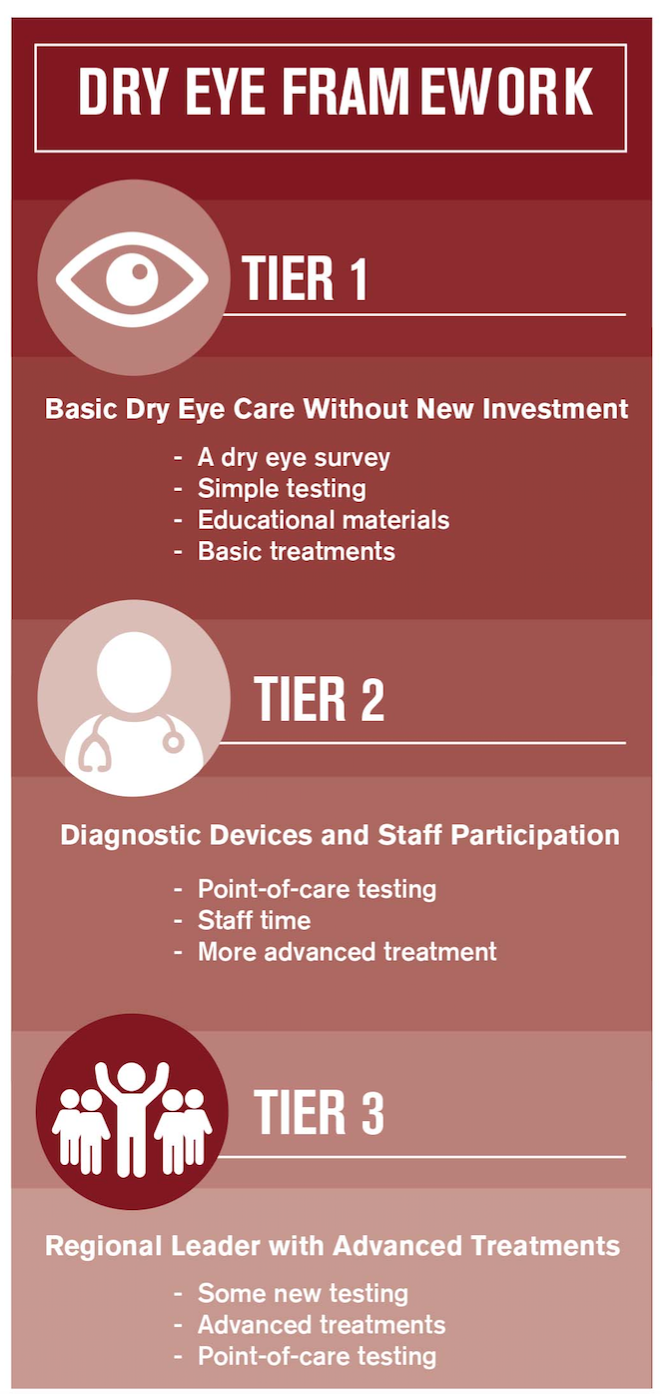
Dry eye protocol for any practice


Optometrists see a large disparity between the prevalence of dry eye disease and the number of patients who are treated.1 ODs know that they need to jump in with both feet, but that’s easier than it sounds.
Doctors attend dry eye courses offered at just about every meeting, and many may feel paralysis of analysis. They learn about the latest high-tech diagnostics and treatments. They read protocols for dry eye disease with a depth and breadth that makes busy practitioners wonder where to begin.
To make dry eye evaluation and treatment routine for all patients and solve the problem of this underdiagnosed, undertreated disease, we need an accessible entry point for practices that don’t have a battery of diagnostic equipment or dedicated capital and space for dry eye.
To bridge the gap between traditional practices and tech-heavy dry eye clinics, I created a new protocol with Alan Kabat, OD, FAAO-a logical, easy-to-digest framework that fits all types of practices.
The protocol is arranged in three tiers according to the level of dry eye care optometrists want to offer. At every tier, patients get the diagnosis and treatment they need, either inside the practice or through trusted referral.
Here, I would like to share a high-level overview of that framework.
Tier 1: Basic care without new investment
At Tier 1, practitioners screen the general population for dry eye, as well as seeing dry eye as a primary complaint. Most eyecare practitioners are already practicing at Tier 1, although they may not acknowledge it as part of their assessment.
If practitioners want to expand their approach to dry eye, they can quickly move to Tier 2. If this level fits best with practitioners’ practice goals, they can stay at Tier 1 and refer moderate to severe patients for tertiary care.
At Tier 1, diagnosis relies on the tools already on hand with no new purchases or additional exam time.
These are the basic components:
• Dry eye survey. Using a standardized survey for all patients helps identify who is symptomatic for dry eye as well as how well dry eye treatments are working. Surveys like Standardized Patient Evaluation of Eye Dryness (SPEED) and the Dry Eye Questionnaire 5 (DEQ-5) offer quick completion by the patient and scoring by doctors or staff.
