Topical immunomodulators can help chronic ocular allergic disease
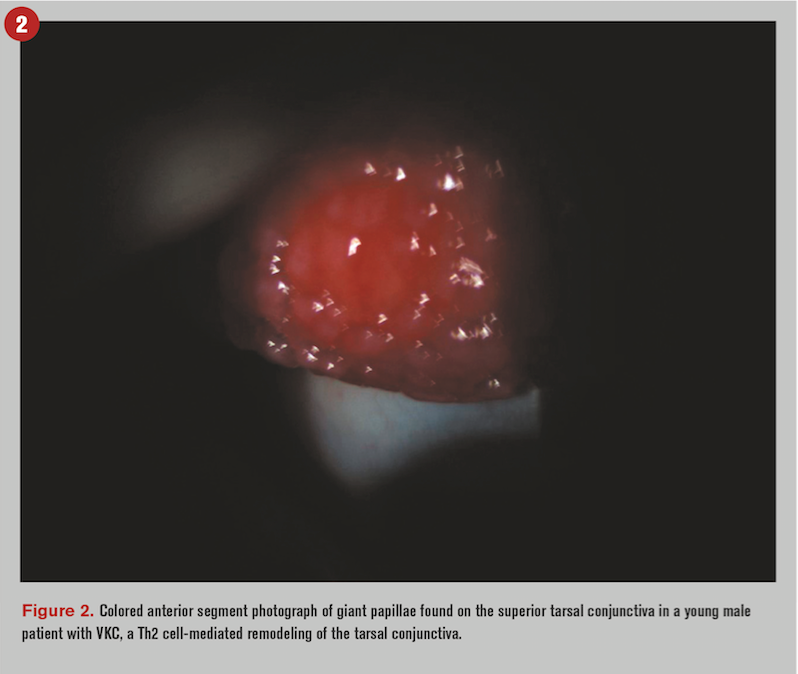
Given that allergies are the sixth leading cause of chronic illness in the United States with an estimated annual cost of greater than $18 billion1 and that 40 to 60 percent of those affected experience ocular involvement,2 allergic eye disease is destined to end up in your exam chair.
You may think, “So what? I’ll just grab my trusted antihistamine/mast cell stabilizer combo and we’ll call it a day.”
However, research indicates that chronic ocular pruritus can be present in almost 30 percent of your patient population.3 Furthermore, patients with moderate to severe pruritus exhibit increased symptoms of dry eye, neuropathic-like pain, nonocular pain, and demonstrate symptoms of generalized systemic hypersensitivity.4
Not only may the standard combo drop be inadequate, but it may benefit your patients to treat their chronic allergic conditions more aggressively to avoid neuropathic hypersensitivity. Astute clinicians are aware of the full scope of their treatment options and know when to pull out the big guns.
Below the surface
Allergic hypersensitivity reactions affecting the eye are IgE and/or T-cell mediated.5 IgE-mediated reactions are common and seen in run-of-the-mill allergic conjunctivitis, whereas T-cell–mediated responses are seen in more chronic cases of ocular allergy. T-cell–mediated responses can lead to irreversible changes to the architecture of the ocular surface, causing fibrotic damage and decrease in visual potential.
