How to create an ocular surface disease treatment protocol
OSD treatments are rarely straightforward because of its complex, multifactorial nature.


Developing an ocular surface disease treatment plan is an involved process because it entails the consideration of overlapping diagnoses, including dry eye disease, ocular allergy, and blepharitis/meibomian gland disfunction. Three published, preoperative treatment protocols are described here that can help ODs develop rewarding treatment plans on a case-by-case basis, once disease severity and surgical outcomes have been assessed.
You have seen the patient for her dry eye evaluation. You have biomicroscopy findings, ancillary testing, maybe an InflammaDry (Quidel) and osmolarity (TearLab Osmolarity Test) result to consider, in addition to her history. You may have imaging, a best-corrected visual acuity, and a questionnaire to help direct you.
But where do you go from there?
Related: Your glaucoma patients also have ocular surface disease
I am often asked for a treatment protocol. Because ocular surface disease is multifactorial, the treatment is rarely straightforward. Because ocular surface disease (OSD) can be challenging, several published protocols deserve attention. These include the Tear Film & Ocular Surface Society Dry Eye Workshop, second edition (DEWS II), the Cornea External Disease and Refractive Society (CEDARS) treatment algorithm, and the American Society of Cataract and Refractive Surgery (ASCRS) Preoperative treatment protocol.1-3
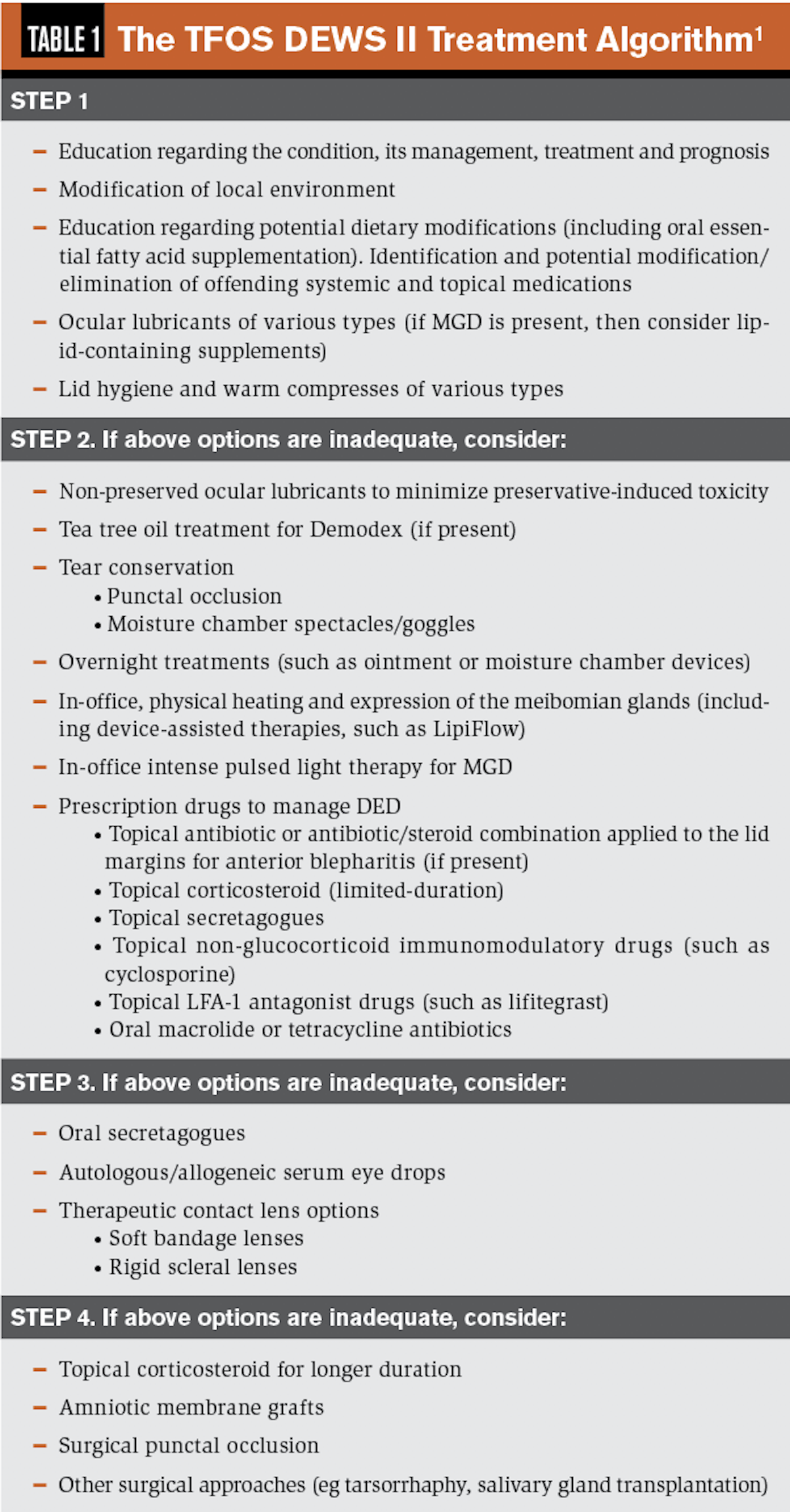
DEWS II protocol
The DEWS II protocol1 is a staged management algorithm in which treatment options are listed in order of disease severity. The recommendations for treatment of tear insufficiency and lid disease may include over-the-counter (OTC) preparations, topical immunomodulators, oral medications, topical steroids, complementary medicines, dietary changes, contact lenses, and surgical options.
