How to address the three aspects of dry eye disease

Jerry Robben, OD, is chief optometric physician and director of clinical research Jacksonville, FL

Follow one doctor’s treatment protocol to addess inflammation, breakdown of the ocular surface, and obstruction to the meibomian glands in treating dry eye patients.
As ODs understand more about dry eye disease (DED), we are finding out that it is more prevalent and complex than previously thought.
A German populations-based study found the incidence of dry eye disease to be over 50 percent,1 and U.S.-based studies show a notable increase among those aged 18 to 34 years.2,3 Younger people are affected as modern, computer-centric lifestyles exacerbate the condition4 and damage the meibomian glands, ocular surface and lacrimal function unit (LFU) as a whole.
In order to combat this increasingly prevalent condition, a more proactive approach is necessary.
In my experience, ODs need to approach dry eye care as dentists approach oral hygiene. Dental care used to be reactionary rather than preventative. It wasn’t until the 1950s and 1960s that researchers demonstrated that fluoride and preventative oral care could eliminate microbial pathogens, resulting in fewer edentulous people and millions less spent on dental care.5,6
As a result of this understanding, we no longer wait until we have a cavity to start brushing and flossing our teeth.
Related: Dry eye protocol for any practice
Eye care should be no different. In my experience, whether or not symptoms are present, proactive eye care can help keep the ocular surface healthy and prevent, or at least slow, future problems. For that reason, I initiate a basic dry eye regimen with every patient that I see-even for those whom I may not diagnose with dry eye disease.
Establishing good habits
In my office, every patient starts his exam with a Standardized Patient Evaluation of Eye Dryness (SPEED) questionnaire to assess his symptoms.
If the SPEED is positive for symptoms, then further dry eye evaluation is performed and medical treatment is initiated. If the patient has no symptoms and no dry eye findings upon examination, he is still started on a preventative regimen.
In my practice, a basic eye care regimen includes HydroEye (ScienceBased Health), Eye-eco (Eye-eco) eyelid scrub, and Oasis Tears (Oasis Medical) lubrication drops. Thermal therapy with warm compresses using a heat mask (Bruder or Eye-eco Dry Eye Relief [DERM] mask is also recommended for eight to 10 minutes twice per day).
Just as the most diligent flosser may still develop cavities even with proactive dental hygiene, dry eye problems may still occur for those who are using preventative treatment. However, I have found that the incidence will be lower, disease severity will be lower, and patients will have established good habits which will extend to treating any pathology that may arise.
Thorough approach to pathology
Any patient with a SPEED score of 1 or higher is further evaluated for DED, with the results of the questionnaire guiding the diagnostic testing options.
For instance, if a patient responds positively to a question geared toward ocular allergies, we know to perform a test specific to allergies in addition to our standard dry eye testing battery.
Another area of the questionnaire steers us toward possible autoimmune problems and determines if the patient should be tested for Sjögren’s disease.
