How alcohol consumption correlates with glaucoma
With the advent of electronic health records, it is now easier than ever to keep up with what medications a patient is actually taking, and (especially in the arena of glaucoma) the several classes of medications, such as steroids, beta blockers, and antihistamines, that can influence how patients’ eyes behave. With this in mind, I had a patient come in the other day with an interesting question regarding her intraocular pressure (IOP).

With the advent of electronic health records, it is now easier than ever to keep up with what medications a patient is actually taking, and (especially in the arena of glaucoma) the several classes of medications, such as steroids, beta blockers, and antihistamines, that can influence how patients’ eyes behave. With this in mind, I had a patient come in the other day with an interesting question regarding her intraocular pressure (IOP).
More glaucoma: Know your glaucoma surgery for better comanagement
She is a 74-year-old African-American female with a longstanding history of bilateral primary open-angle glaucoma (POAG). She has been stable for several years now and uses a prostaglandin analog in each eye at bedtime. Her medical history is remarkable for hypothyroidism, systemic hypertension, and hypercholesterolemia-all of which are all reportedly under good control. Her systemic medications include Synthroid (levothyroxine, AbbVie), lisinopril (Prinivil, Merck)/hydrochlorothiazide (Microzide, Watson Laboratories), and simvastatin (Zocor, Merck). She also supplements with fish oil daily in the form of a pill.
She presented for a three-month IOP check with entering best-corrected visual acuities of 20/20 in each eye. Pupils were normal, as were the anterior segments. Intraocular pressures by means of Goldmann applanation tonometry were 13 mm Hg in the right eye and 15 mm Hg in the left eye at 2:45 p.m. Undilated optic nerve evaluation by means of pre-corneal lens revealed no Drance hemorrhages. After asking her if she needed any refills of her drops and recommending she schedule another three-month follow-up appointment, she asked me an interesting question.
More from Dr. Casella: Why retinal vasculature could aid glaucoma diagnosis
“Let me ask you something,” she said. “My girlfriends and I play bridge and drink on Saturdays. Is that going to affect my eye pressure?” I asked her how much she drank, and she said, “Just a little gin while we play.”
Next: Glaucoma and alcohol
Glaucoma and alcohol
Several things went through my head, one of which was the somewhat jaded truth that “just a little bit” can mean many things, including “a lot.” However, I appreciated the question, and after the fact I was compelled to research the topic.
As it turns out, ethyl alcohol (ethanol) has been known for decades to be a hyperosmotic molecule (albeit in the short term). However, ethanol consumption may have a propensity to raise IOP after chronic use. The implication is that it may reduce IOP in the short term (perhaps just a couple of hours or so) but possibly have a negative impact in the long term. I was unable to find any compelling evidence showing alcohol consumption as having a direct and causatively negative impact on glaucoma. Therefore, drinking alcohol has not been clearly demonstrated as being a risk factor for the development of glaucoma.
