Zoom out to expand treatment for diabetes patients

While the dilated eye exam has been optometry’s core diabetes responsibility, an epidemic prevalence of diabetes, a state of therapeutic inertia, and greater overall morbidity and mortality from the disease means that ODs must more fully engage in an amplified and targeted challenge of diabetes in the U.S.
As a profession, optometry should push for scope expansion for:
• Injectable authority to accommodate optometry’s increased need for point-of-care testing1 and Clinical Laboratory Improvement Amendments Act (CLIA) certification;2 and providing easier unrestricted patient access to earlier diabetes treatment protocols for anti-VEGF drugs3
• Authorities to perform laser surgery for glaucoma and retinal treatments
Related: How diabetes affects your patients
In addition, optometry must expand relationships and cooperation via:
• Practice alliances focused on diabetes with pediatrics,4 behavioral health, family practice, internal medicine, endocrinology, and nursing
• Adding members to the diabetes team (possibly within your optometry clinic) including but not limited to certified diabetes educator4 and behavioral health specialist-both of whom can be an integral part of the optometry practice team as patients with these services face less stigma and have easier access to appropriate comprehensive diabetes care
• Advanced technologies intersecting optometry and the care of patients with or at risk of diabetes and diabetic eye disease (such as spectral domain optical coherence tomorography [SD-OCT], OCT angiography, nerve fiber analysis [GDx])
• Support and collaboration from all optometry-aligned sectors (housing,5 banking,6 public health,7 emergency preparedness,8 environmental)9 united to a triple bottom line approach that includes health, economy, and environment
Related: Why in-person care and technology must partner
Past success
Although optometry had been participating in the care of patients with diabetes since 1971,10 the profession was not fully recognized as being “official diabetes care providers” until the Diabetes Care Supplement published by the American Diabetes Association (ADA) in January 1995. This publication reset diabetes clinical care recommendations that all providers follow, recommending that “Comprehensive dilated eye and visual examinations should be performed annually by an ophthalmologist or optometrist.”11
This was the very first time the reference “ophthalmologist or optometrist” was used in ADA Clinical Practice Recommendations.
Furthermore, growing U.S. diabetes rates in the 1980s brought new attention to diabetes by the Centers for Disease Control (CDC), which established the CDC Division of Diabetes Translation (DTT) in the 1990s.
Related: New diabetes agents can improve, save patients' lives
Combined with the American Optometric Association’s (AOA) advocacy efforts and new ADA clinical care recommendations, optometry’s place in interprofessional diabetes care was solidified by the CDC/DDT through the establishment of the integrative diabetes practice model, Pharmacy, Podiatry, Optometry and Dentistry (PPOD), in 199912 and the publication Improving the Nation’s Vision Health: A Coordinated Public Health Approach in 2006.13
The CDC, in its most recent diabetes report card (2017) reports that 61.6 percent of Americans adults with diagnosed diabetes received a dilated eye exam from 2014-2015, adding, “The only recommended practice that consistently met or exceeded the Healthy People 2020 target was the dilated eye exam.”14
By many accounts, optometry has traveled far and performed well. ADA’s January 2019 Diabetes Care practice guidelines still reinforces: “Patients with type 1 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist within 5 years after the onset of diabetes. Patients with type 2 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist at the time of diagnosis.”15Related: When to refer patients with diabetic retinopathy
Markers indicating course correction
Optometry’s current position requires a closer look at the data. In fact, the percentage of adults diagnosed with diabetes who had contact with an eye doctor (optometrist or ophthalmologist) during the past 12 months increased with age.16
This trend may be consistent with a prevention focus on the Medicare population, perhaps by clinicians and the Medicare program itself.
