Why ODs shouldn’t stop short with patient care
ODs strive to always focus on managing the contact lens patient. But sometimes they are tempted to stop shy of 100 percent, especially once a patient’s complaints have quieted. Here’s one such example.
Patient CA presented as a new patient six weeks ago with complaints of mild light sensitivity in both eyes for the past several years. The photosensitivity is constant-but much worse outside-and she needs to wear sunglasses if it is daylight.
Her medical history is unremarkable. She takes birth control pills and 800 mg ibuprofen prn (Advil, Pfizer). She wears Acuvue Vita (Johnson & Johnson Vision) from 7 a.m. to 11 p.m., disposes them monthly, and “never” wears her prescription glasses.
She uses OptiFree Replenish Multi-Purpose Disinfecting Solution (Alcon) for contacts twice a day before contact lens insertion and after removal. CA works on the computer at least 10 hours per day and complains that her eyes are dried out and irritated by evening.
Previously by Dr. Brimer: Troubleshoot contact lens discomfort and prevent complications
Optical options
An OD’s first impulse is to scream, “Well, of course!”
Ten hours at the computer with contact lenses could cause anyone to be annoyed. But it was clear there was something more causing the light sensitivity CA was experiencing.
Nonetheless, ODs have to be readily armed to discuss computer habits and computer setup, including distance and height, timing of breaks, and inclusion of blink exercises. Career device users are more and more common, and the time to discuss these things continues to diminish.
I urge ODs to incorporate patient education pieces to do the talking. While these tips are second nature to ODs, it needs to be spelled out to patients. Do not take it for granted that they know how to influence their own work environment in a positive way.
CA was correctable to 20/20 OD, OS with a refraction of OD: -2.50 -0.75 x 175 and OS: -3.00 -0.50 x 147. This 38-year-old patient requested an addition of +1.25 D. However, she denied computer or near strain.
Related: How to recognize and manage digital eye strain
We discussed her optical options to reduce the strain:
• Eyezen lenses (Essilor) for her non-contact lens hours
• A computer pair for screen time
• Distance-vision-only (DVO) contact lenses with plus specs
• Multifocal contact lenses
CA was adamant about staying with her DVO contact lenses-and I was adamant about her moving into a daily disposable wear modality-so we met in the middle.
