Your glaucoma patients also have ocular surface disease
Employ treatment strategies that control both conditions with less reliance on drops.

S. Wade Kimmell, OD, is part of an OD-MD practice in Indianapolis

Figure 1. Dr. Kimmell ready to place cryo-preserved amniotic membrane (CAM). He expects the patients will have a reduction in symptoms for five to seven months.

Figure 3. A technician performs TearLab osmolarity testing.

Figure 4. A technician performs InflammaDry testing.

Figure 5. Prokera ready for insertion to treat inflammation, as measured by InflammaDry, seen in background.
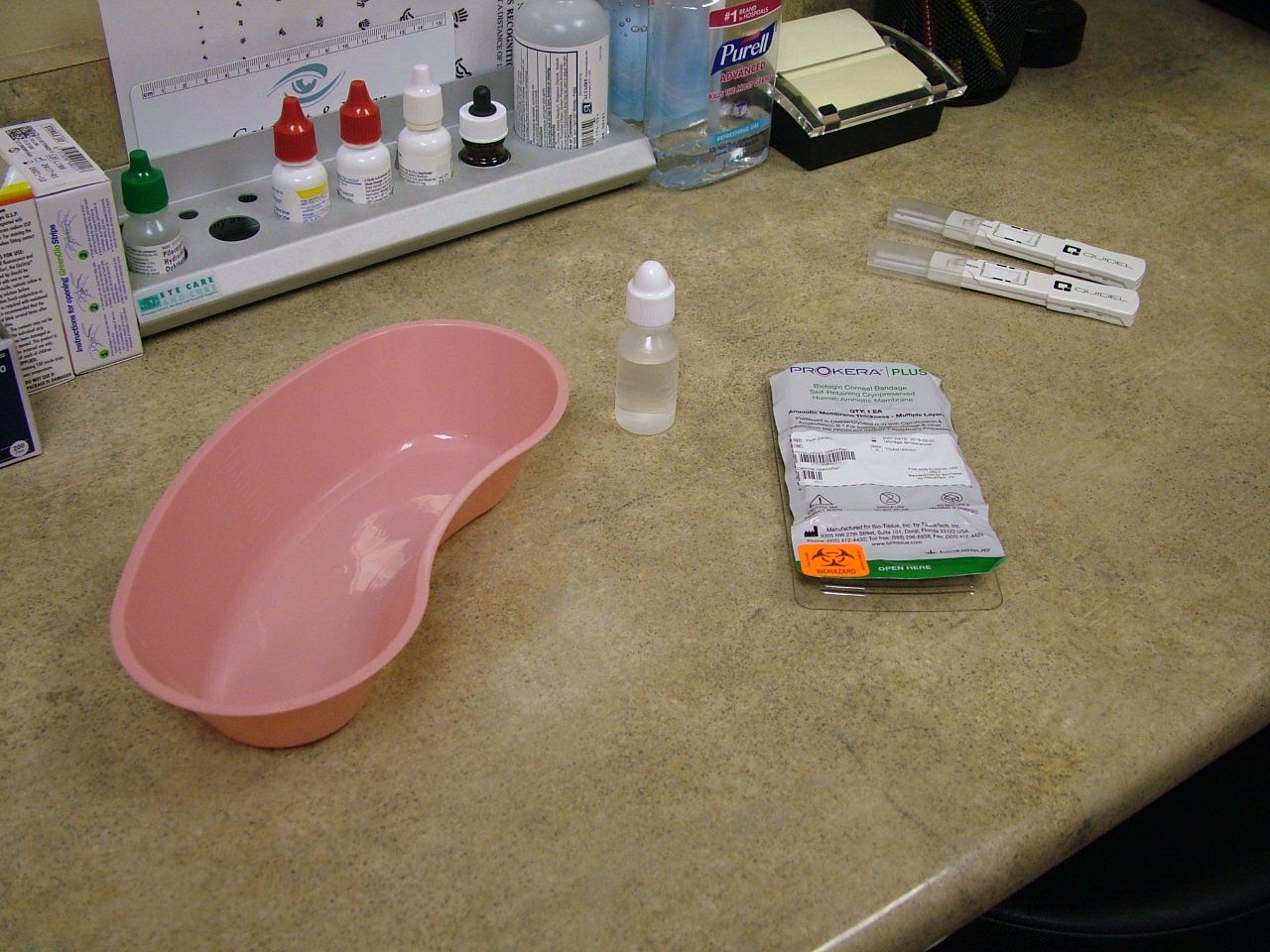
Reducing the medication burden on patients is important for compliance and overall quality of life, and helps to strengthen doctor–patient relationships. Use of the Prokera cryo-preserved amniotic membrane, in conjunction with new imaging technologies, can reduce dry eye symptoms for five to seven months.
It is a fact: glaucoma patients are dry eye patients. Think about it. How many of your glaucoma patients don’t complain of dry-eye-related symptoms?
Glaucoma affects nearly 3 million Americans, including one in 50 people aged 40 years and older, according to the American Academy of Ophthalmology. Worldwide, an estimated 76 million people will have the disease in 2020. Many patients with glaucoma have signs and symptoms of ocular surface disease (OSD)-according to one study, about 56.9 percent of women and 45.7 percent of men.1
Related: Go beyond fish oil with astaxanthin in krill oil
Considering that both glaucoma and OSD occur more often as patients age, and the most common form of treatment for glaucoma are drops presesrved with benzalkonium chloride (BAK), this information is not a surprise. ODs have grown accustomed to seeing glaucoma patients with their injected conjunctivae and keratitis.
When treating glaucoma, ODs make every effort to control patients’ intraocular pressure (IOP) with as few drops and medications as possible. Practitioners dislike adding a twice-daily drop to an at-night drop and hate adding a third drop, knowing that each drop erodes compliance.
Complex drug dosing regimens are a significant barrier to patients’ adherence to therapy.2,3 For glaucoma in general, patients’ lack of compliance ranges from 23 percent to as high as 60 percent.4-8
Click here to watch a video related to this article
Related: Look at more than the optic nerve head in glaucoma patients
Compliance matters
Think about how this changes when it comes to OSD patients. Practitioners prescribe as if patients are compliance superheroes. We put these folks on artificial tears at least four times a day, plus prescription medications like cyclosporine (Restasis, Allergan; Cequa, Sun Pharma; Klarity-C, ImprimisRx) or lifitegrast (Xiidra, Novartis) twice a day, not to mention doxycycline for some.