• Simple testing. In the exam room, doctors perform fluorescein staining as part of the traditional slit lamp exam, check the appearance of the meibomian glands and eyelids, and note the quality and expressability of the meibum.
These are parts of a routine exam, but doctors combine the observations with survey results to draw initial conclusions about dry eye disease. In addition to fluorescein staining, lissamine green can be utilized to assess the eye for conjunctival staining as well lid wiper epitheliopathy and the positioning of the line of Marx. Lid hygiene, lid closure, and presence of telangiectasias may be noted on examination. Also, the tear prism height can be quickly assessed during slit lamp examination.
Related: How to start treating dry eye at your practice
• Educational materials. Patient education not only provides a greater understanding of dry eye disease, but it also aids in compliance and understanding the chronicity of the condition. Discussions can be accompanied by patient education sheets to help teach patients about dry eye and how to perform home care.
• Basic treatments. If the dry eye disease is evaporative, a lipid-based tear and warm compress may be warranted. The inflammatory component of dry eye disease can be treated by the use of omega nutritional supplements and prescription ophthalmic medications such as cyclosporine (Restasis, Allergan) or lifitegrast (Xiidra, Shire), as well as lifestyle changes. If the patient’s dry eye isn’t controlled, adjustments may be made within the regimen off Tier 1, but if patients fail to make marked improvement, further intervention may be required.
Tier 2: Diagnostic devices and staff participation
As practitioners move from Tier 1 to Tier 2, it is time to make additional financial commitments, adding new testing technologies and prioritizing staff engagement for ocular surface disease.
A Tier 2 practice has all the dry eye offerings of Tier 1, plus these features:
• Point-of-care testing. At this level, doctors consider adding tear osmolarity testing (TearLab Osmolarity Test, TearLab), an MMP-9 inflammatory mediator test (InflammaDry, Quidel), and/or meibography (LipiView II, Johnson & Johnson Vision; Keratograph 5M, Oculus; and SL-D701 slit lamp attachments, Topcon). They can perform ocular photography as well.
A complaint of dry eye disease symptoms or a diagnosis of ocular surface disease may dictate additional diagnostic tests. A physician’s order for the test is made, and once the test is executed, appropriate interpretation of the testing must be completed. The evaluation may be charged with an appropriate diagnosis and medical necessity.
Related: 3 tips to incorporate or expand your dry eye services
• Staff time. Staff take an active role in patient education at this level, and staff require training by practitioners. They initiate education before patients see the doctor, or efficiency will drag. In my experience, I recommend choosing empathetic people who are well suited to dry eye patients’ higher level of anxiety.
• More advanced treatment. Moderate additions to treatment include in-office lid debridement such as microblepharoexfoliation (BlephEx, RySurg). Practices may add additional diagnostic and therapeutic pieces over time. Thermal pulsation, amniotic membranes, and other options are often integrated incrementally.
Tier 3: Regional leader with advanced treatments
Tier 3 is a dry eye center. The doctor makes a solid commitment to treating dry eye, becoming a thought leader in the city or region. Optometrists and ophthalmologists refer their dry eye patients to this practice.
Tier 3 offers the same benefits as Tier 2, as well as these additions:
• New testing. One of Tier 3 practices’ greatest services is to act as referral destinations for other eyecare practitioners in their markets. Not all doctors share an interest in managing dry eye at an advanced level, preferring instead to rely on a colleague for that care. Being a trusted resource is an important role.
• Advanced treatments. Tier 3 practices utilize diagnostic testing and advanced therapeutic options. At this level, advanced therapeutic options are engaged frequently. Doctors can use thermal pulsation for meibomian gland dysfunction (MGD) and intense pulsed light (IPL) (M22 OPT, Lumenis) therapy to address underlying inflammation. Amniotic membrane promotes healing of the ocular surface, while serum tears provide relief in advanced cases. Patients can be referred for treatment of punctual stenosis or conjunctivochalasis.
• Staffing and scheduling changes. In most dry eye clinics, a doctor and staff have dedicated time on certain days or at least parts of the day to only dry eye.
Low threshold for adoption
As dry eye knowledge and capabilities continue to evolve, I frequently update this protocol on my website. It is not designed to be a substitute for the comprehensive research of exceptional protocols such as TFOS DEWS II, but rather to provide practical, accessible guidance for how to apply knowledge of dry eye in daily practice with the tools at our disposal.
I hope this low-threshold framework for adoption lays out how practices can get started, regardless of the level of dry eye interest and commitment.
References:
1. Paulsen AJ, Cruickshanks KJ, Fischer ME, Huang GH, Klein BE, Klein R, Dalton DS. Dry eye in the beaver dam offspring study: prevalence, risk factors, and health-related quality of life. Am J Ophthalmol. 2014 Apr;157(4):799-806.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.