This protocol is based upon subtyping and determination of disease severity. Using appropriate tests, first determine if the patient suffers more from aqueous deficient or evaporative dry eye, then consider the severity of the disease. Treatment is performed to restore homeostasis of the ocular surface.
Related: Do ODs take chronic inflammation seriously?
Mild disease is managed using patient education, environmental modification, omega-3 supplementation, lubricants, and lid treatments. Moderate disease steps up the lubricants to preservative-free preparations, gels and ointments; more targeted lid treatments such as tea tree oil; in-office treatments such as LipiFlow (Johnson & Johnson Vision) and intense pulsed light (IPL) therapy; punctal occlusion; and prescription medications (Restasis [cyclosporin, Allergan], Xiidra [lifitegrast, Novartis], Cequa [cyclosporin, Sun Pharma]).
More severe disease not resolving with these techniques may require autologous serum, oral secretagogues to increase lacrimation, and use of contact lenses. When these fail, the last level of treament recommendations include chronic steroids, amniotic membranes, surgical occlusion, and other surgeries.
Related: Experts offer advice to ODs starting dry eye subspecialty
Surgical approaches for severe dry eye not responding to treatment include a temporary or permanent tarsorrahaphy; conjunctivochalasis repair; corneal treatment of epitheliam basement membrane dystrophy (EBMD); Botox (onabotulinumtoxinA injection, Allergan) for blepharospasm; lid surgery for dermatochalsis; blepharotoptosis; conjunctival surgery for pterygium or pingueculae, Stevens-Johnson syndrome and pemphigoid; amniotic membrane grafts; and salivary gland transplantation.
