- March digital edition 2022
- Volume 14
- Issue 3
Contoured prism lenses enhance vision clarity and patient comfort
New technology improves precision of binocular vision disorder diagnosis and correction
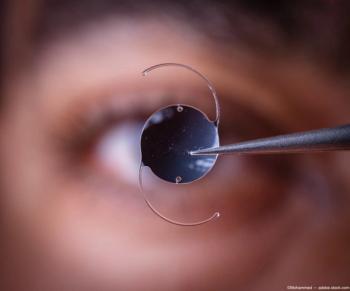
At its most basic level, the goal of optometry is to diagnose refractive errors and vision disorders, as well as to provide patients with optical lens-based devices to compensate for those deficiencies.
With respect to binocular vision disorders, conventional teaching directs optometrists to prescribe prism lenses and perhaps provide vision therapy (VT). However, unless an optometrist is regularly looking for binocular disorders and treating them, the disorders can be missed and implementing standard prism can be tricky.
After 17 years in practice, I have come to question the efficiency and practicality of prescribing standard prism correction, as there tends to be a lot of subjectivity in the measurements.
Further, patient acceptance of prism is challenging because the amount needed in the distance is different from what is needed at near. Instead, I’ve begun testing for and prescribing custom contoured prism spectacles for patients whose symptoms suggest they will benefit.
Whereas standard prism lenses correct eye misalignment at a single distance, Neurolenses with contoured prism (Neurolens) provide eye alignment at all distances by gradually increasing the prism from distance to near.
Prescribing Neurolens spectacles goes hand-in-hand with using a specialized eye tracking device, the Neurolens Measurement Device Gen 2 (nMD2). The nMD2 enables the optometrist to check eye alignment at distance and near, thus more easily and precisely measuring visual misalignment.
The objective of the nMD2 is to arrive upon the Neurolens value, which is the measurement used to prescribe contoured prism correction (Table 1). This technology helps treat a subset of patients whose symptoms often go unaddressed.
Unaddressed symptoms
Double vision is associated with binocular vision disorders (BVDs), but headaches, eye strain, dry eye sensation, and neck and shoulder pain are also red flags signifying visual misalignment.
Eye misalignment leads to increased effort by the visual system to realign to avoid double vision and strabismus.1
This constant effort to realign culminates in symptoms of trigeminal dysphoria such as chronic headaches, as well as the aforementioned dry eye sensation, neck pain and eye strain.
Even small prismatic corrections of the misalignment can reduce trigeminal dysphoria symptoms and improve visual comfort.1
Trigeminal dysphoria symptoms mimic and intersect with those associated with computer vision syndrome (CVS), and with the pervasive use of digital devices, these symptoms are naturally ubiquitous.
The process of prescribing Neurolenses starts with a Neurolens Lifestyle Questionnaire (Table 2).
These questionnaires identify patients who have discomfort with computer use, tired eyes, dry eye sensation, light sensitivity, dizziness, headaches, neck stiffness, or pain.
They also gauge how often the patients experience these symptoms. Patients who meet a specific symptom threshold can undergo testing with the nMD2, which provides precise, accurate, objective measurement of phoria and other alignment information.
Precise, objective measurement
BVDs are common, but patients often go untreated because recognition of these disorders tends to be limited by how dedicated optometrists are to looking for them.
The Neurolens Lifestyle Questionnaire makes it easy to identify patients who normally wouldn’t mention things such as neck and shoulder pain or even eye strain and headaches. Too often individuals consider these the price they pay for spending time looking at their laptops or smart phones.
Unlike traditional BVD measurement techniques, the nMD2 makes it easy to produce a prescription that will precisely compensate for a visual misalignment and/or trigeminal dysphoria.
The device captures more than 10,000 data points per patient and identifies eye misalignment as small as 0.10 PD. It’s an elegant process that can be delegated to technicians during pretesting.
