ODs’ guide to MRIs
Know the types of magnetic resonance imaging and how to order them.
The eyes are the outer extension of the human body’s nervous system. As the frontline primary eyecare provider, optometrists must have a clear understanding of the neurology that affects the visual system and neuroimaging that can help diagnose specific pathology.
Optometrists daily diagnose vision and by extension brain and neurologic problems.
Common clinical findings can present as symptoms of serious medical problems:¹
• Optic nerve swelling
• Visual field defects
• Vision loss
• Pupil problems
• Diplopia
• Ptosis
• Proptosis
• Ophthalmoplegia
Imaging
Many different types of neuroimaging are safe imaging techniques to indicate problems within the human brain, including:²
• X-ray
• Computed tomography (CT)
• Magnetic resonance imaging (MRI)
• Functional MRI (fMRI)
• Positron emission tomography (PET)
• Electroencephalography (EEG)
• Magnetoencephalography (MEG)
• Near infrared spectroscopy (NIRS)
• Magnetic resonance angiography (MRA)
• Digital subtraction angiography (DSA)
This article will focus specifically on MRI modality, review what it does, how it is applicable, and how to order this test.
MRI
The MRI is the study of choice for tumor, multiple sclerosis, and ischemic stroke.
With the addition of gadolinium, evaluation of tumors such as meningioma, inflammation, and infection can be visualized. This is due to providing valuable imaging of orbital soft tissues and the brain.
The MRI uses strong magnetic fields, magnetic field gradients, and radio waves to generate images of organs in the body. This is accomplished by atomic nuclei absorbing and emitting radio frequency when placed in an external magnetic field.
Related: Know the benefits of adopting neuroimaging
Most MRI machines use protons (hydrogen atoms), which are abundant in water and fat. Radio waves excite the nuclear spin energy transition, and the magnetic field gradients localize the signal in space. As the hydrogen atoms pulse and relax, contrasts are generated between the properties of different tissues.³
MRI does not involve X-rays or the use of ionizing radiation, giving a better safety profile than CT or PET scan technology.³
A contraindication of MRI is patients with magnetic metallic items from previous surgeries such as pacemakers, defibrillators, cochlear implants, and other medical devices. If these are known or suspected, it is very important to consult with the radiologist and other health professionals to ensure patient safety.
Viewing MRI images
When viewing an MRI image, it is important to understand where in space the patient is in respect to the direction of magnetic field.
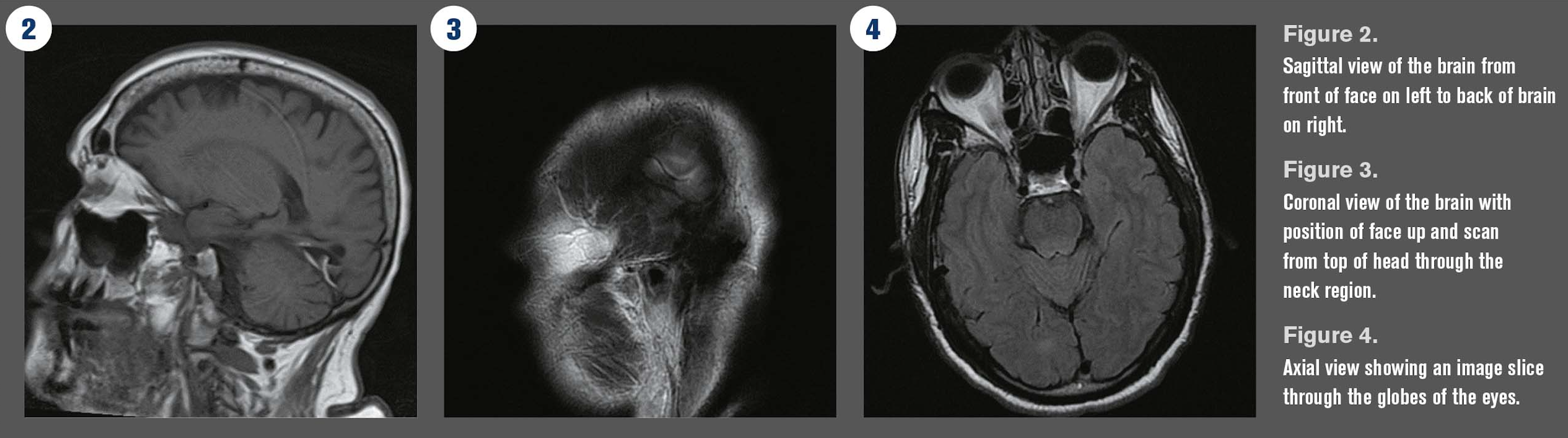
MRI consists of three common image scans; they are displayed as: sagittal, coronal, and axial (see Figure 1).
A sagittal scan (see Figure 2) is often easiest to interpret due to the clear anatomical picture of seeing the head from the nose to the back of the skull. Sagittal scans are side or profile views of the body or brain. The image looks as if the patient has been sliced vertically, from head to the back of the skull.