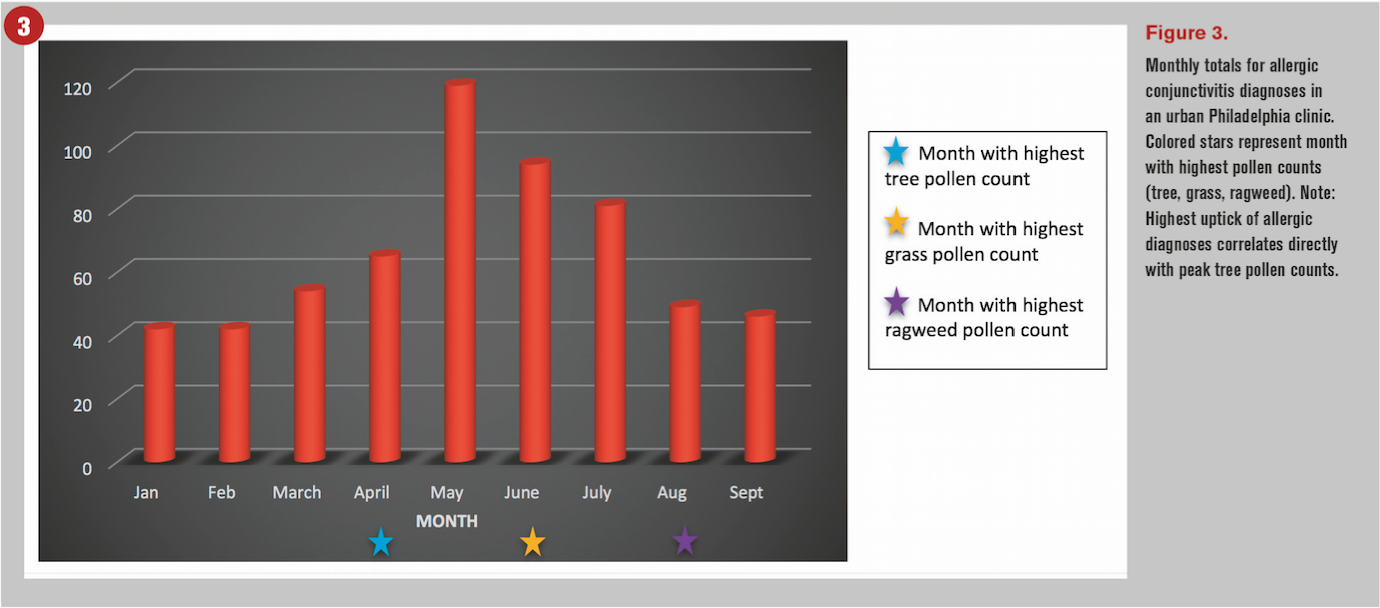
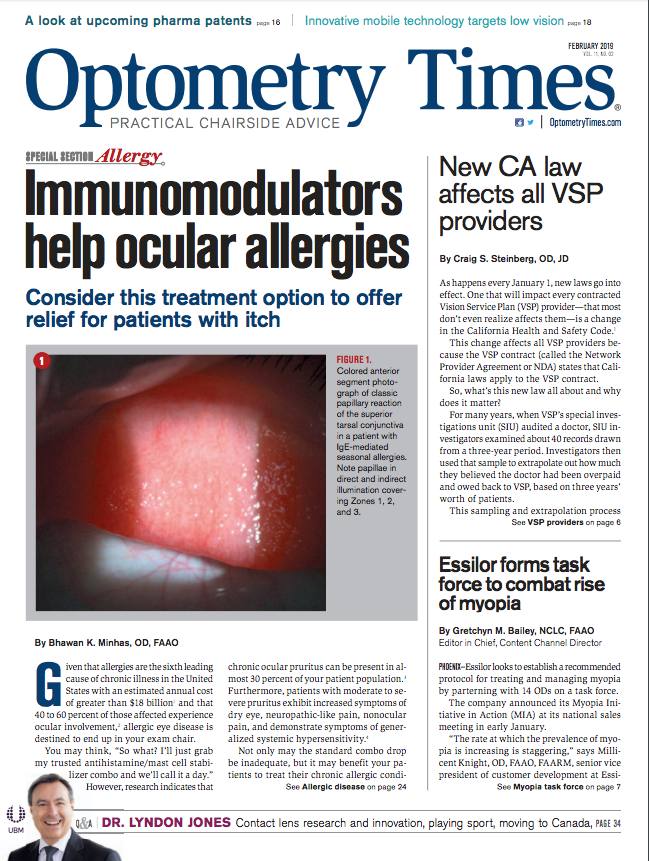
As environmental allergens encounter IgE-primed mast cells in the conjunctiva, they begin the sensitization phase of a cascade of events that ultimately lead to the classic signs and symptoms of ocular allergy. Namely, the release of histamine, tryptase, IL-4, leukotrienes, prostaglandins, and other mediators from degranulated mast cells cause symptoms of hyperemia, chemosis, tearing, and pruritus and classic conjunctival papillary lesions (see Figure 1).6
Related: Diagnosing and managing ocular allergy
Mast cell-derived mediators can be divided into two groups: those associated with granules (histamine, proteoglycans, tryptase, chymase, etc.), and those synthesized de novo (prostaglandins, leukotrienes, platelet factor, cytokines, etc.).7
The de novo products include cytokines (IL-4, IL-5, IL-6, IL-13, TNF-α, and TGF-β) and chemokines (CXCL8, CCL3, CCL5, and eotaxin), which further propagate the allergic inflammatory cascade.8
Of the released mediators, histamine and tryptase are the most studied in the tears of patients suffering from ocular allergy.9
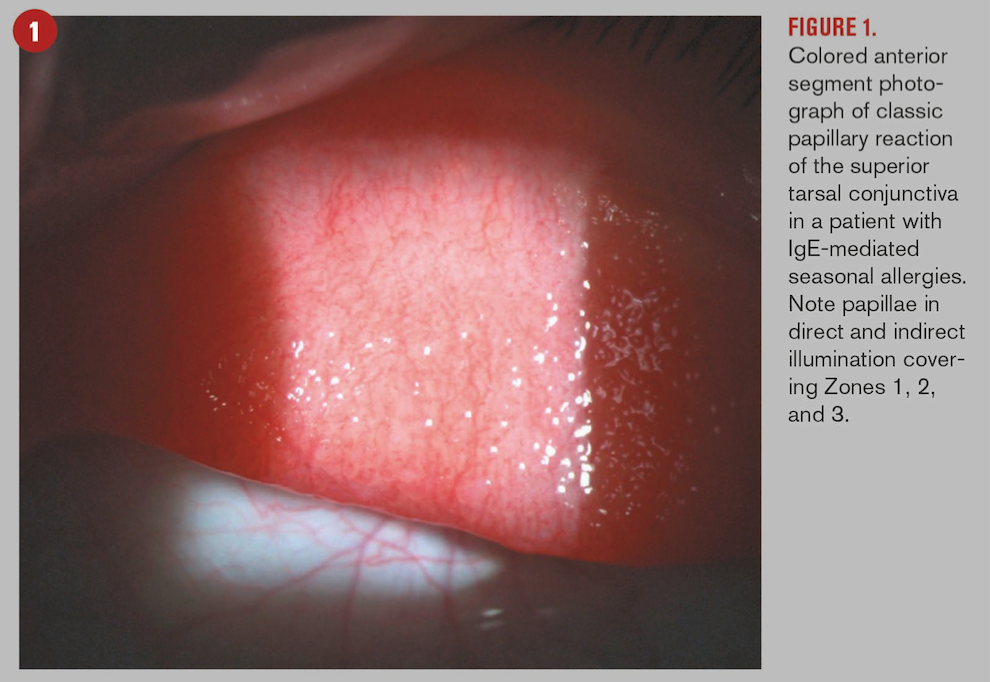
Chronic and often more ominous forms of ocular allergy, including vernal keratoconjunctivitis and atopic keratoconjunctivitis, have been shown to follow an inflammatory cascade that is predominantly mediated by T cells. The activation and subsequent increase of T lymphocytes, namely Th2 cells, in the conjunctiva is thought to have a vital role in a more chronic presentation.10 This pathway of events focuses on Th2 mediated cytokines (IL-4, IL-5, and IL-13) which activate both mast cells and eosinophils.10