National data indicate a recent increase in diabetes complications is most apparent in young adults (aged 18-44 years) and middle-aged adults (aged 45-64 years).17
Optometry aiming its sights toward lower age groups may be in order. For example, among adults age 18-39 who had diabetes, only 35.9 percent reported contact with an eye doctor in the past 12 months.16
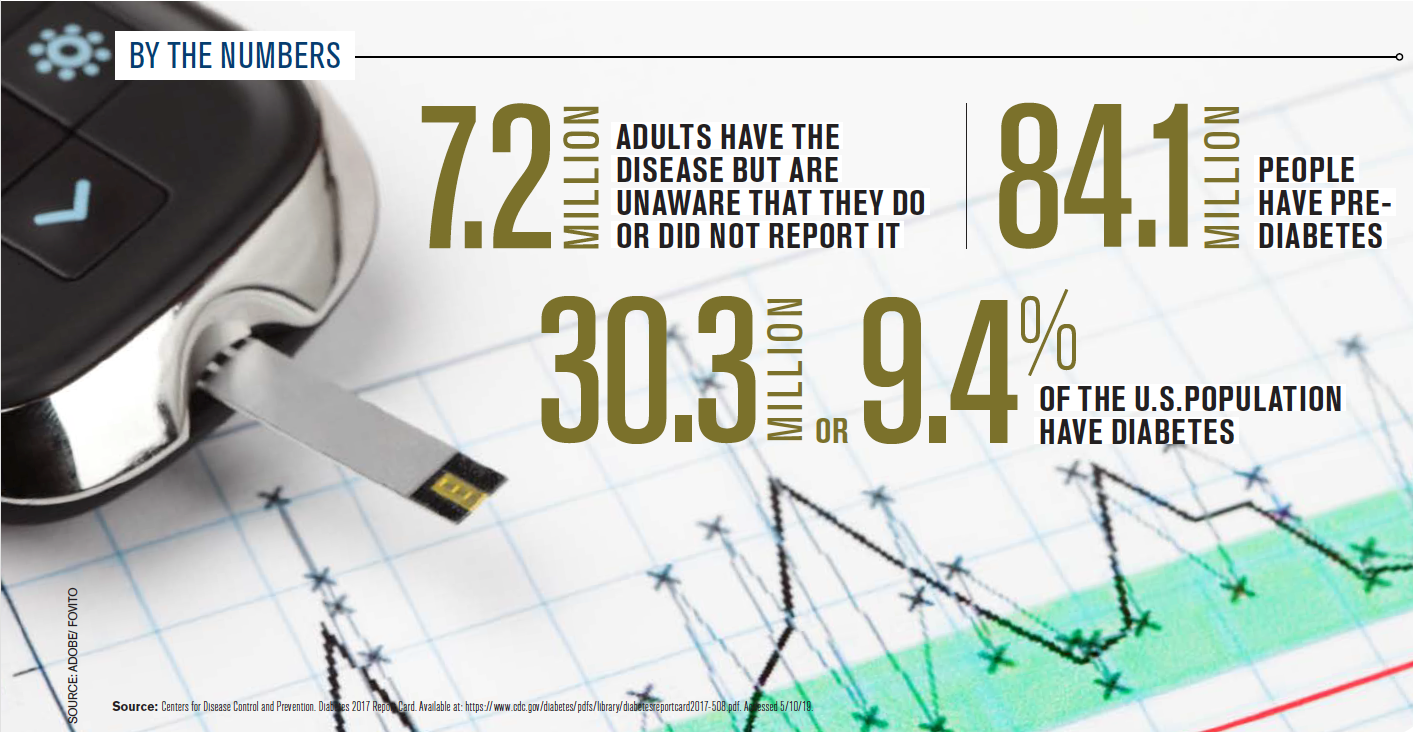
The CDC (2017) estimates 7.2 million adults have diabetes but were not aware they have the disease or did not report they have it and that 84.1 million people have prediabetes.18
These 91.3 million Americans can directly benefit from comprehensive eye examination which can uncover undiagnosed disease. Retinopathy can present itself as an initial indication of overt type 2 diabetes mellitus (T2DM) and other ocular findings (cataract, glaucoma, ocular surface diseases, papillopathy) have been associated with hyperglycemia.19
Related: How to potentially reduce diabetic retinopathy by manipulating microbial species
Additionally, data shows the group with the highest increase of T2DM was children. Importantly, youth-onset type 2 diabetes displays unique aspects, such as rapidly progressive β-cell decline and accelerated development of diabetes complications.20
This increase of T2DM among children is thought to be due to increased screen time, sedentary life style, and higher rates of obesity. Because children suffer higher rates of myopia21 (another epidemic), optometry is perfectly poised to accommodate assisting early diagnosis of both diseases during the comprehensive eye examination.
Optometry’s diabetes information come from several sources:
• ADA
• Diabetes Advocacy Alliance (DAA)22
• U.S. Congressional Caucus on Diabetes
• AOA Health Policy Institute (HPI)23
Combined, these four sources can inform optometry of impending threats and opportunities.