Our standard battery of diagnostics include:
• Evaluation of tear osmolarity
• Lipid layer thickness
• Blink pattern analysis
• Meibomian gland evaluation
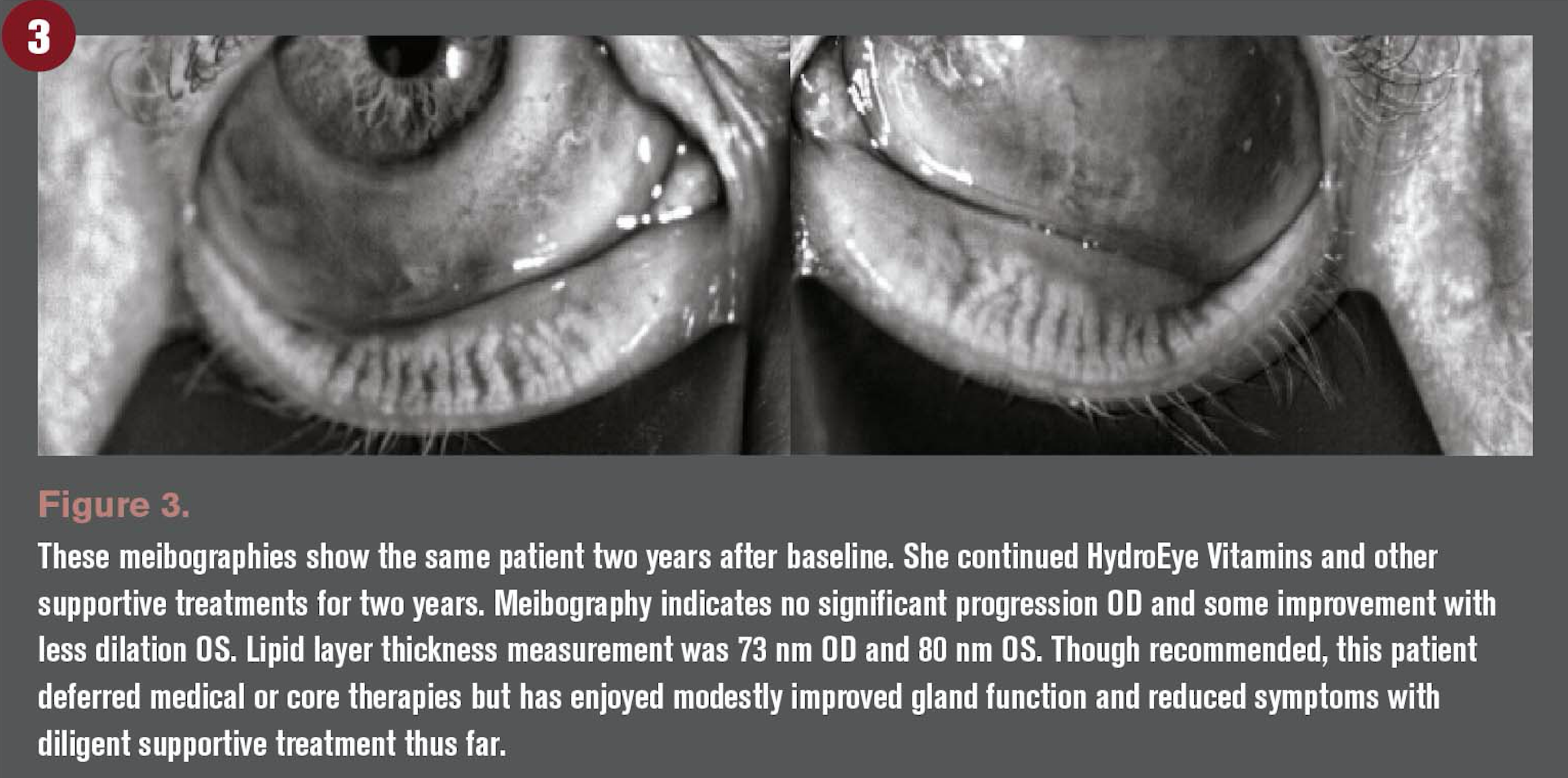
• Meibography
• Ocular surface scatter
• MMP-9 inflammatory marker
The use of a meibomian gland evaluator helps to examine the glands and determine abnormalities in their function or full obstruction at the slit lamp. This evaluation is performed independent of the patient experiencing symptoms.
Related: New cyclosporine therapy joins fight against dry eye disease
DED is multifactorial, it can have a variety of causes, and it is easy to get lost in the weeds when treating it. I focus on three specific goals to keep DED in check:
1. Treat the inflammation
2. Address the ocular surface breakdown
3. Address any obstruction to the Meibomian glands
1. Treat the inflammation
ODs have multiple means of treating inflammation in DED, and in my experience it is best to start with overall nutrition.
