Considering scleral lenses for astigmatic patients
We have witnessed a rise in clinical utilization of scleral lenses in recent years, and in some cases, their clinical indications have expanded to include even those patients with regular corneas. Given this sharp rise in scleral lens utilization, the principle of lens selection continuum as proposed by Visser et al appears to also hold true in patients with normal healthy eyes. Thus, when should clinicians reach for scleral lenses when providing care to patients with regular corneas?

A study at University Medical Center Utrecht assessed the performance of multiple lens modalities for a wide range of medical indications.1
This prospective cross-sectional study evaluated 281 existing contact lens patients fit with lenses based on a lens selection algorithm. Soft lenses and scleral lenses were two of the most commonly prescribed lens designs in this Netherlands study.
Surprisingly, despite the various corneal pathologies and conventional clinical wisdom, both soft and scleral lenses scored similarly in lens performance and patient satisfaction.
Visser et al determined that wearing contact lenses significantly improved corrected distance visual acuity and quality of life. Additionally, the authors went on to propose that scleral lenses are valid treatment choices after soft lenses fail to achieve desired visual rehabilitation in study patients.1
We have witnessed a rise in clinical utilization of scleral lenses in recent years, and in some cases, their clinical indications have expanded to include even those patients with regular corneas. Given this sharp rise in scleral lens utilization, the principle of lens selection continuum as proposed by Visser et al appears to also hold true in patients with normal healthy eyes. Thus, when should clinicians reach for scleral lenses when providing care to patients with regular corneas?
Looking at scleral lenses
Scleral lenses are large-diameter gas permeable (GP) contact lenses designed to vault over the cornea and rest on the scleral conjunctiva with minimal to absent pressure exerted along the corneal limbal region (Figure 1).
Subsequently, a scleral lens is able maintain a sizable fluid interface connecting the posterior optical zone to the corneal plane, which allows for neutralization of regular and irregular corneal astigmatism, and also provides therapeutic protection to the underlying ocular surface.
In recent years, owing to modern manufacturing processes and the availability of highly oxygen-transmissible lens materials, scleral lenses have further expanded their clinical indications. These lenses are now able to provide excellent vision and comfort for patients with corneas that are of normal, prolate profile with or without concomitant conditions like meibomian gland dysfunction, blepharitis, or dry eye.

It’s important for clinicians to keep in mind that many regular cornea patients also wish to achieve best visual function while remaining spectacle-free; however, dissatisfactions with frequent replacement soft contact lenses often lead to contact lens dropout.
Despite the advancing strides that have been made in frequent replacement soft spherical and soft toric contact lenses, numerous studies have demonstrated that contact lens dropout ranges from 15 to over 20 percent.2-6
The reasons for contact lens dropout are likely multifactorial because no single risk factor has been found to conclusively predict such a negative outcome. Nonetheless, the incidence of contact lens dropout has been observed to significantly increase as one enters the fifth decade of life.