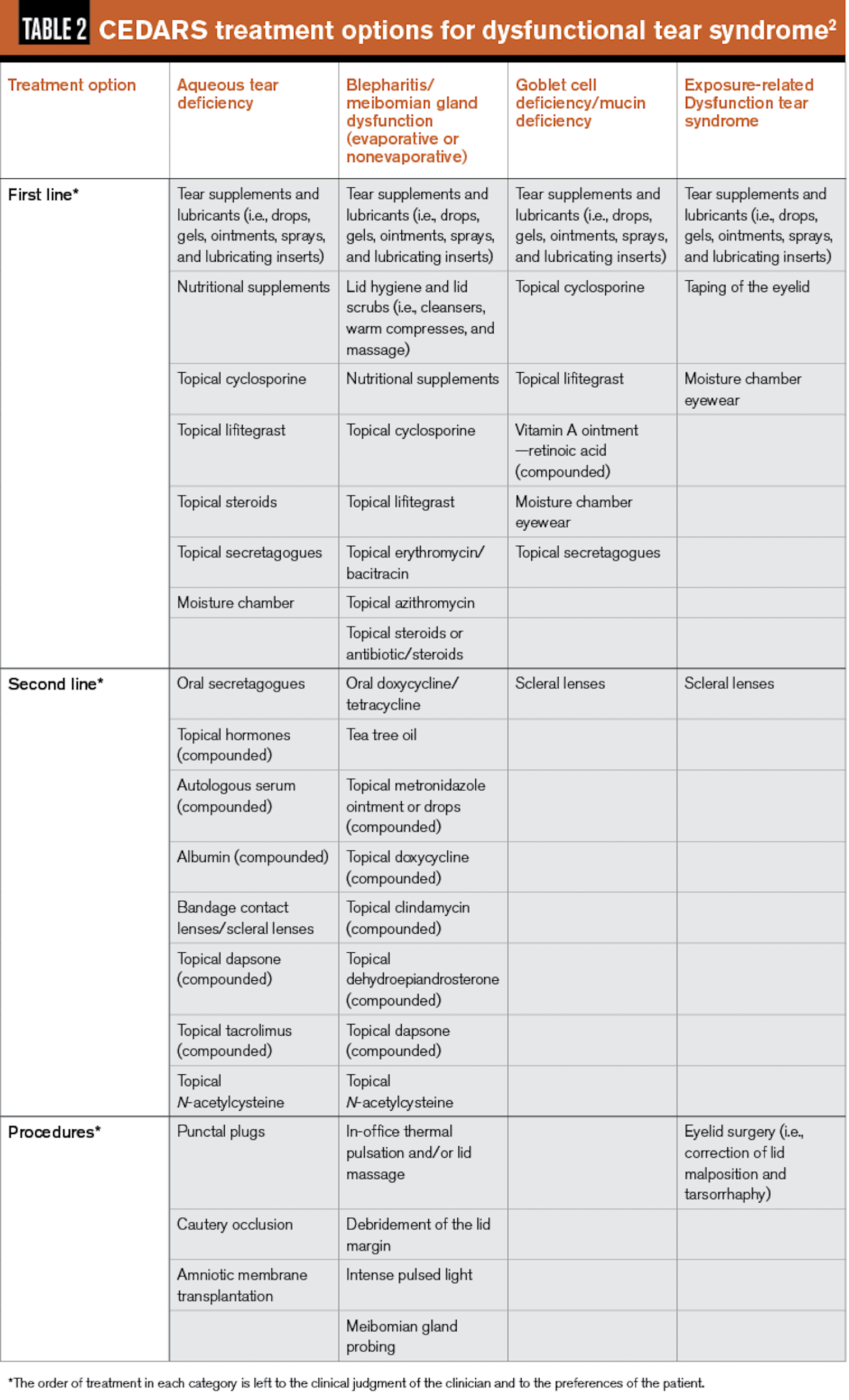
CEDARS algorithm
The CEDARS treatment algorithm2 is slightly different in that it considers the type of evaporative disease. It features more diagnostic categories-aqueous deficiency is one category, but evaporative is broken into goblet cell or mucin deficiency, blepharitis, and exposure-related dry eye.
Once you determine the category, then treatment is directed by severity level. (See Table 2 for more specifics.)