Triggering this more chronic response leads to a more prominent and enduring structural remodeling of the conjunctiva via collagen type I, III, IV, and V (see Figure 2).11 Furthermore, though present and often exaggerated, an IgE-mediated reaction is a secondary event in these chronic forms;12 hence, your average combo medication not being able to quite scratch that itch.
Is TSLP making you itch?
Thymic stromal lymphopoietin (TSLP) is a cytokine and proallergic molecule that is a hidden culprit in the allergic inflammatory response. Though also involved in the propagation of an allergic response, it can cause pruritis.13
This happens via TSLP receptors that can be found on sensory neurons and immune cells, specifically dendritic cells, T cells, B cells, natural killer cells, mast cells, basophils, and eosinophils.13
Interestingly, downstream production of IL-4, IL-5, and IL-13, the cytokines involved in Th2 mediated allergic response, have been linked to TSLP.8
Ocular itch can be a very real and debilitating consequence of allergy and is often not controlled in chronic cases by an antihistamine/mast cell stabilizer combo; potential future pharmacological agents that target TSLP may be a more promising answer.
When to bring in the cavalry
Ocular allergy management can include both allergen avoidance, though easier said than done, and pharmacotherapy.
Common drugs that jump into most clinicians’ minds when presented with a red and itchy eye include vasoconstrictors, antihistamines, mast-cell stabilizers, combo antihistamine/mast-cell stabilizers, nonsteroidal anti-inflammatory agents, and-if severe enough-steroids.