It is easy to jump to the conclusion that emerging presbyopia may be the primary culprit limiting patient satisfaction at this stage of life; in actuality, vision and comfort have been reported as equal contributors for contact lens dropout after age 45.7
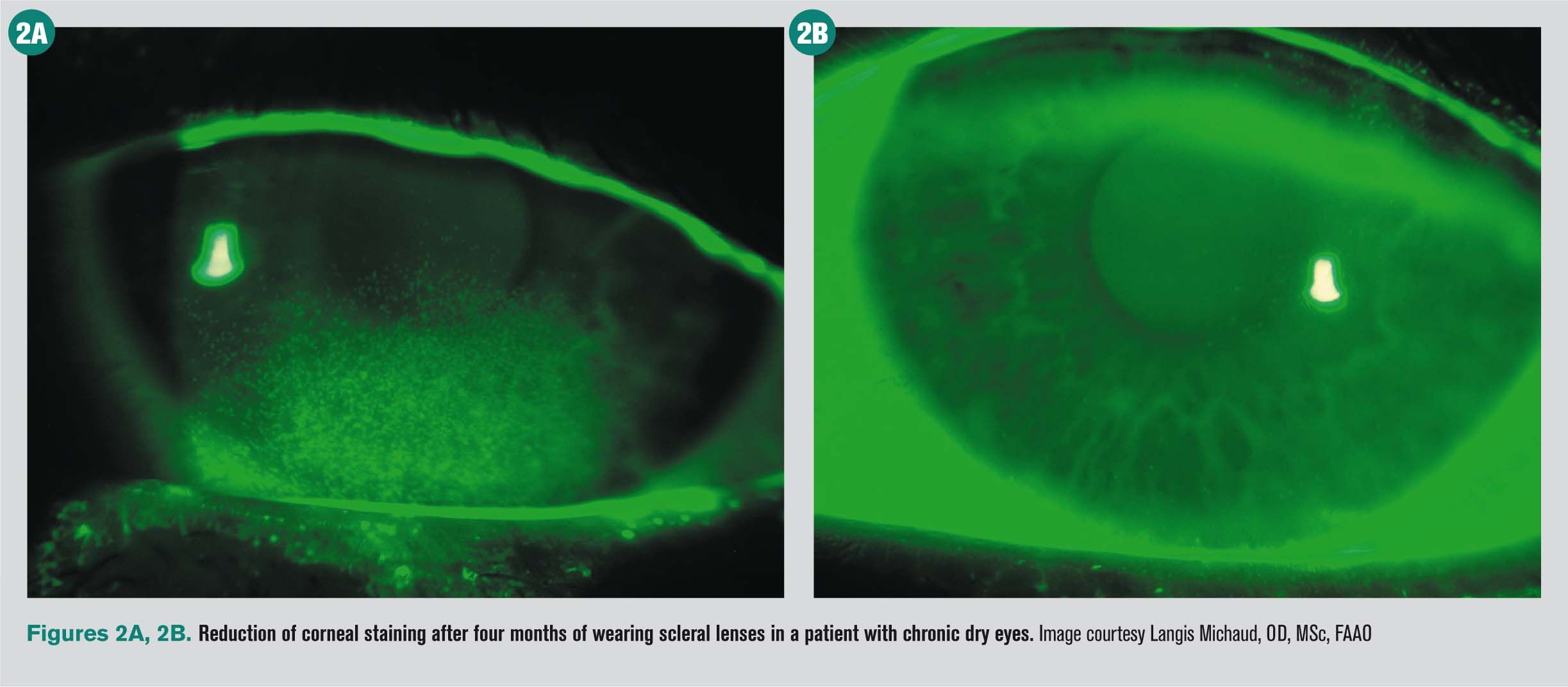
According to the Tear Film and Ocular Surface Society (TFOS), patients often begin experiencing physical awareness and/or visual disturbance. With increasing lens-related discomfort potentially exacerbated by extrinsic environmental factors, permanent discontinuation (or lens dropout) invariably becomes a reality for these patients (Figure 2A and 2B).8
Moving to scleral lenses
Given the optical advantage of corneal cylinder neutralization and therapeutic benefit of improved corneal surface hydration, scleral lenses can significantly improve the contact lens-wearing experiences for otherwise normal, healthy eyes-especially when these patients fail soft lenses or are considering dropping out of soft lenses altogether. Transitioning a patient from other contact lens modalities to scleral lenses is certainly attainable and may proactively prevent contact lens dropout.
Thus, a logical entry point to start considering scleral lens technology for a regular cornea patient can be when a patient wishes to remain in contact lenses but is dissatisfied with his current soft, soft toric, corneal GP, or hybrid contact lenses. Given the high prevalence rate in clinical utilization of soft contact lenses, the majority of patients reporting contact lens dissatisfaction who most clinicians will encounter are those who are currently wearing soft spherical or soft toric contact lenses.
Perhaps patients are finding their frequent replacement lenses are not as comfortable as desired, particularly at the end of the day, or maybe soft lenses do not provide the level of vision required throughout the entire wearing period.