A coronal scan (see Figure 3) shows a head-on view of the body. The image shows the patient’s features vertically from the front as if the patient were standing facing the camera.
An axial scan (see Figure 4) is viewed as thin slices of the brain from the top down. A visualization of this is horizontal slices from the head to the toes.³
Read the latest by James F. Hill III: How to diagnose an optic nerve
Weighted images
MRI scans are further differentiated into different weighted images. The two most common sequences used for brain imaging are T-1 weighted and T-2 weighted sequences.
A T-1 weighted scan represents the time it takes tissue to recover from a radiofrequency pulse. In a T-1 image, fluid is extremely dark, water-based tissue is gray, and lipid-based tissues are bright.
These images are useful for brain parenchyma in which the brain appears medium gray, the cerebrospinal fluid (CSF) is dark gray, and water looks nearly black. Most tumors appear dark with low signal intensity. Sensitivity helps to view images, depending on scan protocol-tissue images as white (high signal intensity), as gray (intermediate intensity), and dark gray or black (low signal intensity).â´
A T-2 weighted scan represents the time the signal lasts after giving a radiofrequency pulse. This type of scan uses a gradient echo (GRE) sequence, which can help with suspected intracranial microhemorrhage.
These images provide contrast between gray and white matter in the brain. They also provide clarity of the CSF spaces, which appear bright white, and brain tissue appears light gray.
T-2 images also show a bright signal around the myelin sheath in the white matter, which is characteristic of multiple sclerosis.âµ
Ordering MRI
ODs need to answer three questions in ordering MRI for their patients.
1. How and what do you need to let the radiologist know?
2. Where do you send the patient?
3. What action do you take when you receive the results or interpretation?
One important point to note is that if you order the MRI, you are responsible for what it reveals.
Ordering neuroimaging is not unlike ordering any other diagnostic testing for a patient in the office setting. The optometrist should clearly state the reason for the testing and document it well in the chart.
Most radiologists welcome suggestions and comments for the reason the MRI order. If the OD suspects optic nerve swelling, homonymous hemianopia, or diplopia from a CN3 palsy, add that to the order.
When in doubt, consider a scan with and without contrast. A contrast series is generally combined with a T1 weighted image because pathology is often associated with fluid. Gadolinium is often used; it has paramagnetic properties and reduces the T-1 relaxation time of the protons that absorb the potons, thus will have a higher signal intensity (more white image).
However, ask the patient about allergies to gadolinium, kidney problems, or medication excreted through the kidneys. If these risk factors are present, consult with the patient’s primary-care physician (PCP) and radiologist. Most likely, a combination of computated tomography (CT) and MRI without contrast will be ordered.
Obtaining MRI
Multiple centers perform MRI. These include large hospital systems, ambulatory surgery and imaging centers, and stand-alone neuroimaging locations.
In this my opinion, it is best to loop in the patient’s other health care providers (PCP, neurologist, neuro-ophthalmologist, or radiologist), if possible.
Not every patient will have a current PCP or have been seen in a subspecialty clinic; thus an OD can help facilitate these referrals. Optometry education, training, and clinical practice give ODs the knowledge and tools to understand the anatomy and pathology that affect the visual system. If pathology is suspected, ODs should feel confident in ordering an MRI to help determine the diagnosis and refer the patient to the appropriate provider for management.
It is important to understand that neuroimaging studies are read by radiologists who provide the impression and diagnosis, but what the OD as the ordering doctor does with that information is what is important. Remember, you as the OD are ordering the test and understand exam findings for your patient. In my clinical experience, a radiologist will welcome an OD’s impression of what might be wrong and what imaging may be best to order. Be confident with reasons to refer for testing, and frequenlty new provider-to-provider relationships can be established.
Optometrists with the suspicion of pathology and the ability to obtain testing should feel confident in doing so.
It is also important to understand the liability that comes with this privilege and the importance of following up and getting the patient the appropriate provider referral once the presumed diagnosis is made.
References:
1. Johnson M, Policeni B, Lee A, Smoker W. Neuroimaging in Ophthalmology. New York, NY: Oxford University Press; 2011.
2. Demetri M. Types of Brain Imaging Techniques. Psych Central. Available at: https://psychcentral.com/lib/types-of-brain-imaging-techniques/. Accessed 11/9/18.
3. Radue EW, Weigel M, Wiest R, Urbach H. Introduction to Magnetic Resonance Imaging for Neurologists. Continuum (Minneap Minn). 2016 Oct;22(5, Neuroimaging):1379-1398.
4. Verma R, Gupta M, Mehta V. Thyroid associated orbitopathy. BMJ Case Rep. 2013 Jun 3;2013. pii: bcr2013009920.
5. Daubner D, Spieth S, Engellandt K, von Kummer R. Diagnosis and differential diagnosis of Graves’ orbitopathy in MRI. Radiologe. 2012 Jun;52(6):550-9.