I recommend HydroEye to all patients, not just those who test positive for MMP-9. It is the basis upon which I build my DED treatment regimen. It has a combination of gamma-linolenic acid (GLA), omega-6 fatty acid to help combat dry eye,7 and omega-3s eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
The combination of GLA with EPA suppresses pro-inflammatory mediators as well as stimulates anti-inflammatory production.7-9
In conjunction with HydroEye, I may prescribe an immunomodulator such as Restasis (cyclosporine, Allergan) or Xiidra (lifitigrast, Shire) depending on the individual patient. In my experience, Xiidra provides results quicker with an effective and direct proposed mechanism of action, but Restasis has a broader proposed mechanism of action that is appealing in the long term.
In either case, if patient is seeking any ocular surgery in the short term or has significant inflammation and/or symptoms, I may prescribe Restasis or Xiidra plus a corticosteroid. These determinations are made on a case-by-case basis. If the patient’s medical insurance does not cover Xiidra or Restasis, I may opt for Klarity-C (cyclosporine, Imprimis). Remember that Cequa is newly approved from Sun Pharma and will soon be available for use in this class.
Related: Know the four stages of dry eye blepharitis syndrome
2. Address ocular surface breakdown
If the patient’s blink rate is not frequent or complete to maintain a smooth, continuous layer of tear film over the cornea, the ocular surface can be exposed to the point of increased evaporative stress and later breakdown and injury.
Providing something to protect and soothe the ocular surface until inflammation is reduced and the lacrimal functional unit (LFU) is working properly is important for patient comfort and preventing further corneal damage.
For a patient with DED, I will prescribe a different lubricant than what I recommend for preventative care. Options include Oasis Plus (Oasis Medical), Retaine MGD (OcuSoft), or a combination of the two. In more severe cases, I will add an ointment, such as Retain PM (OcuSoft).
For patients with a significantly damaged corneal surface, I recommend use of amniotic membrane application and autologous serum eye drops sooner rather than later. For amniotic membrane, I have found that cryopreserved Prokera (Bio-Tissue) is the best option for that patient’s surface. With proper patient education and observation, tolerance for this device is not a concern. I use Vital Tears (Vital Tears) autologous serum drops, which has made access to these drops for the patients much easier then in the past.
Related: The changing dry eye dynamic
3. Clear meibomian glands
Meibomian glands play an essential role in keeping the tears stable and the ocular surface clean, healthy, and well-lubricated. ODs know that gland dysfunction causes dry eye for many patients. We also know that the glands can be affected and disrupted for many reasons. No matter the cause of MGD, it decreases the quality and quantity of gland secretions, which can progress and become permanent. Other treatments cannot be effective in the long term if the meibomian glands are not appropriately treated.
Gland therapy in my office begins with clearing the glands of any obstructions and maintaining their proper function. I begin with LipiFlow (TearScience) thermal pulsation treatment. Some patients may have significant obstruction that may not respond to Lipiflow alone. For these patients, we perform distal meibomian gland probing just prior to Lipiflow treatment.
I supplement these therapies with heated meibomian expression with the iLux device (Tearfilm Innovations) every four to six months after Lipiflow. I also treat the biofilm by performing Blephex (Rysurg) on the lids to eliminate scurf and bacterial biofilm to improve the overall health of the lid margin and prolong the effects from the thermal pulsation. Blephex is preformed prior to Lipiflow and thereafter at four- to six-month intervals with the iLux.
These treatments will likely need to be repeated at times throughout the course of the patient’s life. Some like Blephex and iLux will need to be performed more frequently than Lipiflow and gland probing.
The patient may also need to upgrade her home lid cleansing routine from the basic regimen. For this I take a case-by-case approach. I recommend Ocusoft Lid Scrub (OCuSOFT) if I see a staph-bleph presentation, Cliradex Eyelid Wipes (Bio-Tissue) if demodex is present, and Avenova (Novabay) if a patient demonstrates rosacea without demodex or if she is presurgical.
Additionally, nearly every patient may benefit from one of the newest treatment options in our dry eye arsenal, TrueTear (Allergan). I have been using it personally for about 18 months and with my patients. It is a great tool to help enhance a patient’s control of his dry eye disease.
