Maximum medical therapy in glaucoma
A few months ago, I began to see what may be a little more progression on her OCT studies. I’m fairly confident that we’re in a good place right now as far as compliance is concerned, and I’m entering a crossroads with her regarding possibly adding therapy vs. getting a consult for a laser procedure, such as selective laser trabeculoplasty (SLT), vs. getting a cataract consult.
One of my glaucoma patients is a 66-year-old African American female who got her first glasses from my grandfather (the original Dr. Casella) in the early 1950s. I began seeing her in 2008, and I’m hoping that, any day now, she’ll start acting like she believes what I tell her about her prognosis if she doesn’t use her drops on a regular basis. I have her on a prostaglandin at bedtime and a beta blocker combination drop in the morning and afternoon (in an attempt to avoid beta blocker effects during the night). We’ll plug along for up to a year or so with reportedly good compliance and intraocular pressures (IOP) at target (which for her is 14-17 mm Hg OU). I check her pressures at different points in the day to try to get a feel for her diurnal fluctuation and feel as though she’s pretty “flat” throughout the day.
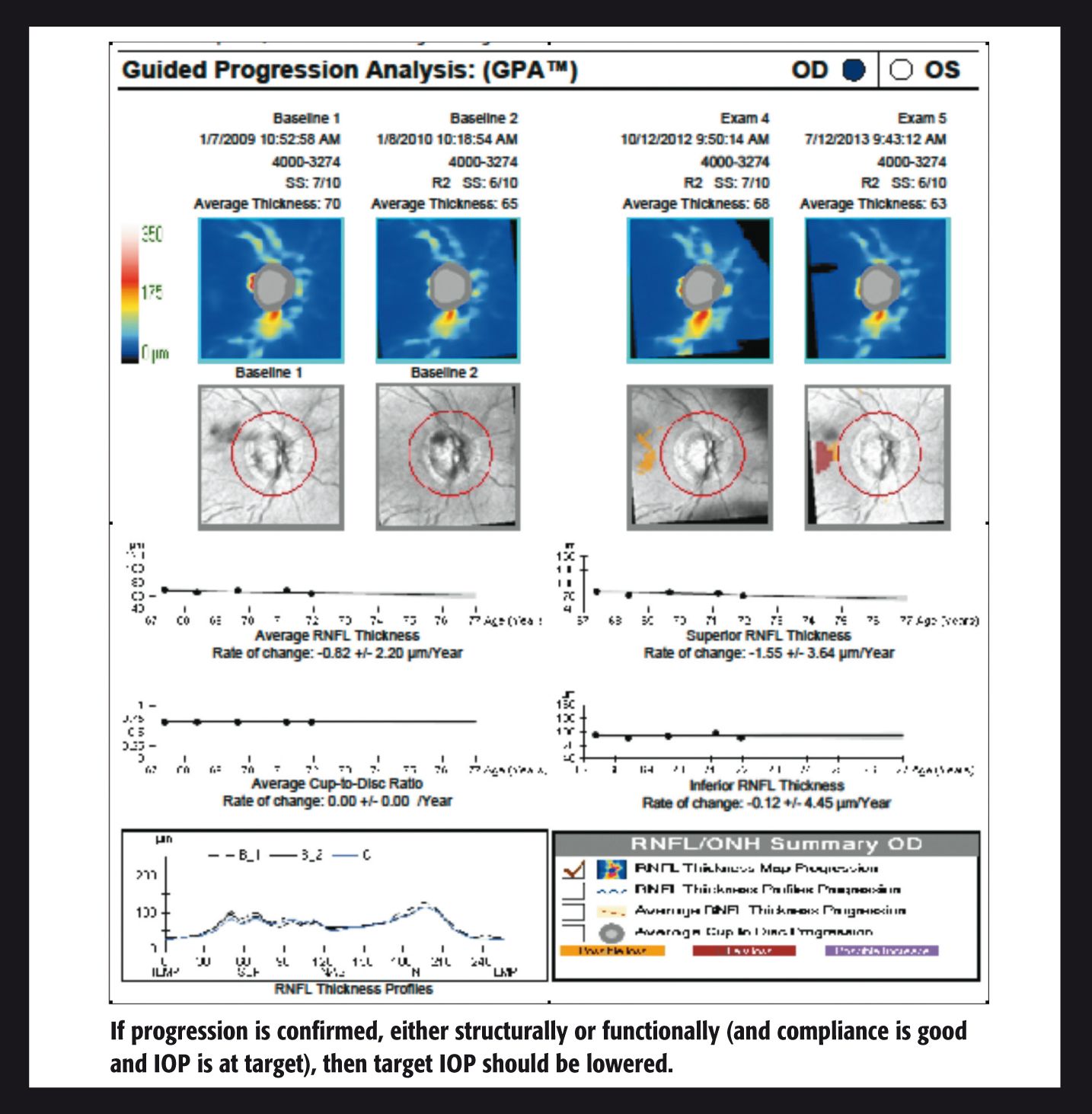
A few months ago, I began to see what may be a little more progression on her OCT studies. I’m fairly confident that we’re in a good place right now as far as compliance is concerned, and I’m entering a crossroads with her regarding possibly adding therapy vs. getting a consult for a laser procedure, such as selective laser trabeculoplasty (SLT), vs. getting a cataract consult. (She is phakic with 20/30 acuities, but she doesn’t want to have cataract surgery right now.) I don’t think her lenses are phacomorphic, but maybe we could achieve a mild IOP drop with cataract extraction. We discussed this, but she is pretty adamantly opposed to cataract surgery and insists she sees “fine.” I didn’t argue with her.
More drops vs. SLT consultation
I’m will attempt to confirm this progression in the next couple of months with another OCT and visual field study, and, if I can confirm the presence of progression, then, by definition, we’re not at target pressure any more. So, let’s take cataract surgery off the table for the moment and talk about additive therapy vs. getting a consult for an SLT.