Conversely, conventional measurement techniques are hindered by imprecision and subjectivity. The alternating cover test is associated with poor repeatability and limits a clinician’s ability to measure small eye deviations accurately.2
The smallest phoria value that can be detected with the cover test is approximately 2 to 3 PD. Furthermore, methods such as the Howell Phoria Card, the Maddox rod, and Von Graefe prism dissociation test are also limited by subjectivity and the inability to accurately test prism in small increments.3,4
Headache clinical trial
I have been prescribing Neurolens spectacles for about a year (as well as wearing them), and I am hearing positive feedback from some of my patients who have been fitted with these lenses.
I am also learning a great deal about the technology as an investigator in a Neurolens clinical trial that is focused specifically on the impact of these lenses on patients who have chronic headaches.
The multisite clinical trial is in the early stages. It began in October 2021 and is expected to end in April 2022, with an anticipated enrollment of approximately 250 participants.5 This trial is a 2-arm crossover study with 2 subgroups.
Participants are initially assessed for their headache symptoms through use of the Headache Impact Test (HIT-6) questionnaire, which measures the impact that headaches have on an individual’s ability to accomplish the activities of daily life.6
After this, the participants are provided an updated lens prescription, which they wear for 35 days. If the participant’s symptoms have subsided after that period, the patient is released from the study.
Participants who continue to meet inclusion criteria based on HIT-6 scores proceed to the evaluation portion of the protocol. They are randomized into 2 arms.
The first-arm participants receive Neurolens first, and the second-arm participants receive a standard single-vision or PAL lens (control lens). When participants return after 35 days of wearing their first test lens, the symptom questionnaire is reassessed.
After that assessment, they are crossed over to the second pair of study lenses. Participants will come back after wearing their second test lens for 35 days, and at that point the symptom questionnaire will be reassessed for the final time.
Practical and precise
When available, I suspect the study outcomes will further support my confidence in this lens.
What excites me the most about Neurolens is the practicality of the diagnostic process and the precision of the lens itself. We receive robust, reliable data in an efficient manner, which enables me to prescribe with confidence.
As Neurolenses and their ability to correct so many symptoms associated with CVS become familiar to the public, I will not be surprised if frequent computer users begin showing up at optometry offices specifically asking for Neurolens.
References
1. Labhishetty V. Can small prism corrections improve visual comfort? Yes! Here is why. Neurolens. March 3, 2021. Accessed December 6, 2021. https://blog.Neurolenses.com/small-prism-corrections
2. Hrynchak PK, Herriot C, Irving EL. Comparison of alternate cover test reliability at near in non-strabismus between experienced and novice examiners. Ophthalmic Physiol Opt. 2010;30(3):304-309. doi:10.1111/j.1475-1313.2010.00723.x
3. Fogt N, Baughman BJ, Good G. The effect of experience on the detection of small eye movements. Optom Vis Sci. 2000;77(12):670-674. doi:10.1097/00006324-200012000-00014
4. Anstice NS, Davidson B, Field B, Mathan J, Collins AV, Black JM. The repeatability and reproducibility of four techniques for measuring horizontal heterophoria: Implications for clinical practice. J Optom. 2021;14(3):275-281. doi:10.1016/j.optom.2020.05.005
5. Neurolens headache study. ClinicalTrials.gov. October 7, 2021. Accessed November 28, 2021. https://www.clinicaltrials.gov/ct2/show/NCT05070767?term=NCT05070767&draw=2&rank=1
6. Kosinski M, Bayliss MS, Bjorner JB, et al. A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res. 2003;12:963-974. doi:10.1023/a:1026119331193
Articles in this issue
almost 4 years ago
Keeping calm with positive vibesalmost 4 years ago
5 diabetes truisms that are (at least partially) falsealmost 4 years ago
Addressing the need for greater access in vision carealmost 4 years ago
Tackling the problem of contact lens dropout from presbyopiaalmost 4 years ago
The ideal glaucoma patient, from an optometrist’s perspectivealmost 4 years ago
5 reasons optometrists have failed to embrace myopia managementalmost 4 years ago
Restoring sight against all oddsNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.