Related: Experts offer advice on fitting, pricing daily disposables
Evaluation
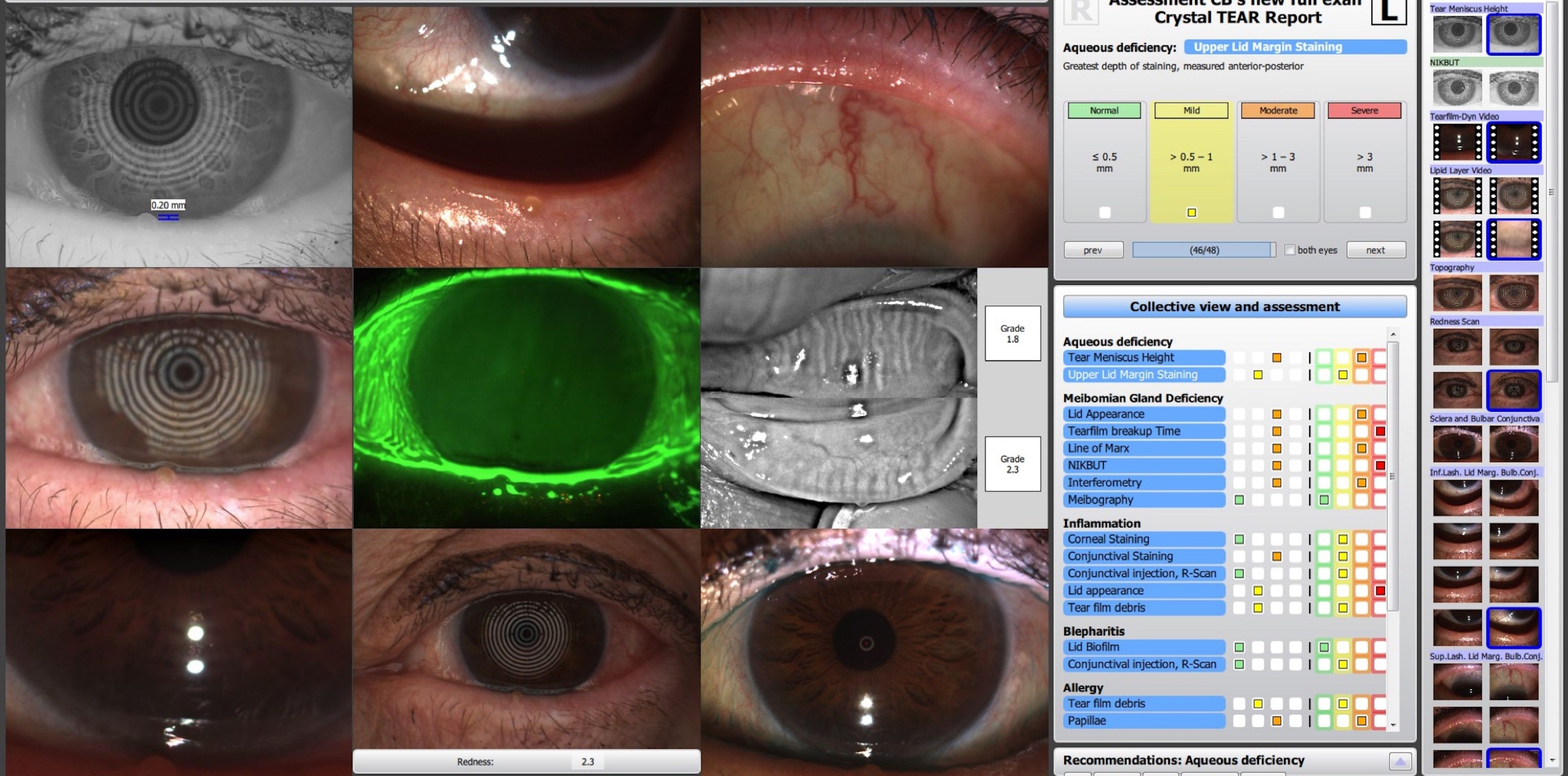
We performed a screening with the Oculus Keratograph 5M. CA’s Crystal tear report screening showed low tear meniscus height, no color on interferometry, and increased hyperemia in both eyes.
The patient was able to see the test results on the printout and understand that her symptoms may be more than just an annoyance. The preliminary slit lamp exam confirmed the findings of the screening, allowing me to facilitate the conversation and recommending that CA return for a full dry eye assessment.
We discussed transitioning to a better contact lens material and shortening her wear time at least by a few hours-a reduction from 16 to 12 hours per day. CA was fit into Dailies Total 1 (Alcon), masking the astigmatism.
We also discussed improving the ergonomics of her workspace, her diet and water intake, and incorporating blink exercises into her routine.
We agreed that the main goal is for her to be able to wear contact lenses for years to come without significant consequence to the ocular surface. I explained that while the current measures will help, we need to explore the underlying challenges causing her to be so photophobic. CA was scheduled for a full dry eye evaluation (DEE) one month later.
Related: Look for small signs to prevent contact lens complications
Follow-up visit
Upon her return, I learned that CA had “felt” her eyes for many years and had told “at least three” other doctors. She listed three brands of contact lenses, three brands of contact lens solutions, and five brands of rewetting drops she had tried during this time.
On a side note, while I am constantly amazed at the volume and variety of eyecare products that I see on the grocery store shelf, I sometimes wonder if consumer availability is a disservice to patients. They go from one product to the next, masking their symptoms, while their underlying problem could be getting worse.
One study showed that 32 percent of patients using tears daily had worse vision after one year.1 Of course, all the blame cannot be placed on CA for her shopping habits because she had given three doctors the chance to guide her to a resolution.
At her DEE, CA noted feeling much better since changing contact lens materials and reducing her wear time slightly. However, I stressed the need to continue with the evaluation.