Related: A look at the latest and upcoming pharmaceutical patents
While topical corticosteroids can come in clutch when dealing with severe cases, they are often needed on a chronic course and their prolonged use can prove taxing with serious and unwanted sequelae. Keeping a patient on a chronic topical steroid should not be taken lightly and alternative treatments should be considered if available.
Cases in which there is significant remodeling, even fibrosis, of the conjunctiva; corneal involvement; or risk to visual potential should implore a clinician to consider reaching for topical immunomodulators.
Two potential agents to consider are cyclosporine and tacrolimus.
Cyclosporine: Not for weak of heart
Cyclosporine is a non-steroidal immunomodulatory which was first developed in the 1970s as a novel drug to inhibit lymphocytes both specifically and reversibly.14 Its first use was in whole organ, namely kidney and heart transplants, to avoid transplant rejection by modulating the host’s immune response.14
Though available in many forms, topical cyclosporine is an established treatment for keratoconjunctivitis sicca. Although the exact concentration of the topical form is up for debate, commercially available 0.05% cyclosporine has been shown to be effective in managing allergic cases in which management requires a steroid.15
Related: New cyclosporine therapy joins the fight against dry eye disease
This can prove to be useful in chronic allergic disease such as vernal keratoconjunctivitis or atopic keratoconjunctivitis where chronic treatment is required. Clinically, it can be useful to pulse a steroid when initially treating with cyclosporine in cases where long-term management is foreshadowed. Prolonged treatment with QID dosing of cyclosporine 0.05% has been proven safe and effective in vernal keratoconjunctivitis.16 Restasis (cyclosporine 0.05%, Allergan) is an easy formulation that you may find yourself reaching for off-label.
Recent phase 3 study results have demonstrated Cequa (Sun Pharma), a 0.09% formulation of cyclosporine, to be effective in management of keratoconjunctivitis sicca. Though an off-label use, this could be a potential concentration to turn to when 0.05% is not quite potent enough.17
Tacrolimus: Pump up the volume
Like cyclosporine, tacrolimus was first used in organ transplants to prevent transplant rejection, however; unlike cyclosporine, it is a macrolide that is made via fermentation of Japanese soil containing the bacteria Streptomyces tsukubaensis.18
It works via inhibiting the production of IL-2, a cytokine key in the proliferation of T cells.18 It is also a calcineurin receptor antagonist with analogous mechanism of action to cyclosporine but with greater potency.18
Dermatological use is common in ointment form in atopic conditions such as eczema or allergic dermatitis; so, promise has been there for topical use for allergic eye disease.
Related: Experts offer top allergy tips
Along with impinging on cellular communication and activation of lymphocytes, tacrolimus reduces the signs and symptoms of ocular allergy by working on the activation and release of mast cells and histamine.19
Research has shown that tacrolimus 0.03% is efficacious, safe, and well tolerated in the treatment of allergic eye disease.19 It has been indicated in reducing recurrences of exasperations of allergic disease.20
There are no current topical formations approved by the FDA for ophthalmic use; however, Protopic (0.03%, Astellas Toyama Co., Ltd) may be used off-label by applying to the inferior conjunctival fornix.
New research in murine models has shown promising results for a biodegradable, sustained-released, tacrolimus micro-film use in chronic allergic ocular disease. Microfilms loaded with tacrolimus were found to have good biocompatibility, desirable drug delivery, and equivalent efficacy to conventional tacrolimus drops.21
These new delivery systems not only allow for safety in long-term management but provide more convenient regimens for patients which may improve compliance.
References:
1. American College of Allergy, Asthma, and Immunology. Allergy Facts. Available at: https://acaai.org/news/facts-statistics/allergies. Accessed 9/18/18.
2. Leonardi A. Allergy and allergic mediators in tears. Exp Eye Res. 2013 Dec;117:106-17.
3. Stull C, Valdes-Rodriguez R, Shafer BM, Shevchenko A, Nattkemper LA, Chan YH, Tabaac S, Schardt MJ, Najjar DM, Foster WJ, Yosipovitch G. The prevalence and characteristics of chronic ocular itch: a cross-sectional survey. Itch (Phila). 2017 Mar;2(1):e4.
4. Galor A, Small L, Feuer W, Levitt RC, Sarantopoulos KD, Yosipovitch G. The relationship between ocular itch, ocular pain, and dry eye symptoms (An American Ophthalmological Society Thesis). Trans Am Ophthalmol Soc. 2018 Jan 17;115:T5.
