Optic disc swelling early sign of cat-scratch neruoretinitis
Scratches by young felines can lead to ocular complications. Find out how a patient’s floater led to a referral and diagnosis of cat-scratch neuroretinitis.

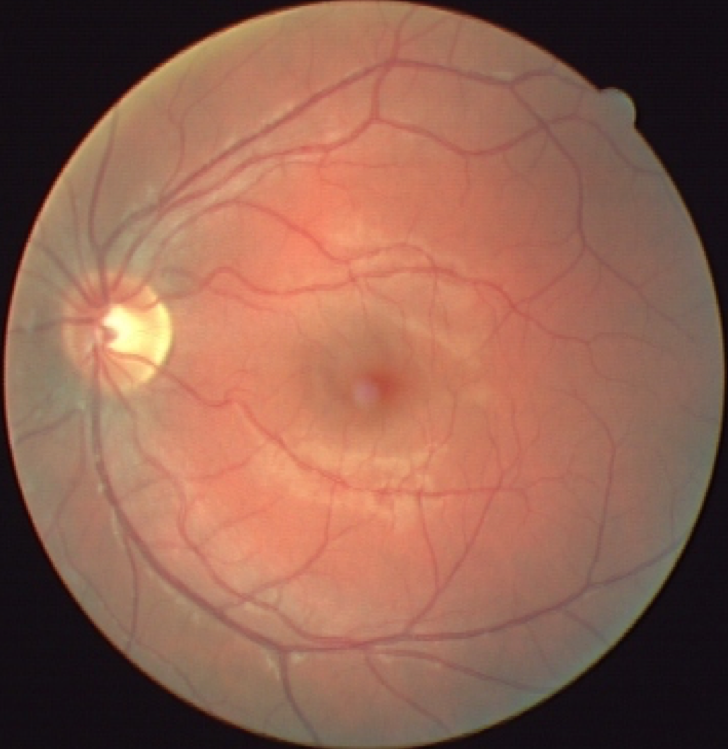
Figure 1. Initial presentation of the right eye. Note the granuloma consistent with retinitis and optic disc swelling completing the clinical picture of neuroretinitis. Images courtesy Leo P. Semes, OD, FAAO

Figure 2. The uninvolved left eye is shown for comparison.
A 22-year-old male was sent by a colleague for evaluation of a floater in the right eye. The patient was healthy with uncorrected vision of 20/20 in each eye. He took no medications. The reported duration of his symptoms was two days.
Initial exam findings
His pupils were dilated upon arrival, but the referring OD reported no relative afferent pupillary defect (RAPD). The patient’s anterior segments were free from cells and flare. On stereoscopic fundus evaluation, mild vitritis was responsible for the granuloma appearance to which the floater was attributed. He had subtle optic disc swelling nasally in the right eye (Figure 1), which is evident when comparing the appearance of the uninvolved left eye (Figure 2).
Previously from Dr. Semes: Clinical findings supported by new OCTA technology
On careful questioning, the patient disclosed having adopted a stray kitten within the past few weeks that had scratched the back of his right hand. This fact and the clinical findings added up to a diagnosis of cat-scratch neuroretinitis.
Cat scratch leads to complications
Optic disc edema has been reported as an early sign of cat-scratch neruoretinitis.1 The causative organism is Bartonella henselae, which is almost ubiquitous in the environment.
The findings and options were discussed with the patient, and treatment with 800 mg sulfamethoxazole (Bactrim DS, Sun Pharmaceutical Industries Ltd.)and 160 mg trimethoprim (Polytrim, Allergan) bid po for two weeks was recommended.
Because of the sulfamethoxazole component, it was important to rule out previous adverse sulfa reactions. In the face of reported spontaneous resolution, it is significant to consider offering a treatment option and consider potential consequences.2, 3
Ocular sequelae in untreated cases of cat-scratch neruoretinitis include vascular occlusions, macular-star formation, or rarely, choroidal neovascularization with potential for permanent vision loss, especially in pediatric cases.2,4-7
Related: The case of the disappearing drusen
Alternative systemic antibiotic options to the sulfmethoxazole/trimethoprim combination have been reported for sulfa-sensitive patients. Guidance for management of systemic manifestations includes laboratory evaluation and culture/sensitivity testing.8
Following up
The patient had complete resolution of the clinical findings at the two-week follow-up visit. Visual acuity remained at 20/20 in the involved eye. He reported no adverse effects from the antibiotic treatment.
This case illustrates an onset of Bartonella henselae infection responding to systemic antibiotic treatment.
References:
1. Wade NK, Levi L, Jones MR, Bhisitkul R, Fine L, Cunningham ET Jr. Optic disk edema associated with peripapillary serous retinal detachment: an early sign of systemic Bartonella henselae infection. Am J Ophthalmol. 2000 Sep;130(3):327-34.
2. Solley WA, Martin DF, Newman NJ, King R, Callanan DG, Zacchei T, Wallace RT, Parks DJ, Bridges W, Sternberg P Jr. Cat scratch disease: posterior segment manifestations. Ophthalmology. 1999 Aug;106(8):1546-53.
3. Reed JB, Scales DK, Wong MT, Lattuada CP Jr, Dolan MJ, Schwab IR. Bartonella henselae neuroretinitis in cat scratch disease. Diagnosis, management, and sequelae. Ophthalmology. 1998 Mar;105(3):459-66.
4. Eiger-Moscovich M, Amer R, Oray M, Tabbara KF, Tugal-Tutkun I, Kramer M. Retinal artery occlusion due to Bartonella henselae infection: a case series. Acta Ophthalmol. 2016 Aug;94(5):e367-70.
5. Nickerson TE, Oliveira CR, Lesser RL, Andiman WA. Macular Star and Central Visual Loss: Two Pediatric Cases. Clin Pediatr (Phila). 2016 May;55(5):496-8.
6. Latanza L, Viscogliosi F, Solimeo A, Calabrò F, De Angelis V, De Rosa P. Choroidal neovascularisation as an unusual ophthalmic manifestation of cat-scratch disease in an 8-year-old girl. Int Ophthalmol. 2015 Oct;35(5):709-16.
7. Durá-Travé T, Yoldi-Petri ME, Gallinas-Victoriano F, Lavilla-Oiz A, Bove-Guri M. Neuroretinitis Caused by Bartonella henselae (Cat-Scratch Disease) in a 13-Year-Old Girl. Int J Pediatr. 2010; 2010: 763105.
8. Caserta MT. Cat-Scratch Disease. Pediatric Clinical Advisor (Second Edition). Eds. Garfunkel LC, Kaczorowski JM, Christy C. Philadelphia: Elsevier Mosby, 2007. 96.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.