If I confirm progression, then I should probably do something further. She’s 66 years old, not 166 years old. She has had breast cancer, but her prognosis is good and she is otherwise pretty healthy. This leads me to believe we should plan on spending another couple of decades or so together. So, should I add a third drop into the mix knowing that compliance has been a factor in the past? I’m thinking not so much. Studies and common sense have shown that adding medications means more effort and cognitive demand on the part of all patients (and I’m thinking especially this patient).1 This is why combination drops are so desirable-they afford the ability of adding another medication with the luxury of not having to add another bottle. That’s why it’s typically a good idea to add one of the components of a combination drop and then build up to a combination drop if need be.
Now, this patient and I have a pretty good rapport, and I believe she listens to me (at least most of the time). Good rapport and communication can go a long way toward improving compliance,2 and I always try to set aside extra time to talk with this particular patient to see how things are going. If I can confirm progression in the presence of good compliance, we’ll have a conversation about adding a third drop vs. getting a consult for an SLT. However, I’ve pretty much made up my mind that I’m going to push for a consult. I just don’t think she’s going to be able to stick with 3 bottles worth of drops (I don’t think I could either). So, if it comes to that, that’s the direction in which I’m going to take the conversation.
While we’re talking about additive therapy and progression, I should say that if this patient was in her 90s, my views on progression would take more of a pragmatic turn. By this, I mean that a little bit of progression very late in life will likely not lead to visual impairment. Glaucoma is a progressive disease by definition, and sometimes a little progression doesn’t mean failure on the part of the clinician. However, in the case of this particular patient, I have a valid argument for intervening further if things go south-likely lowering her target pressure to 12-14 mm Hg OU, as well. I want to intervene in as effective a way as possible, and, in many cases, effectiveness, simplicity, and convenience go hand in hand.ODT
References
1. Khouri AS, Realini T, Fechtner RD. Use of fixed-dose combination drugs for the treatment of glaucoma. Drugs Aging. 2007;24(12):1007-16.
2. Nordmann J, Badouin C, Renard JP, et al. Identification of noncompliant glaucoma patients using Bayesian networks and the Eye-Drop Satisfaction Questionnaire. Clin Ophthalmol. 2010 Dec 8;4:1489-96.