TrueTear is an FDA-approved intranasal stimulator that utilizes neurostimulation to activate the LFU on demand. This activation naturally stimulates the lacrimal gland, goblet cells, and meibomian glands to produce their contribution to the tear film in unison instantly. This technology is being used as an adjunctive option to better help dry eye patients.
Patient education
For these treatments to be successful, the patient must be compliant. Education plays a significant role in this, and educating patients can be time consuming and complex.
To relieve the doctor of the education burden, staff helps the effort in my practice. Receptionists, technicians, doctors, and counselors are fully educated on the disease, treatments, and practice philosophy toward providing patients with the best outcomes. All staffers who come in contact with the patient will reinforce our treatment approach.
In addition, patients who score 1 or higher on the SPEED questionnaire, or who are undergoing dry eye treatment, meet with a dry eye counselor prior to seeing the doctor at each visit. The counselor will review diagnostic results with the patient, explain anything he does not understand, review the treatment recommended by the doctor, and educate the patient in detail on dry eye disease. The patient will return to the counselor after seeing the doctor to reinforce treatment plans, answer follow-up questions, and schedule needed interventions.
The diagnostics we use play an important role in education because they identify the severity of the disease and track its progress or improvement in a way that is visible to the patient. Plus, counselors show patients interactive educational videos to explain DED and the importance of treatment compliance. Currently, we show educational videos from Rendia on a tablet.
Dry eye is a serious condition and should be treated as one. Our proactive approach requires not only investment in advanced tools and equipment but also in staff training and patient education.
While such a protocol may be daunting to some doctors, I imagine that it also seemed daunting to teach the public to brush and floss daily, to visit the dentist twice yearly for exams and cleanings, or to add fluoride to public water systems a half century ago.
But with a unified effort and persistence in knowing what was best, the dental community and its patients now enjoy more successful dental outcomes. Eyecare providers need to have the same conviction and persistence with dry eye disease.
Click here to read more articles about dry eye
References:
1. Erb C, Gast U, Schremmer D. German register for glaucoma patients with dry eye. I. Basic outcome with respect to dry eye. Graefes Arch Clin Exp Ophthalmol. 2008 Nov;246(11):1593-601.
2. Farrand KF, Fridman M, Stillman IO, Schaumberg DA. Prevalence of Diagnosed Dry Eye Disease in the United States Among Adults Aged 18 and Older. Am J Ophthalmol. 2017 Oct;182:90-98.
3. Gupta PK, Stevens MN, Kashyap N, Priestly Y. Prevalence of Meibomian Gland Atrophy in a Pediatric Population. Cornea. 2018 Apr; 37(4):426-430.
4. Schlote T, Kadner G, Frudenthaler N. Marked reduction and distinct pattern of eye blinking in patients with moderately dry eyes during video display terminal use. Graefes Arch Clin Exp Ophthalmol. 2004 Apr;242(4):306-312.
5. White BA, Caplan DJ, Weintraub JA. A quarter century of changes in oral health in the United States. J Dent Educ. 1995 Jan;59(1):19-57.
6. Axelsson P, Nyström B, Lindhe J. The long-term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance. J Clin Periodontol. 2004 Sep;31(9):749-57.
7. Barabino S, Rolando M, Camicione P, Ravera G, Zanardi S, Giuffrida S, Calabria G. Systemic linoleic and gamma-linolenic acid therapy in dry eye syndrome with an inflammatory component. Cornea. 2003 Mar;22(2):97-101.
8. Barham JB, Edens MB, Fonteh AN, et al. Addition of eicosapentaenoic acid to gamma-linolenic acid-supplemented diets prevents serum arachidonic acid accumulation in humans. J Nutr. 2000 Aug;130(8):1925-31.
9. Viau S, Leclère L, Buteau B, Grégoire S, Acar N, Bron A, Creuzot-Garcher CP, Bretillon L, Joffre C. Polyunsaturated fatty acids induce modification in the lipid composition and the prostaglandin production of the conjunctival epithelium cells. Graefes Arch Clin Exp Ophthalmol. 2012 Feb;250(2):211-22
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.