Because soft toric lenses may become rotationally unstable with each blink, an astigmatic patient may complain of fluctuating vision throughout the day, even in the presence of a healthy lacrimal unit. In addition, similar visual challenges related to lens destabilization can occur when astigmatic patients assume a non-primary gaze position, especially during supero-nasal and infero-temporal excursions.9
Due to exceptional lens stability and crisp GP optics, scleral lenses are unmatched in their abilities to maintain clear and consistent vision all day long. This is particularly important for patients with high corneal astigmatism and/or those who participate in visually demanding athletic activities.
For many athletes, lens stability is essential, and scleral lenses are an excellent option. Unlike the majority of soft toric lenses or corneal GP lenses, scleral lenses tend to retain their physical and optical stability despite the rapidly changing ocular movements required while participating in athletic endeavors. Additionally, a large part of the ocular surface is shielded from foreign bodies during these demanding activities, such as dust or dirt exposure.
Generally, a spherical scleral lens can easily compensate up to 3.50 D of regular corneal astigmatism.10 In this case, the coupling of a larger optical zone with a spherical optical surface offers the clear and stable world that are sought after by patients. If residual astigmatism is detected, front toric optics can be incorporated to further deliver improved visual performance.
According to a study in a population of asymptomatic contact lens wearers, large diameter rigid gas permeable lenses can be a good alternative to soft toric lenses for the correction of refractive astigmatism.11
In addition to athletes and patients with high amounts of corneal astigmatism, another prime scleral lens candidate can be a patient who is intolerant of corneal GP lenses despite the absence of an irregular cornea. Patients who experience dry eyes, fluctuating vision, GP lens dislocation, or GP lens nonadaptation appreciate the comfort afforded by scleral lenses.