Related: New guidelines in OSD evaluation before surgery
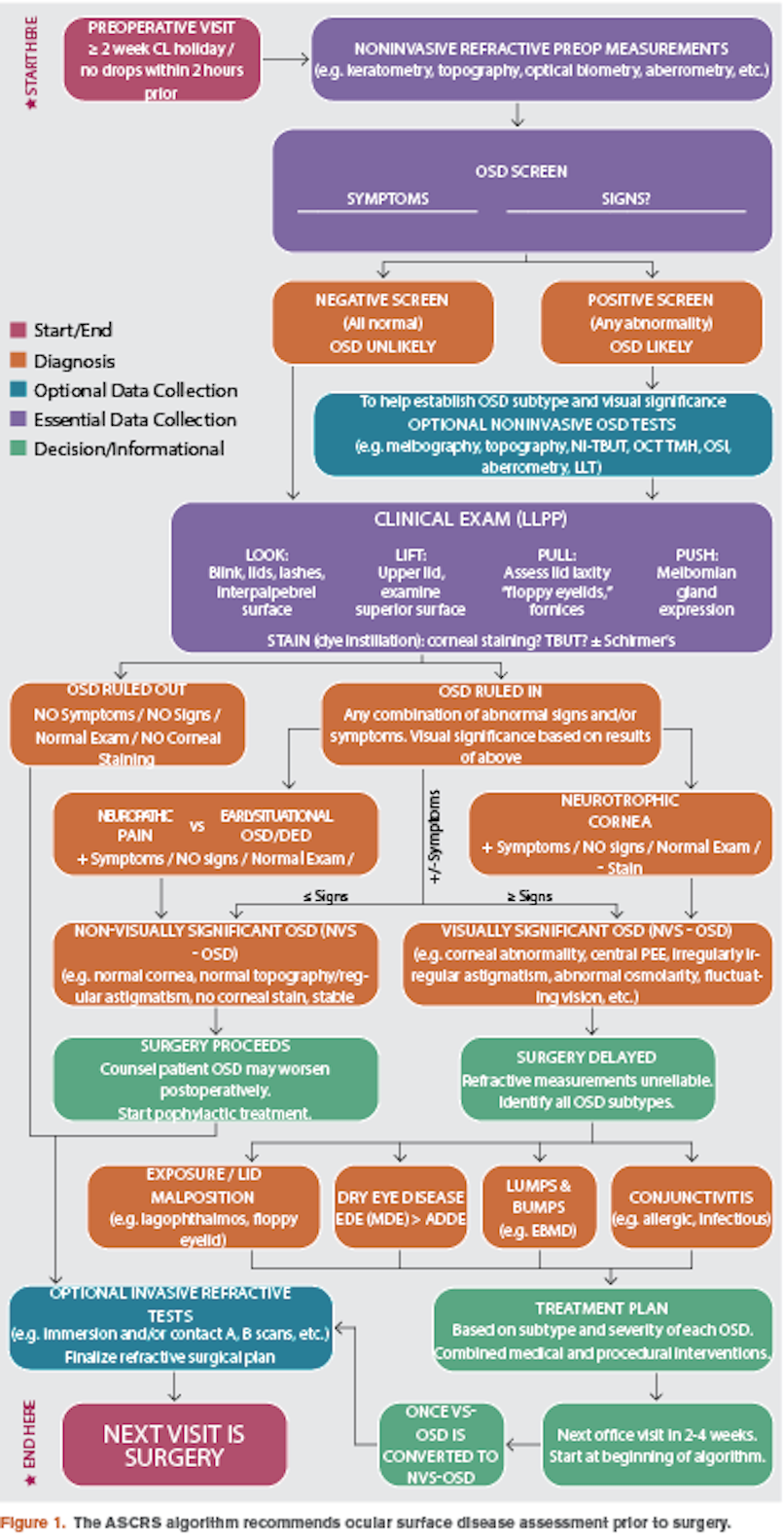
ASCRS algorithm
The ASCRS Preoperative OSD Algorithm recommends assessment of ocular surface disease prior to performing ocular surgery.3 It starts at a “preoperative visit” in which preliminary testing may reveal a compromised ocular surface which can negatively affect surgical outcome (Figure 1).
This algorithm is obviously directed toward surgical interventions such as cataract or vision correction surgery, but it may be applicable to contact lens fitters, helping clinicians know when to trust their refractions, and aid technical staff in understanding their roles in OSD diagnosis and management.
Related: Common systemic conditions associated with dry eye disease
Surgical evaluation typically begins with testing: topography, biometry, aberrometry, and autorefraction. If these tests suggest a compromised ocular surface, a questionnaire regarding OSD symptomatology is given, and osmolarity and MMP-9 levels are measured by the technician. If these are significant for OSD, the patient “fails.” Further diagnostic testing may be performed prior to the doctor’s evaluation.
When the patient sees the doctor, the examination is performed with categoric placement in mind: OSD is present and should be addressed prior to surgery, or no OSD and the patient may proceed with surgery.
For those in the OSD category, neurotrophic disease with significant clinical signs is separated from the usually less severe neuropathic, “more symptoms than clinical signs” type.
