Corneal hysteresis and biomechanics growing in diagnostic importance
Knowing your glaucoma vitals is key to providing best treatment for patients.

What are your glaucoma vitals? How do we monitor and predict glaucoma progression in the modern practice of optometry? Technology is shaping clinical education models, demonstrating the importance of corneal hysteresis (CH) in the modern management of glaucoma. CH is fluid and predictive of glaucoma progression.
When my (TW) optometry students and residents at State University of New York College of Optometry present to me, I want them to succinctly state the patient’s risk factors (eg, corneal thickness, ethnicity, genetics, age).
Progression analysis software is becoming more commonplace in the offices of optometrists and ophthalmologists. Let’s look at how the understanding of corneal biomechanics and hysteresis can improve our glaucoma outcomes.
Background
Glaucoma is a progressive neuropathy that causes destruction to the retinal nerve fiber layer, consequently damaging the optic nerve head. Progression of this disease can lead to functional vision loss, first affecting peripheral vision and eventually central vision in severe cases. This rate of progression can vary depending on risk factors pertaining to the individual affected.
The true mechanism of this disease is not entirely understood. Risk factors individuals may have can affect how quickly or slowly this disease progresses. This can make it very difficult for practitioners to determine effective treatment regimens for glaucoma patients.
Currently, IOP is the only modifiable risk factor and treatment often includes drops, laser, and/or surgical procedures.
Despite our best efforts, a large subset of patients progresses even with significant IOP reduction. Identifying a new risk factor that gives insight into speed of progression may be very useful for clinicians. Another tool that practitioners may consider is corneal hysteresis. This measurement can give more information to determine risk of progression and progression speed.1
Because of this, just lowering IOP in these patients to a normotensive level does not sufficiently stop the progression of glaucomatous damage in their eyes. Approximately a quarter of patients with glaucoma who have well-controlled, stable IOP will progress with visual field loss.
Early intervention for patients at high risk is crucial in slowing or preventing permanent damage and vision loss caused by glaucoma.2 This demonstrates the need to identify all risk factors that could be used in early diagnosis and perhaps help predict how quickly patients will progress.3
Identifying contributing risk factors will provide practitioners a better understanding of when and how aggressively patients should be treated.4 There is now mounting evidence that CH is a new risk factor.
Corneal hysteresis basics
CH has been identified as a new independent risk factor for glaucoma.
CH is a measurement of the viscoelasticity of the corneal tissue, which is determined using the ocular response analyzer (ORA; Reichert Technologies). The ORA is the only commercially available device that measures CH and provides a numeric result.1
It has been postulated that the biomechanical properties of the cornea may give us valuable insight into the biomechanics of the sclera and lamina cribrosa. The lower the corneal hysteresis, the higher the chances the lamina cribrosa cannot withstand fluctuations in IOP. This results in a higher risk of optic nerve head conversion to glaucoma as well as glaucomatous progression for those patients who have already received diagnoses.2
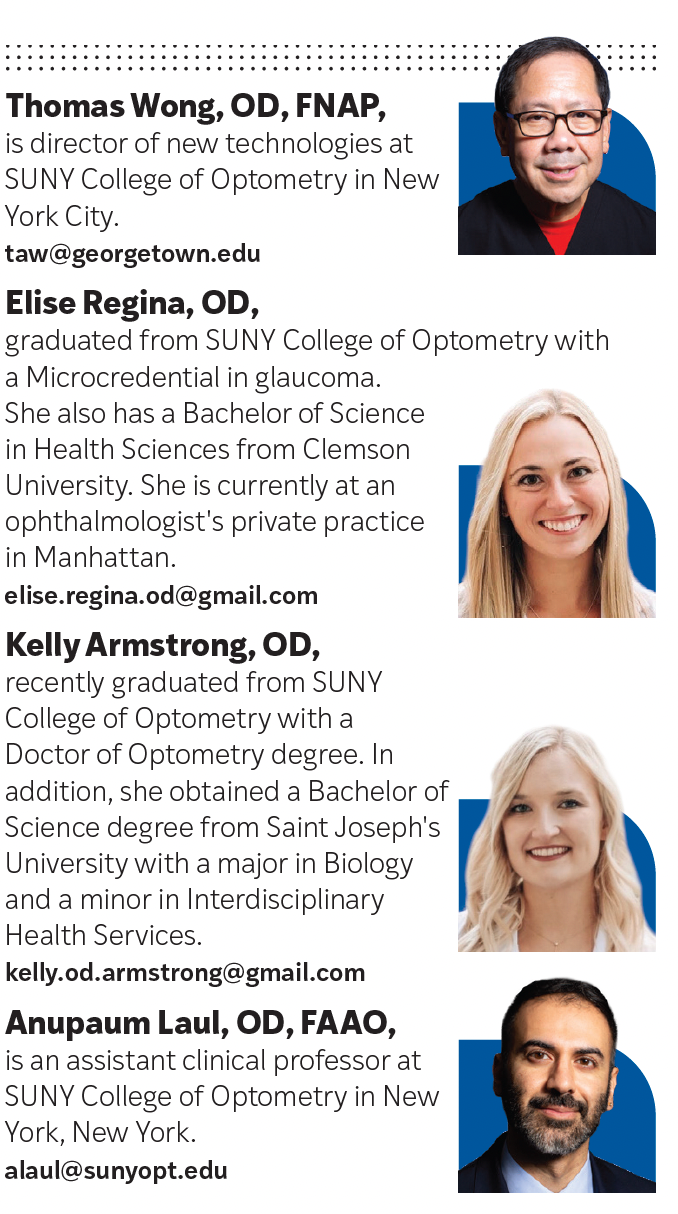
The ORA measures the biomechanical properties of the cornea by using applied force displacement. This is done by utilizing a puff of air to deform the cornea slightly into a concave surface. An optical sensor is then used to measure the reshaping of the cornea, which is timed to the pressure applied by the air puff. There are 2 application pressures measured with this machine.