Whether the inability to adapt to GP lens wear is due to 3 o’clock and 9 o’clock staining secondary to lens rocking or simply corneal hypersensitivity, these fitting challenges are largely eliminated with scleral lenses. Moreover, the lid-lens edge interaction is drastically diminished after a scleral lens settles into conjunctival plane, which is one of the many reasons scleral lenses offer a more comfortable wearing experience.11
With proper patient motivation and good lens handling techniques, it can be easy to transition patients to scleral lenses to improve lens comfort, maintain crisp and clear vision, and avoid spontaneous lens dislodgement.
Fitting considerations
A regular cornea patient with relatively large mesopic pupils and/or corneal-based higher order aberrations that exceeds population average may be more likely to complain of glare and haloes with her conventional contact lenses. Such patients may include those who have occupations that require night driving such as truck drivers and healthcare workers with night shifts. Scleral lenses offer more flexible customization in their optical zone widths as compared to conventional frequent-replacement soft lens designs. Consequently, symptoms of haloes and glare are reduced, along with a corresponding improvement in night vision.
Allergies are increasingly prevalent and affect as many as 30 percent of adults and 40 percent of children.12 They are the fifth leading chronic condition in industrialized countries for all ages, and the third most common chronic disease in children under 18 years old.
Many patients, who are frequently young and active, want to use contact lenses for vision correction and to improve their quality of life.13 Currently, eye-related allergies and contact lens wear affect increasing populations worldwide.13
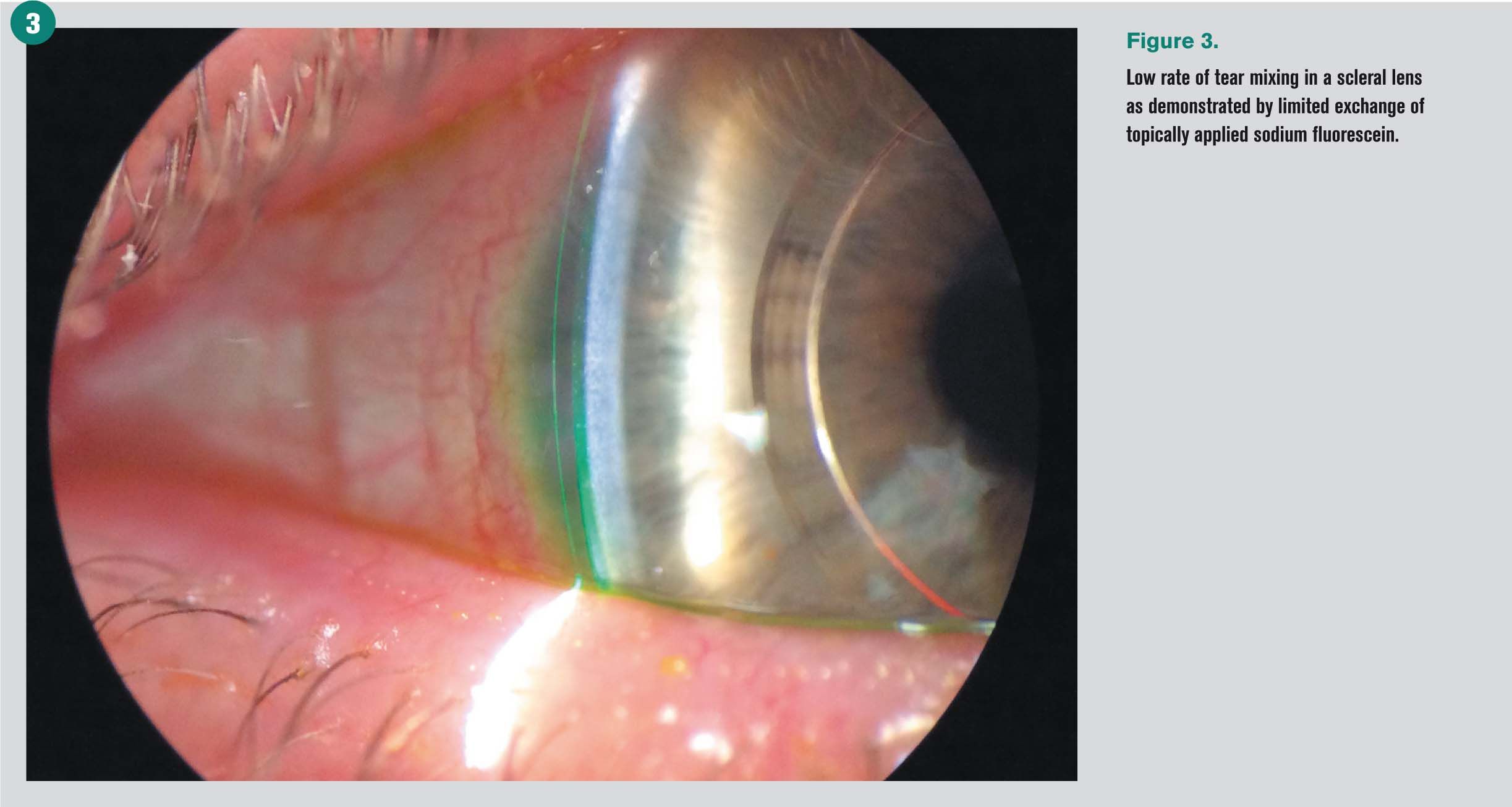
Scleral lens tear exchange is minimal after lens settling, which has been estimated at 0.2 percent per minute (Figure 3).14 The low rate of tear mixing can potentially reduce immunological and chemical mediators from entering a scleral lens, which may produce a prolonged period of comfortable wear on a daily basis during an allergy season.