For example, an opportunity came in November 2018 with the start of an ADA multi-year campaign to reduce therapeutic inertia (clinician failure to initiate or intensify treatment) in the management of type 1 and type 2 diabetes. AOA was one of 100 organizational members-and the only eyecare provider group-of the diabetes ecosystem assembled for the opening ADA Therapeutic Inertia Summit.
Related: The importance of multidisciplinary care for diabetes
Optometry has a role to play in this ADA campaign as the summit outcomes inform the profession’s course. They reveal:24
• Unacceptable levels of diabetes morbidity and mortality, especially with respect to T2DM
• Intensive treatment leads to better microvascular status (37 percent for microvascular complications such as retinopathy)
• At the time of T2DM diagnosis, 87 percent of individuals will have another disease
• Time and treatment barriers ( 56.9 percent inadequate therapy, 14.9 percent non-adherent) to effective diabetes care can be countered by upscaling the role of the primary-care team members (this includes ODs)
Per the DAA, prevention of type 2 diabetes is a policy priority because slowing the number of new cases of diabetes and providing education to empower individuals with or at risk of diabetes is vital to decreasing the human and economic burden of the disease in America.22 Note that the AOA has been a DAA member since the organization’s inception.
Optometry is part of, and informed by, combined advocacy for medical nutrition therapy, Medicare Diabetes Prevention Program (MDPP), National Diabetes Prevention Program (NDPP), and Diabetes Self-Management Education and Support (DSMES).
Related: Role of insulin therapy in diabetes and diabetic retinopathy
Similarly, the large, 313 member, U.S. Congressional Caucus on Diabetes activities are important to monitor. Its goal is to ensure diabetes is adequately addressed in all relevant legislation and regulations-and its actions can change often.
Finally, HPI offers research and analysis focused on eye health and vision care with policy briefs that often intersect with diabetes care.25
Optometry’s future in diabetes care
Simply put, optometry will move beyond retinopathy.4 Optometry will play a greater role in assisting patients’ glycemic control, their attainment of suitable body mass index, reduction of behavioral and cardiovascular risk factors, and avoidance of progressive retinopathy, diabetic macular edema, glaucoma, cataract, neuropathies, and nephropathy.4
Doctors of optometry must be resolute with the knowledge, optometry’s course is not constrained by diabetes; rather, diabetes is contained within the navigable waters optometry can sail. Armed with this knowledge, ODs will continue go farther and do good. In fact, optometry’s 2021 turning point, marking the 50th year of the diabetes care journey, is up to you.
Read more diabetes content here
About the authorDr. Dueñas has a wide background in private and hospital-based optometry practice and interdisciplinary teaching and service to the U.S. Centers for Disease Control and Prevention (CDC). He is immediate past chair of the Patient Centered Outcomes Research Institute (PCORI), Advisory Panel on Improving Healthcare Systems. In his free time, Dr. Dueñas enjoys sailing with his wife and completed a 900-nm ocean passage from Spain to Africa, sailing a 57-foot cutter rigged sloop. Opinions expressed are those of the author and may not necessarily reflect those of the AOA or its affiliates.
MDuenas@aoa.org
References:
1. Brown JB. Point-of-Care Testing in Diabetes Management: What Role Does It Play? Diabetes Spectrum. 2004 Oct; 17(4):244-248.
2. Centers for Medical & Medicaid Services. Clinical Laboratory Improvement Amendments (CLIA). Available at: https://www.cms.gov/Regulations-and-Guidance/Legislation/CLIA/index.html?redirect=/Clia/. Accessed 5/10/19.
3. ClinicalTrials.gov. Study of the Efficacy and Safety of Intravitreal (IVT) Aflibercept for the Improvement of Moderately Severe to Severe Nonproliferative Diabetic Retinopathy (NPDR) (PANORAMA). Available at: https://clinicaltrials.gov/ct2/show/NCT02718326. Accessed 5/10/19.
4. Pinkston W. 21st century optometric care for the 21st century pandemic. AOA Focus. Available at: http://aoa.uberflip.com/i/1056416-the-great-diabetes-pandemic. Accessed 5/10/19.
