss of homeostasis” which re-calibrates the way ODs clinically think of dry eye. Clinically, dry eye used to be thought of simply as the absence of adequate tear production. Traditional wisdom would encourage lubrication to the ocular surface with the addition of an artificial tears or an attempt is made to retain tears on the eye through punctal occlusion. As opposed to thinking about dry eye as simply a reduced level of tear production, we now view it as a loss of homeostasis.
Related: Remember the basics as dry eye treatments expand
Homeostasis on the ocular surface demonstrates an intricate relationship between all of the components of the ocular surface. In a normal individual, this relationship produces a consistent comfortable visual experience. Homeostasis is a critical concept that challenges the clinician to think differently about how the surface of the eye functions. A patient who complains about dry eye is no longer diagnosed with a simple lack of tear production but rather a disruption of the homeostatic balance on the ocular surface.
Related: New guidelines in OSD evaluation before surgery
Clinically, as ODs examine the ocular surface through both physical inspection and the incorporation of advanced diagnostics, the clinician’s interpretation of the homeostatic disruption is what determines a treatment path. Often, we attempt to treat the cause that is most disruptive to tear film homeostasis. Integral to this is understanding inflammation.
Measuring inflammation
Until relatively recently, ODs didn’t have the ability to measure inflammation levels on the surface of the eye. Instead, physical findings were used to reach conclusions about inflammation.
Today, there is a point-of-care test that measures levels of matrix metalloproteinase-9 (MMP-9) on the surface of the eye. MMP-9 is a diffuse, non-specific inflammatory marker that is critical to monitor in patients who have dry eye disease.
InflammaDry (Quidel) determines whether there is greater than 40ng/mL of MMP-9 in the tear film. If the test is positive, there is greater than 40ng/mL in the tear film. If the test is negative, there is less than 40ng/mL in the tear film.
Related: Treat dry eye disease first, address comfort next
From the onset, experiences with InflammaDry made ODs realize that positive responses varied in intensity level. Some patients who tested positive had a bright, strong signal show up. Other patients tested positive, but signal strength was very weak (Figure 1).
After discussion with the company, ODs realized that the response was dependent on concentration and that the test provided much more information than simple MMP-9 levels. ODs also thought it was important to better quantitate the level of inflammation through in such a test.
Related: Don’t shy away from steroid use for surgery patients
Solutions to MMP-9 shortcomings
Four years ago, presented a poster at a major optometry meeting to propose a new grading scale for the utilization of this point-of care-test.2 By using various concentrations of diluted MMP-9 solutions and testing them, we were able to put together a scale that helps quantify the test to a greater level, helping improve its diagnostic capabilities.
Five different concentrations of MMP-9 in vials were tested: 8 nanograms per milliliter (ng/mL), 34 ng/mL, 66 ng/mL, 101 ng/mL, 381 ng/mL. Each test produced different signal strengths. We labelled them from weakest to strongest signal strength, respectively, with the following classifications: negative, trace positive, weak positive, positive, strong positive. (Figure 2)
Related: Novel drugs + delivery systems ease ocular pain and inflammation
When ODs understand the level of MMP-9 on the ocular surface, it helps them to formulate an appropriate dry eye treatment plan. ODs understand that chronic inflammation will erode the integrity of tissue over time. For this reason, inflammation levels on the surface of the eye are monitored at baseline and tracked during treatment.
With evolving technologies, point-of-care technologies and advancing treatment options, it is critical to be aware of inflammation levels on the eyes to set appropriate treatment protocols. Additionally, it is critical to understand the influence of treatments on inflammation levels. With an advanced understanding of the ocular surface and inflammation levels, ODs can optimize the management of patients’ clinical outcomes and promote wellness of the ocular surface.
More by Dave and Mile: 4 uses for OCT in OD practices
References:
1. Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo CK, Liu Z, Nelson JD, Nichols JJ, Tsubota K, Stapleton F. TFOS DEWS II Definition and Classification Report. Ocul Surf. 2017 Jul;15(3):276-283.
2. Brujic M, Kading DL. Making matrix metalloproteinase-9 levels more meaningful. Poster presented at Global Specialty Lens Symposium annual meeting; January 21-24, 2016; Las Vegas, NV.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.