5. Chigbu DI. The pathophysiology of ocular allergy: A review. Cont Lens Anterior Eye. 2009 Feb;32(1):3-15.
6. Chigbu DI, Minhas B. Immunopathology of allergic conjunctivitis. EMJ. 2018 Mar;3(1):76-83. 7. Dordal MT, Lluch-Bernal M, Sánchez MC, Rondón C, Navarro A, Montoro J, Matheu V, Ibáñez MD, Fernández-Parra B, Dávila I, Conde J, Antón E, Colás C, Valero A; SEAIC Rhinoconjunctivitis Committee. Allergen-specific nasal provocation testing: review by the rhinoconjunctivitis committee of the Spanish Society of Allergy and Clinical Immunology. J Investig Allergol Clin Immunol. 2011;21(1):1-12.
8. Zheng X, Yao J, Li B. Expression of TSLP and downstream molecules IL-4, IL-5, and IL-13 on the eye surface of patients with various types of allergic conjunctivitis. J Ophthalmol. 2016;2016:5072781.
9. Leonardi A. The central role of conjunctival mast cells in the pathogenesis of ocular allergy. Curr Allergy Asthma Rep. 2002 Jul;2(4):325-31.
10. Bielory L, Bonini S, Bonini S. Allergic eye disorders. In: Inflammatory mechanism in allergic diseases. Eds: Zweiman B, Schwartz LB. New York: Marcel Dekker, 2002. 311-323.
11. Pattnaik L, Acharya L. A comprehensive review on vernal keratoconjunctivitis with emphasis on proteomics. Life Sci. 2015 May 1;128:47-54.
12. Bonini S, Lambiase A, Sgrulletta R, Bonini S. Allergic chronic inflammation of the ocular surface in vernal keratoconjunctivitis. 2003. Curr Opin Allergy Clin Immunol. 2003 Oct;3(5):381-7.
13. Wilson SR, Thé L, Batia LM, Beattie K, Katibah GE, McClain SP, Pellegrino M, Estandian DM, Bautista DM. The epithelial cell-derived atopic dermatitis cytokine TSLP activates neurons to induce itch. Cell. 2013 Oct 10;155(2):285-95.
14. Colombo D, Ammirati E. Cyclosporine in transplantation – a history of converging timelines. J Biol Regul Homeost Agents. 2011 Oct-Dec;25(4):493-504.
15. Akpek EK, Dart JK, Watson S, Christen W, Dursun D, Yoo S, O’Brien TP, Schein OD, Gottsch JD. A randomized trial of topical cyclosporine 0.05% in topical steroid-resistant atopic keratoconjunctivitis. Ophthalmology. 2004 Mar;111(3):476-482.
16. Yücel OE, Ulus ND. Efficacy and safety of topical cyclosporine A 0.05% in vernal keratoconjunctivitis. Singapore Med J. 2016 Sep;57(9):507-10.
17. Luchs J. Phase 3 clinical results of cyclosporine 0.09% in a new nanomicellar ophthalmic solution for treatment keratoconjunctivitis sicca. Presented at: American Society of Cataract and Refractive Surgery annual meeting; April 13-17, 2018; Washington, DC.
18. Almawi WY, Melemedjian OK. Clinical and mechanistic differences between FK-506 (tacrolimus) and cyclosporine A. Nephrol Dial Transplant. 2000 Dec;15(12):1916-8.
19. Attas-Fox L, Barkana Y, Iskhakov V, Rayvich S, Gerber Y, Morad Y, Avni I, Zadok D. Topical tacrolimus 0.03% ointment for intractable allergic conjunctivitis: an open-label pilot study. Curr Eye Res. 2008 Jul;33(7):545-9
20. Hazarika AK, Singh PK. Efficacy of topical application of 0.03% tacrolimus eye ointment in the management of allergic conjunctivitis. J Nat Sci Biol Med. 2015 Aug;6(Suppl 1):S10-2.
21. Liu YC, Ng XW, Teo EPW, Ang HP, Lwin NC, Chan NSW, Venkatraman SS, Wong TT Mehta JS. A biodegradable, sustained-released, tacrolimus microfilm drug delivery system for the management of allergic conjunctivitis in a mouse model. Invest Ophthalmol Vis Sci. 2018 Feb 1;59(2):675-684.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.