5. Lloyd PC, Helms VE, Simon AE, Golden C, Brittain J, Call, E, Mirel LB, Steffen BL, Sperling J, Rudd EC, Parker JD, Star, CS. Linkage of 1999–2012 National Health
Interview Survey and National Health and Nutrition Examination Survey Data
6. Community Development Innovation Review. Federal Reserve Bank of San Francisco. Available at: https://www.frbsf.org/community-development/files/mental-health-and-community-development-cdir-13-1.pdf. Accessed 5/16/19.
7. American Public Health Association. Vision Care. Available at: https://www.apha.org/apha-communities/member-sections/vision-care. Accessed 5/10/19.
8. American Optometric Association Health Policy Institute. Issue Brief: Doctors of Optometry in Disaster Preparedness, Response, and Recovery. Available at: https://www.aoa.org/documents/HPI/Disaster%20Draft%20Brief%20HPI%20FINAL%2010.04.17_lg.pdf. Accessed 5/10/19.
9. United States Environmental Protection Agency. Federal Interagency Working Group on Environmental Justice (EJ IWG). Available at: https://www.epa.gov/environmentaljustice/federal-interagency-working-group-environmental-justice-ej-iwg. Accessed 5/10/19.
10. Bennett I. A Witness to History. Review Optom. Available at: https://www.reviewofoptometry.com/article/a-witness-to-history. Accessed 5/10/19.
11. American Diabetes Association. Standards of Medical Care for Patients with Diabetes Mellitus. Diabetes Care. 1995 Jan;18 (Supplement 1):8-15.
12. Rodgers P, Bennet PW, Frisch DR, Ball WL, Chous P, Gerson J, Primo S, Furnari W, Gillis M, Novak K, Tayor G. Working Together to Manage Diabetes: A Guide for Pharmacy, Podiatry, Optometry, and Dentistry. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/diabetes/ndep/pdfs/ppod-guide.pdf. Accessed 5/10/19.
13. Centers for Disease Control and Prevention. Improving the Nation’s Vision Health: A Coordinated Public Health Approach. Available at: https://www.cdc.gov/visionhealth/pdf/improving_nations_vision_health_508_final.pdf. Accessed 5/10/19.
14. Centers for Disease Control and Prevention. Diabetes Report Card 2017. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2018.
15. American Diabetes Association. Standards of Medical Care in Diabetes-2019. Diabetes Care. 2018 Jan;42 (Supplement 1):S1-S2.
16. Villarroel MA, Vahratian A, Ward BW. Health Care Utilization Among U.S. Adults With Diagnosed Diabetes, 2013. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/nchs/data/databriefs/db183.pdf. Accessed 5/10/19.
17. Gregg EW, Hora I, Benoit SR. Resurgence in Diabetes-Related Complications. JAMA. 2019 Apr 15. doi: 10.1001/jama.2019.3471. [Epub ahead of print]
18. Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Availabe at: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed 5/16/19.
19. Sayin N, Kara N, Pekel G. Ocular complications of diabetes mellitus. World J Diabetes. 2015 Feb 15;6(1):92-108.
20. Nadeau KJ, Anderson BJ, Berg EG, Chiang JL, Chou H, Copeland KC, Hannon TS, Huang TT, Lynch JL, Powell J, Sellers E, Tamborlane WV, Zeitler P. Youth-Onset Type 2 Diabetes Consensus Report: Current Status, Challenges, and Priorities. Diabetes Care. 2016 Sep;39(9):1635-1642.
21. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016 May;123(5):1036-42.
22. Diabetes Advocacy Alliance. Prevention. Available at: https://www.diabetesadvocacyalliance.org/html/policy_prevention.html. Accessed 5/10/19.
23. American Optometric Association. Health Policy Institute. Available at: https://www.aoa.org/hpi. Accessed 5/10/19.
24. American Diabetes Association. Summary of Proceedings of the American Diabetes Association Summit. Overcoming Therapeutic Inertia: Accelerating Diabetes Care FOR_LIFE. Available at: https://professional.diabetes.org/sites/professional.diabetes.org/files/media/ada_therapeutic_inertia_interior_final.pdf. Accessed 5/10/19.
25. American Optometric Association Health Policy Institute. Doctors of Optometry Increase Primary Eye Care at Health Centers. Available at: https://www.aoa.org/documents/HPI/HPI%20Health%20Centers_Doctors%20of%20Optometry_2019REV.pdf. Accessed 5/10/19.

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.