Related: Novel drugs + delivery systems ease ocular pain and inflammation
Once grouped, visual significance of the disease is considered. Those with more clinical signs and vision loss require treatment prior to surgery; those with no visual loss and minimal clinical signs with some symptoms may proceed with surgery.
Treatment is directed by subtyping: lid abnormalities, corneal abnormalities (EBMD, Salzmann’s nodules, pterygium), and conjunctival problems (allergic conjunctivitis, chalasis, pingueculitis).
Related: Offer IPL as a treatment for MGD and dry eye disease
Enough already: What do I do?
Personally, I lean toward categorizing the etiology of the most significant complaint, determining what is causing the patient’s symptoms, and treating her according to severity.
In primary-care settings, I inquire about symptoms early in my history discussion. “Do your eye get tired or red? Do they bother you?”
When I perform biomicroscopy, I ask questions based upon what I see. For example, if I see significant lid disease, I may ask, “Do your eyes feel dry or sticky when you wake up?” or “Have you had styes before?”
If I note asymmetry between the two eyes, I ask, “Does the (worse eye) bother you more?”
The impact of asking about symptoms while you examine the eyes, and linking your clinical impression to patient symptoms, can impact the patient’s impression of you as a doctor.
Related: Minimize symptoms of dry eye disease in refractive surgery patients
Following my examination, I consider the patient’s symptoms relative to the clinical picture as well as disease severity. I develop a treatment plan that addresses her primary symptom because I think that the patient is more likely to return for follow-up as well remain compliant with the recommended treatment if the primary symptom improves.
For example, if the initial complaint is primarily pain, I include topical nonsteroidal anti-inflammatory drugs (NSAIDs) in my plan. If it is primarily itching, I include a topical anti-allergy. If it is primarily redness or generally inflammatory, I include a steroid.
Related: Recognize signs and treatment for patients with persistent PSP
I present treatment plans with trade medications. In the OSD “game,” I think trade medications are less problematic than generics. If the patient is unable to afford the trade medications, I will switch to generic with a comment that this medication may not work as well as the one I preferred.
I live in the Tennessee Valley where there are more plant species than anywhere else in the U.S. Patients here often experience allergies.
More than once, I have had a patient insist the problem is allergies, essentially demanding an anti-allergy medication. In many of these cases, I knew from my exam the problem was not allergy because I found EBMD, severe keratitis, conjunctival chalasis, pingueculitis, or Salzmann’s degeneration, for example.
When a patient presents with a strong belief that his problems are due to allergies, I may venture away from these protocol recommendations. If the patient voices concern over my treatment plan and strongly thinks that a particular treatment is the best option, I may try “his” treatment. I have the patient back quickly, usually in two to three weeks, to how “his” treatment is going.
If symptoms improve, the patient appreciates my willingness to listen. If it does not work, I gently reiterate that I was not sure it would work and I would like to try “my” treatment to see if I can improve symptoms more quickly. Typically, the patient is much more compliant with my treatment plan and will improve.
Read more by Dr. Swartz: Offer support to patients with inherited eye diseases
References:
1. Jones L, Downie LE, Korb D, Benitez-Del-Castillo JM, Dana R, Deng SX, Dong PN, Geerling G, Hida RY, Liu Y, Seo KY, Tauber J, Wakamatsu TH, Xu J, Wolffsohn JS, Craig JP. TFOS DEWS II management and therapy report. Ocul Surf. 2017 Jul;15(3):575-628.
2. Milner MS, Beckman KA, Luchs JI, Allen QB, Awdeh RM, Berdahl J, et al. Dysfunctional tear syndrome: dry eye disease and associated tear film disorders – new strategies for diagnosis and treatment. Curr Opin Ophthalmol. 2017 Jan;27 Suppl 1:3-47.
3. Starr CE, Gupta PK, Farid M, Beckman KA, Chan CC, Yeu E, Gomes JAP, Ayers BD, Berdahl JP, Holland EJ, Kim T, Mah FS; ASCRS Cornea Clinical Committee. An algorithm for the preoperative diagnosis and treatment of ocular surface disorders. J Cataract Refract Surg. 2019 May;45(5):669-684.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.