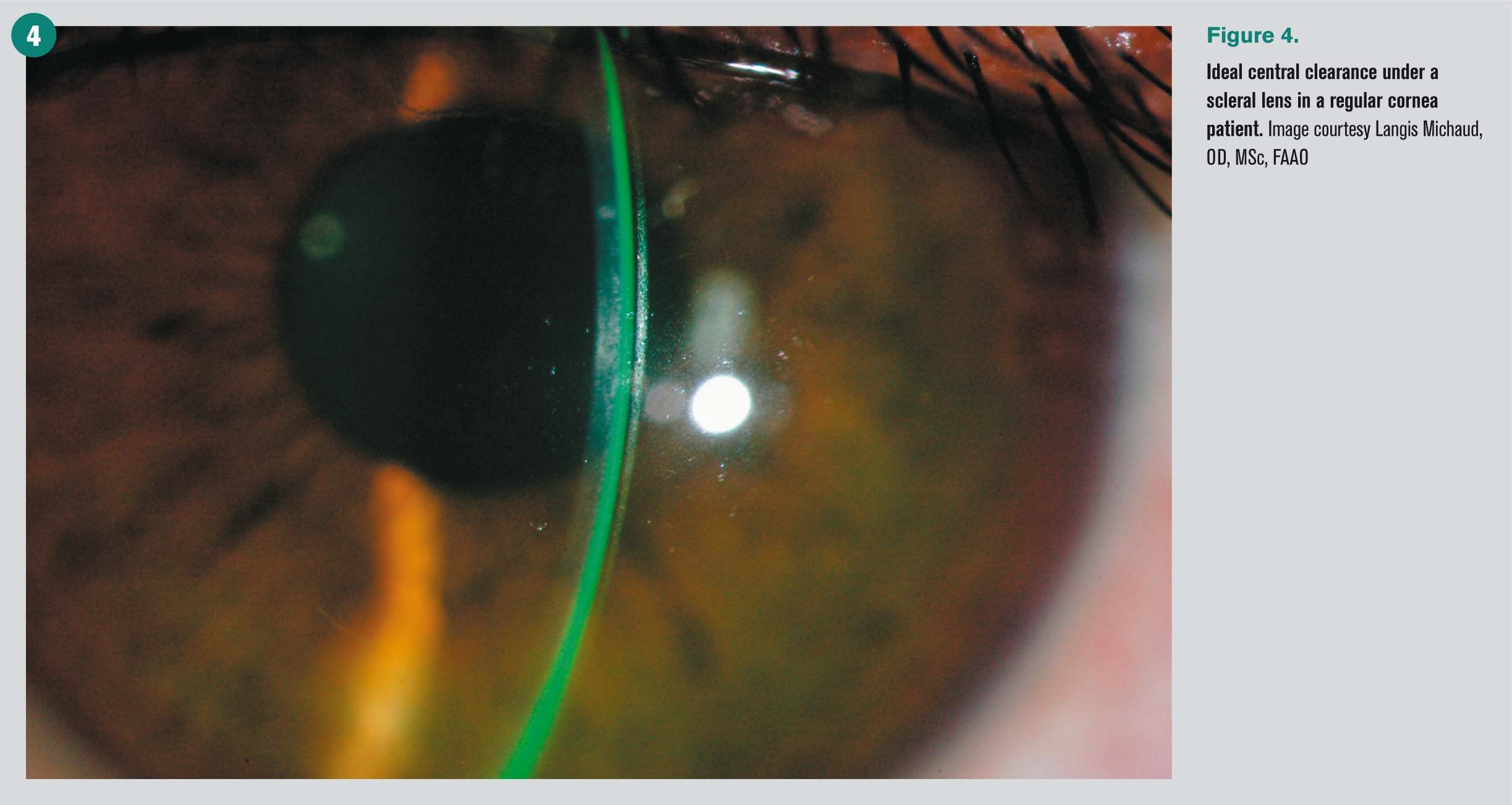
Conversely, the low tear exchange rate necessitates the selection of highly oxygen-permeable materials and a precise fitting algorithm to keep lens thickness and tear lens thickness as thin as possible,15 especially in healthy eyes (Figure 4).
A multicenter, prospective, cross-over study that compared patient satisfaction outcomes between a soft toric lens design and a large-diameter GP lens design found that patients subjectively report better acuity while using a computer and performing other near tasks when wearing prescribed large diameter GP lenses.11 Therefore, it is foreseeable that even a single vision scleral lens design may potentially help to defer the need for multifocal optics.
