It’s not just about the eyes but the skin too
Optometrists at the forefront of ocular basal cell and squamous cell carcinomas
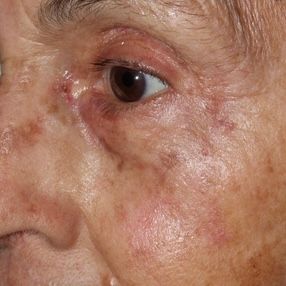
Basal cell CA

Rich Castillo, OD, DO
Optometrists are in a unique position to diagnose carcinomas of the eyelids. Rich Castillo, OD, DO, who is in practice in Tahlequah, OK, described how to establish a comprehensive approach towards skin cancer screening in an optometric practice.
Looking outside the box
Knowledge about skin cancer is important considering the startling statistics, i.e., 20% of Americans will develop skin cancer by age 70 and almost 6 million new cases develop annually. Broken down further, this translates to 15,000 new cases daily and of these 10% develop on the eyelids, Dr. Castillo reported.
Recognition of these lesions is key and the ABCDE System is helpful for screening for skin cancer; this includes A, asymmetry; B, border; C, color; D, diameter; and E, evolution.
The American Society of Optometric Surgeons defines asymmetry of melanoma as moles with an asymmetrical appearance, border as blurry/jagged edges, color as more than one color, diameter as size larger than a pencil eraser (about ¼ inch), and evolution as a mole that has changed suddenly in size, shape, or color.
He reported that the classic signs of lid carcinoma are madarosis, lid notching, loss of meibomian gland orifices, surface telangiectasias, and ulceration.
In the precancerous stage, actinic keratoses can progress to basal or squamous cell carcinoma (SCC and BCC, respectively). Keratoacanthomas are now considered a subtype of SCC and not a precancerous lesion.
The generally applied treatment for actinic keratosis is liquid nitrogen cryotherapy; others, but not preferred, include 5-fluorouracil (5FU) (Efudex, Valeant Pharmaceuticals) and Imiquimod (Aldara, Inova Pharmaceuticals), electro or radiosurgery, CO2 laser ablation, and curettage followed by one of the previous treatments.
The risk factors to be aware of for skin cancer are fair skin; presence of genetic syndromes such as Gorlin syndrome, xeroderma pigmentosum, and oculocutaneous albinism; chronic sun exposure or radiation therapy; age over 50 years; and exposure to arsenic or tar.
Squamous Cell CA
Commonly encountered skin cancers
The most common are BCC and SCC.
BCC. This occurs in upwards of 80% of cases and is 4 times more common than SCC. BCC is the most common cause of enucleation or orbital exenteration in the Western hemisphere.
Subtypes of this carcinoma include nodular (pigmented and infiltrative), which is characterized by rolled or pearly margins, chronicity, and common development on the head and neck; superficial, which is characterized by a scaley erythematous plaques, slow growth, no symptoms; and morpheaform or sclerosing, which have a scar-like appearance, slow growth, poorly defined borders, no symptoms, and difficult control for margins at biopsy, Dr. Castillo described.
Excisional biopsy is the gold standard for BCC and has a 90% to 95% cure rate. Other approaches include radiation, desiccation and curettage, and topic therapy with 5-FU or imiquimod, which has a 50% to 75% cure rate.
SCC. The major SCC subtypes are in situ (Bowen’s disease and carcinoma in situ) and invasive and keratoacanthoma.
The risks associated with Bowen’s disease are arsenic exposure, human papillomavirus 16, and radiation exposure.
Invasive SCC looks like an erythematous nodule that is firm and slow growing and generally results from sun exposure. More men than women are affected.
Keratoacanthoma, now considered a variant of SCC, grows rapidly over a few weeks; this nodular lesion can have a plug of keratin in the center or look like a nodular hyperkeratotic lesion. The lesion can regress over time but may evolve to invasive SCC. The risk include trauma, sun exposure, and human papillomavirus 11 and 16.
Dr. Castillo described that invasive SCC can exhibit perineural invasion around the orbit; the lesion can metastasize in from 1% to 3% of cases. If metastatic to the lungs occurs, there is no cure.
Treatments for in situ SCC are Efudex or Aldara, cryosurgery, radiation, desiccation and curettage by electro or radiosurgery. The best option, he noted, is surgical excision; clear margins include a cure.
Invasive SCC requires a systemic cancer work-up, surgical excision, radiation, immunotherapy, and chemotherapy.
Screening protocol for oculofacial carcinoma
The risk level is the driving factor.
For patients at low risk, screening is not recommended.
A number of factors should be considered to establish high risk. These include:
• Patient phenotype, i.e., more than 50 nevi, tendency for sunburn, red/blonde hair, blue eyes, freckles, and albinism.
• Personal history including nonmelanoma skin cancer; actinic keratoses; leukemia, lymphoma, childhood cancer, HIV; immunosuppression for solid organor stem cell transplantation.
• Genetic predisposition including rare genetic disorders, personal/family history or suspicion of a TP53 mutation; and germline mutations or polymorphisms related to increased risk of melanoma.
• Environmental exposures including sun/ultraviolet exposure, and previous radiation exposure.
Patients at increased risk should undergo annual screening with a comprehensive eye examination.
“Screening for eyelid cancer is an important public health service that all primary care practitioners need to be providing for their patients. Optometric physicians are in a unique position to serve the public welfare in this regard,” Dr. Castillo concluded.
This article is adapted from Dr. Castillo’s virtual SECO presentation, March 9, 2022. He has no financial interest in this subject matter.