The first measures the amount the cornea flattens after the puff of air makes contact and increases pressure on the corneal surface. The second measurement is the cornea deflecting and reshaping with the drop in pressure. The difference between these 2 measurements results in the CH in mm Hg and is related to the viscoelastic property of the cornea.2
The amount the cornea can resist the puff of air may reflect the resilience of the cornea’s extracellular matrix. This is a key area of study because this extracellular matrix is most likely related to the composition of the lamina cribrosa and peripapillary sclera. Therefore, a cornea with lower hysteresis may be related to an optic nerve that is more susceptible to damage from fluctuations in IOP.3
See Figure 1 for an ocular response analyer (ORA) reading, where the air jet pressure (P1) is shown when the cornea undergoes an inward applanation, and P2 is the pressure at which the cornea bends back to normal configuration. CH is defined by P1-P2.
Corneal hysteresis and glaucoma
There are copious publications on the relationship between CH and glaucoma. It has been shown that CH plays a significant role in the potential conversion to glaucoma, severity of the disease, and possible progression seen structurally and functionally using the optical coherence tomography (OCT) and visual field, respectively.1
Medeiros et al noted that CH is correlated to visual field loss over time.2 Every 1-mm Hg decrease of CH correlated with 0.25% per year of visual field progression.3
When evaluating eyes that have a well-controlled, normotensive IOP, the eyes with this progressive visual field loss also had reduced corneal thickness and low CH. This reiterates the likelihood that these are risk factors in glaucoma development and progression.4
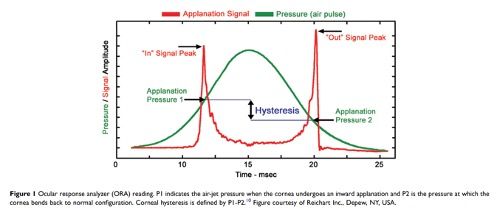
See Figure 2, which shows the cumulative probability of glaucoma development in suspect eyes with CH equal or greater than 10.2 mm Hg and in those with CH lesser than 10.2 mm Hg.
Patients who have a lower CH are much more affected by IOP and have a faster rate of visual field progression.3 Glaucoma patients whose eyes have both lower CH and higher IOP will have more progressive functional loss and advanced disease.3 Therefore, monitoring the corneal hysteresis may add important information for risk and rate of disease progression.3
Corneal hysteresis and therapy
Multiple studies show that CH might be predictive regarding effectiveness of eye drop therapy.1 Patients with glaucoma who had a low CH measurement and higher IOP at baseline had a more significant reduction in IOP when treated with a prostaglandin analog drop.1 Prostaglandins may also play a role in the maintenance of the extracellular matrix of ocular tissues; however, that needs to be further investigated.1
Treatment of IOP by either topical prostaglandis, selective laser trabeculoplasty (SLT), or via incisional surgery have been shown to increase corneal hysteresis; however, it is unknown whether it is a true effect of the biomechanics of the tissue or just a result of the acute IOP reduction.1
Conclusion
The biggest challenge that we face as clinicians when determining the appropriate treatment for glaucoma patients is not knowing the rate at which an individual will progress in this disease.
Through technological innovation, understanding CH will help improve clinicians’ ability to understand glaucoma development and progression. There is no doubt that there is a relationship between CH and glaucomatous progression.1 This can be a useful tool for practitioners to use in aid of developing a treatment regimen for patients.1
Although we tend to always focus on new technologies in the management of ocular disease and glaucoma, CH and other technologies should be important diagnostic tools in the modern management of glaucoma.
Moreover, it is time for those of us in clinical education to train future clinical optometrists and ophthalmologists on the value of understanding CH and biomechanics.
References
1. Zimprich L, Diedrich J, Bleeker A, Schweitzer JA. Corneal hysteresis as a biomarker of glaucoma: current insights. Clin Ophthalmol. 2020;14:2255-2264. doi:10.2147/OPTH.S236114
2. Susanna CN, Diniz-Filho A, Daga FB, et al. A prospective longitudinal study to investigate corneal hysteresis as a risk factor for predicting development of glaucoma. Am J Ophthalmol. 2018;187:148-152. doi:10.1016/j.ajo.2017.12.018
3. Medeiros FA, Meira-Freitas D, Lisboa R, Kuang TM, Zangwill LM, Weinreb RN. Corneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal study. Ophthalmology. 2013;120(8):1533-1540. doi:10.1016/j.ophtha.2013.01.032
4. Susanna BN, Ogata NG, Jammal AA, Susanna CN, Berchuck SI, Medeiros FA. Corneal biomechanics and visual field progression in eyes with seemingly well-controlled intraocular pressure. Ophthalmology. 2019;126(12):1640-1646. doi:10.1016/j.ophtha.2019.07.023

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.