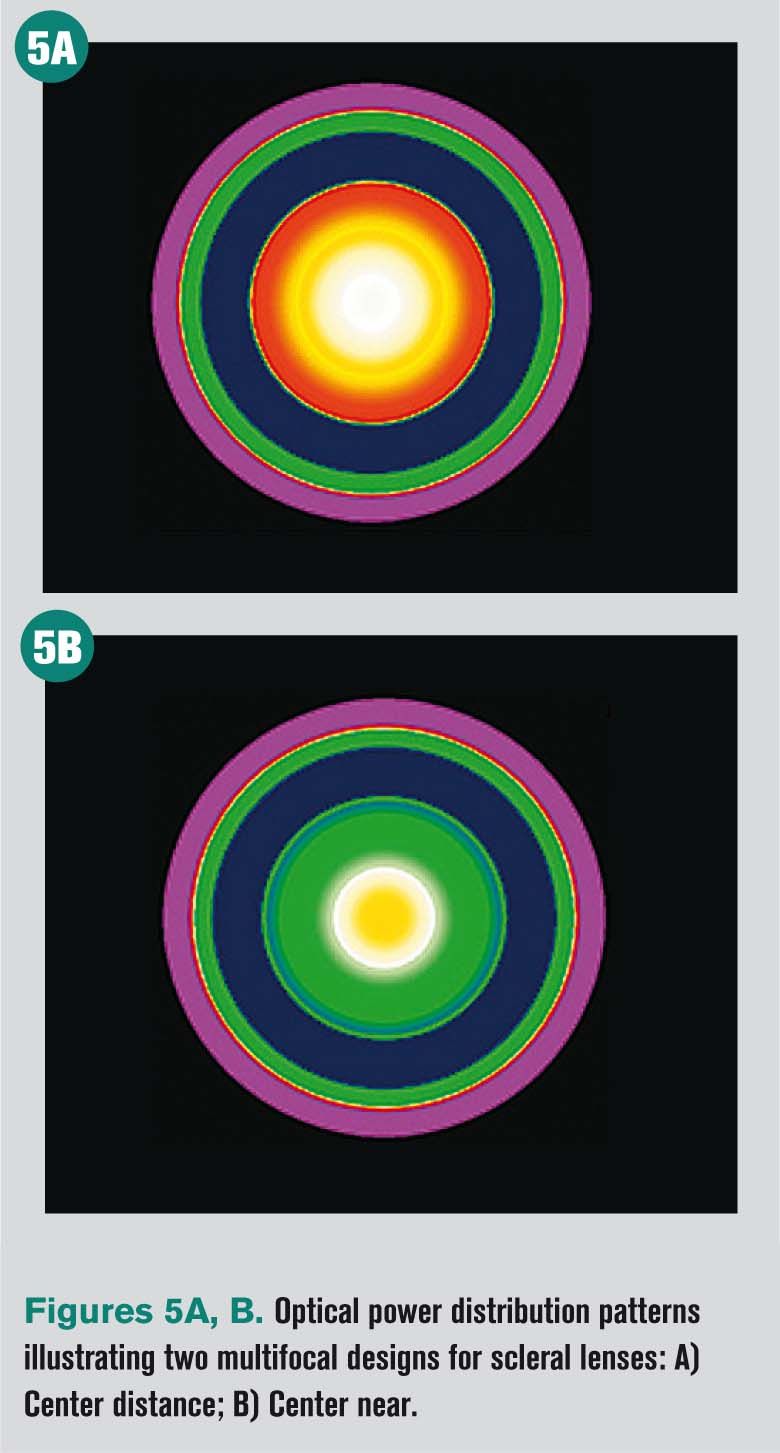
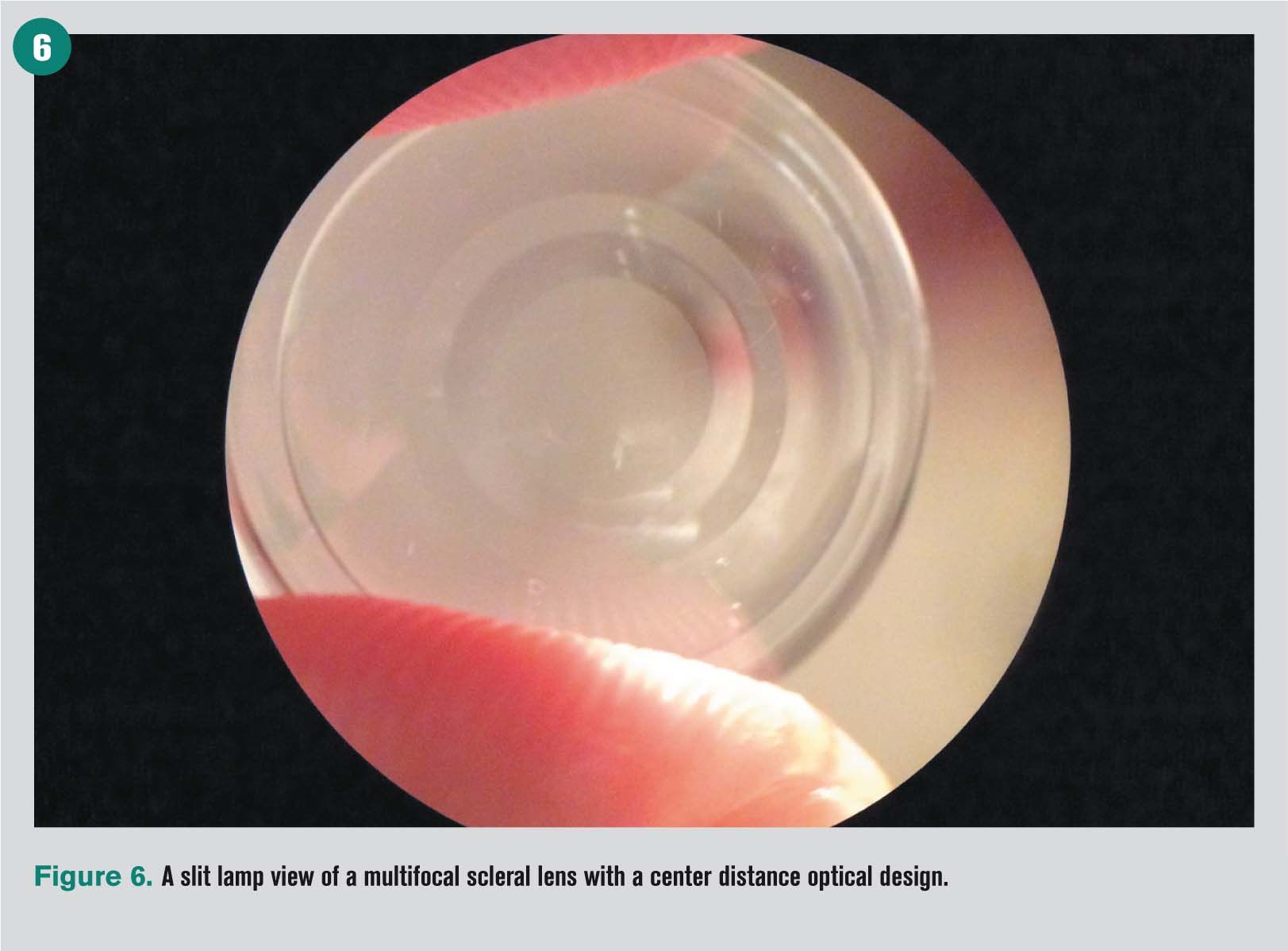
Nonetheless, for presbyopic patients who require more accommodative assistance, multifocal scleral lenses are becoming a great clinical addition to our optometric armamentarium.
Not only can scleral lenses help these patients who often have concomitant dry eye, there are numerous multifocal scleral lens options that provide exceptional vision across multiple visual ranges.16
Aspheric, center distance and center near designs are just a few of the multifocal lens options (Figures 5A, 5B; Figure 6).
Because scleral lenses protect and bathe the ocular surface, they are fantastic for patients who have been clinically diagnosed with dry eyes and/or have suffered poor on-eye contact lens performance related to their tear deficiencies.
As the patient profile complexity increases, scleral lens designs become exceedingly one of the first treatment options for us to recommend to patients. Therefore, it is no wonder that one of our top indications for scleral lens in healthy eyes is a patient with astigmatism, presbyopia, and dry eye.
Moving into sclerals
Today’s scleral lenses are an ideal way to expand a contact lens practice. Start with your existing patients with normal, healthy eyes, especially when vision, comfort, or both are suboptimal with patients’ habitual contact lens modalities.