More glaucoma: Understanding drainage in glaucoma surgery
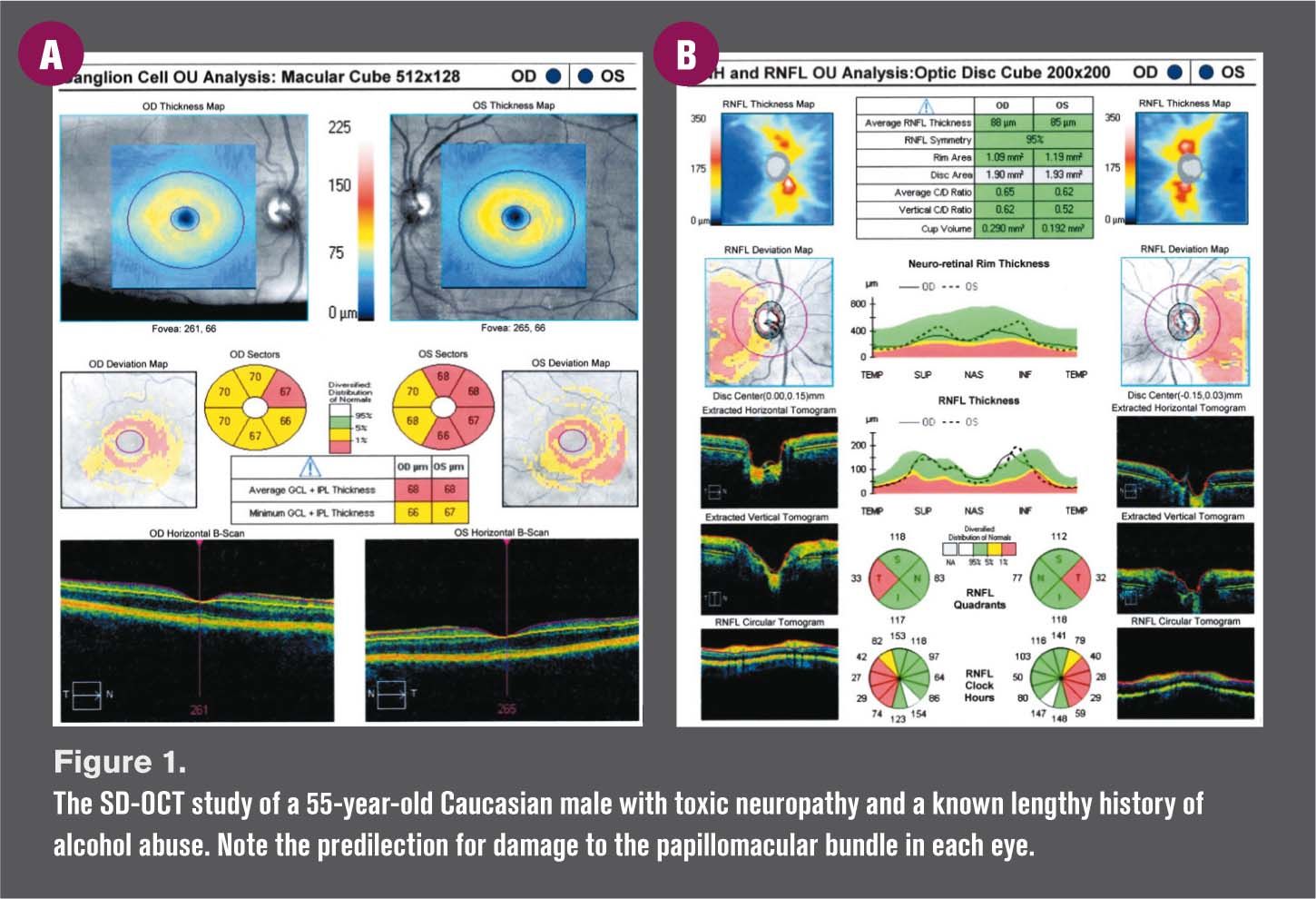
That being said, glaucoma is just one optic neuropathy (in addition to another on the list of optic neuropathies: toxic optic neuropathy, which alcohol over-consumption is known to cause). Figure 1 is the spectral domain optical coherence tomography (SD-OCT) ganglion cell analysis and corresponding retinal nerve fiber layer analysis of a 55-year-old Caucasian male with toxic optic neuropathy and a known lengthy history of alcohol abuse. The patient died several years later of complications related to liver failure.
Sharing good information
Systemically, there is a great deal of information readily available to the public regarding differing opinions of what levels of alcohol consumption are considered “safe” for adult males and females. However, the Centers for Disease Control and Prevention (CDC) has what I consider to be an excellent, comprehensive, and definitive website devoted to alcohol consumption and health and welfare: http://www.cdc.gov/alcohol.
Related: Managing glaucoma in women
Getting back to my patient and her seemingly pointed question, I answered as practically as I knew how and simply said, “Well, alcohol consumption technically does slowly poison us, but that being said, your glaucoma has been behaving ever since I’ve been treating you. So, just don’t overdo it and your eyes should be fine.”
We, as optometrists, are fiduciaries and have an obligation to inform our patients appropriately. Sometimes that can mean quoting studies, and sometimes that can mean simply extending the notion of good common sense.