Blog: 4 uses for OCT in OD practices
The views expressed here belong to the author. They do not necessarily represent the views of Optometry Times or MultiMedia Healthcare.
When anterior segment
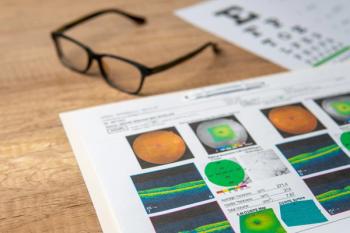
Over the last decade, ODs have learned how to maximize the use of OCT in clinical practice.
There are four commonly utilized reasons for anterior segment OCT.
Previously by Dr. Brujic and Dr. Kading:
Specialty contact lenses
Anterior segment OCT was initially developed to measure the anterior segment-not
Scleral lens fitting abides by a few rules: They need to be fit with the appropriate central corneal clearance, limbal clearance, and landing zone fitting the relationship.
ODs can measure the central corneal clearance along with limbal clearance. (Figures 1 and 2) This enables them to communicate more accurately with specialty lens laboratories and determine exact measurements and microns of clearance.
In our experience, this creates a more efficient fitting process and ultimately requires less lens adjustments to optimize the fit for the patient.
Keratoconus
Keratoconus is a condition traditionally monitored with topography to measure corneal curvature. With this condition, the cornea is steeper at the cone.
Anterior segment OCT technology monitors the condition by assessing the corneal thickness and at the thinnest region of the cornea, typically located in the region of the cone. This has become critically important for ODs because some vision plans require this measurement to determine the severity of the keratoconus.
Anterior segment OCT provides an additional metric to topographies to monitor disease progression over time.
Related:
Dry eye patients
One study looking at the epithelial thickness maps (ETM) of patients showed that individuals with dry eye had thickened ETM compared to those without dry eye.1
In a second study, researchers demonstrated a thinning of the ETM in the superior region of the cornea compared age-related normals.2
Although these studies may seem contradictory, they can be viewed as representing different phases of
We have noted this in our clinical experience as well. Those patients with earlier DED tend to have thickened ETM, while those who have had chronic dry eye for decades tend to have thinner ETM superiorly (Figure 3). We have also seen more variability in ETM in the dry eye patient than normal individuals.
This has become one of the new metrics to follow in dry eye patients. It is our goal to stabilize the ETM so there is less variability in the thickness of the ETM in those individuals with dry eye and to help avoid long-term thinning that can occur in some DED patients.
Related:
Post-refractive surgery patients
ETM has provided new insight and understanding into certain visual characteristics of post-
An interesting relationship was found between ETM and visual outcomes for patients. We determined that those individuals who experience more visual disturbance tend to have increased ETM. The total pachymetry readings of post-refractive surgery patients was predictably thinner centrally where the myopic ablation occurred.
But there is a variance in the ETM that exists in these patients, and we found a strong correlation between thicker ETM and more visual complaints. In normal individuals, the expected ETM is 50 to 59 µm. In some post-refractive surgery patients, we have seen ETM as high as 73 µm of epithelial thickness (Figure 4).
Related:
Other uses
Other conditions for anterior segment OCT include epithelial basement membrane dystrophy (EBMD), Fuch’s endothelial dystrophy, and narrow-angle glaucoma.
Viewing the anterior segment with higher diagnostic technologies gives ODs a greater insight into understanding the physiology of the anterior segment and helps illuminate the unexplained visual outcomes that our patients may have.
With more time and research, ODs will continue to increase their understanding of anterior segment OCT as it becomes an increasingly important part of clinical practices.
References:
1. Kanellopoulus AJ, Asimellis G. In vivo 3-dimensional corneal epithelial thickness mapping as an indicator of dry eye: preliminary clinical assessment. Am J Ophthalmol. 2014 Jan;157(1):63-68.
2. Cui X, Hong J, Wang F, Deng SX, Yang Y, Zhu X, Wu D, Zhao Y, Xu J. Assessment of corneal epithelial thickness in dry eye patients. Optom Vis Sci. 2014 Dec;91(12):1446-54.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.