Educate these patients on the benefits and risks of scleral lenses and help them set proper expectations with regards to the scleral lens fitting process.
You can offer this incredible technology to patients with astigmatism, athletic demands, dry eyes, allergies, presbyopia, or simply to improve vision and/or comfort compared to their habitual contact lenses.
Many professional resources exist to help clinicians obtain the latest developments in this field, including The Scleral Lens Education Society (www.sclerallens.org) and International Keratoconus Academy (www.keratoconusacademy.com).
Whether patients have regular corneas or existing corneal pathologies, scleral lenses can positively impact the lives of many of our patients. And in return, our optometric profession will be enriched with the satisfaction of delivering the best care that our patients deserve.
References
1. Visser ES, Wisse RP, Soeters N, Imhof SM, Van der Lelij A. Objective and subjective evaluation of the performance of medical contact lenses fitted using a contact lens selection algorithm. Cont Lens Anterior Eye. 2016 Aug;39(4):298-306.
2. Pritchard N, Fonn D, Brazeau D. Discontinuation of contact lens wear: A survey. Int Contact Lens Clin. 1999 Nov;26(6):157-162.
3. Young G, Veys J, Pritchard N, Coleman S. A multi-centre study of lapsed contact lens wearers. Ophthalmic Physiol Opt. 2002 Nov;22(6):516-27.
4. Richdale K, Sinnott LT, Skadahl E, Nichols JJ. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea. 2007 Feb;26(2):168-74.
5. Rumpakis J. New Data on Contact Lens Dropouts: An International Perspective. Rev Optom. 2010;147(11):37-42.
6. Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013 Jan;39(1):93-99.
7. Brujic M, Miller, J. Minimizing Dropouts: What You Can Do. Rev Cornea Contact Lens. Available at: http://www.reviewofcontactlenses.com/content/c/27244/. Accessed 9/19/17.
8. Nichols JJ, Willcox MD, Bron AJ, Belmonte C, Ciolino JB, Craig JP, Dogru M, Foulks GN, Jones L, Nelson JD, Nichols KK, Purslow C, Schaumberg DA, Stapleton F, Sullivan DA; members of the TFOS International Workshop on Contact Lens Discomfort. The TFOS International Workshop on Contact Lens Discomfort: executive summary. Invest Ophthalmol Vis Sci. 2013 Oct 18;54(11):TFOS7-TFOS13
9. MciIlraith R, Young G, Hunt C. Toric lens orientation and visual acuity in non standard conditions. Cont Lens Ant Eye. 2010 Feb;33(1):23-26.
10. Michaud L. Scleral Lens Fitting: Once Rare, Now Routine? Rev Cornea Contact Lens. Available at: https://www.reviewofoptometry.com/ce/scleral-lens-fitting-once-rare. Accessed 9/19/17.
11. Michaud L, Bennett ES, Woo SL, Reeder R, Morgan BW, Dinardo A, Harthan JS. Clinical Evaluation of Large Diameter Rigid-Gas Permeable Versus Soft Toric Contact Lenses for the Correction of Refractive Astigmatism. A MultiCenter Study. Eye Contact Lens. 2016 Nov 24. [Epub ahead of print]
12. Allergy Facts. American College of Allergy, Asthma, and Immunology. Available at:
http://acaai.org/news/facts-statistics/allergies. Accessed 6/12/17.
13. Urgacz A, Mrukwa E, Gawlik R. Adverse events in allergy sufferers wearing contact lenses. Postepy Dermatol Alergol. 2015 Jun;32(3):204-9.
14. Vance KD. Miller W. Bermangson J. Measurement of tear flow in scleral contact lens wearers. Poster presented at American Academy of Optometry annual meeting, October 7-10, 2015, New Orleans.
15. Michaud L, van der Worp E, Brazeau D, Warde R, Glasson CJ. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Anterior Eye. 2012 Dec;35(6):266-71.
16. Barnett M. Multifocal Scleral lenses. Contact Lens Spectrum. Available at: https://www.clspectrum.com/issues/2015/december-2015/multifocal-scleral-lenses. Accessed 9/1/9/17.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.