Related: Blog: Modern-day techniques for diagnosing dry eye disease
CA reported that her eyes felt fine in the morning and mid-day. However, every evening her eyes became bothersome and dry. She complained blinking frequently to see better, and that she felt occasional tearing, grittiness, and burning. Her eyes were very fragile, bothered by wind, air, and smoke. When asked, she revealed that-for the past several years-she has had daily sinus drainage in her throat and fatigue.
Upon lid examination, OD was worse than OS, with moderate lid edema, hyperemia, and telangiectasia noted in both eyes. There was moderate line of Marx staining in both eyes, as well as mild lid wiper epitheliopathy.
CA had moderate tear film debris and a low tear meniscus height of 0.16 mm and 0.18 mm OD, OS. Her osmolarity was 310 and 328, respectively. There was only trace color on interferometry, non-invasive keratography break-up time (NIKBUT) was 10 and 24 seconds, and tear break-up time (TBUT) was 2 and 6 seconds. There was mild corneal haze in both eyes, and grade 2 conjunctival hyperemia, grade 2 papillae OD, grade 2 to 3 papillae OS, and grade 1 conjunctival punctate staining nasally with lissamine green.
Meibomian gland evaluator and manual expression of the lid was unproductive. She exhibited severe meibomian gland truncation and dropout on the right upper and lower lids and moderate loss on upper and lower lids OS.
Related: Why you should add upper eyelid eversion to your comprehensive exam
Surprisingly, only rare partial blinks were documented, and there was no gap on the Korb-Blackie (KB) light test. My assumption is that had she been wearing her contact lenses, I would have video-captured more partial blinks.
CA’s primary challenges were meibomian gland dysfunction (MGD) and inflammation. Her secondary problem was aqueous deficiency and possibly allergies.
Next steps
I spent a few minutes telling CA her story by showing her the pictures on my 5M and discussing treatment options. My recommendations for CA are as follows:
Evacuate the remaining glands with LipiFlow (Johnson & Johnson Vision), then attempt to keep the flow moving via medical grade omegas and daily warm compress for 20 minutes with Tranquileyes (Eye Eco).
I explained that our main goal is to keep the remaining glands from degrading, but LipiFlow will likely have a positive influence on the evening symptoms she experiences. In fact, subjects in Blackie’s 2018 trial were able to increase comfortable wear time by an average of four hours per day within one month after the procedure.2
These recommendations were in addition to the prior ones regarding diet and environment. We discussed the option of implementing a long-term anti-inflammatory treatment but agreed to re-assess the need after her procedure.
Related: How I handled an unusual contact lens request
My other goal in CA’s care is to rule out the influence of allergies on her discomfort. Having post-nasal drip daily for years is a significant symptom to sweep under the rug. I will have her back for in-office percutaneous skin testing with the system from AllerFocus.
We will know in 10 minutes if her allergies are from something that can be avoided or if treatment is indicated. If so, I will prescribe sublingual immunotherapy (SLIT) in order to relieve her symptoms. This will build her tolerance without the drying side effects.
CA ordered new glasses in a frame she loves and will be more motivated to wear. The near add will help with her accommodative challenges. We revisited the computer ergonomics discussion and how taking breaks while wearing her contact lenses will help with the typical accommodative infacility our career device users experience.
CA is on her way to healthy contact lens wear-despite extended device use. It is important to flag patients who have these two major risk factors for gland loss. If she had not had symptoms and returned for the DEE, would this severe gland loss have gone undetected? If we had forgone the DEE because her symptoms improved with the lens change, what would have been missed? Perform routine meibography or at the very least transillumination on these patients-so you can both sleep better at night.
Disclosure: This author is a consultant for OculusRead more by Dr. Brimer
References:
1. Rao SN. Topical cyclosporine 0.05% for the prevention of dry eye disease progression. J Ocul Pharmacol Ther. 2010 Apr;26(2):157-164.
2. Blackie CA, Coleman CA, Nichols KK, Jones L, Chen PQ, Melton R, Kading DL, O’Dell LE, Srinivasan S. A single vectored thermal pulsation treatment for meibomian gland dysfunction increases mean comfortable contact lens wearing time by approximately 4 hours per day. Clin Ophthalmol. 2018 Jan 17;12:169-183.

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.




.png&w=3840&q=75)






