Related: SD-OCT shows schisis advancements due to sickle cell
We tell them to use heat masks, hot compresses, and other interventions. Then we believe patients will follow through despite all the data to the contrary.
At least OSD patients have the advantage that treatments are likely to help them feel and see better. Unfortunately, this can’t be said for glaucoma patients. No matter how well ODs manage the disease-glaucoma patients can’t actually see or feel the difference. The result is that their disease doesn’t progress, which is not a tangible benefit for the patient.
Innovative paradigm
Related: New guidelines in OSD evaluation before surgery
Optometrists have a great opportunity to treat glaucoma patients’ OSD by offering therapy that provides results they can see and feel. We can get out of our prescribing rut with glaucoma medications by using innovative approaches that are less harmful to the ocular surface as well as incorporating effective therapies to maximize ocular surface health. When their OSD is well controlled, glaucoma patients are happier, which in turn strengthens the doctor-patient relationship.
We can do much to improve our patients’ OSD by altering their glaucoma treatment. Preservatives in glaucoma medications contribute to OSD, with BAK being the most common. As a patient uses more of these preserved medications, their exposure and therefore OSD risk increases. Newer, non-preserved topical glaucoma medications are an alternative, and multiple options exist. Zioptan (tafluprost ophthalmic solution; Merck), Cosopt PF (dorzolamide hydrochloride-timolol maleate ophthalmic solution; Akorn), Timoptic in Ocudose (timolol maleate ophthalmic solution) and Xelpros (latanoprost ophthalmic emulsion) are BAK-free.
Click here to watch a video related to this article
Related: ODs: Redefine your role in glaucoma collaborative care
Another way to reduce preservatives is to eliminate a drop-or drops-entirely. Selective laser trabeculoplasty (SLT) has been available for years but continues to be underutilized. Research suggests evidence for considering laser as first-line treatment, although it estimates that only 15 percent to 20 percent of physicians take this approach.9,10 Even the early Glaucoma Laser Trial (GLT) comparing the use of the old argon laser trabeculoplasty to medications as a first-line treatment found that patients starting with laser had better long-term outcomes than patients starting with medications.11 Patients were also using fewer drops at the end of follow-up.
Related: Common systemic conditions associated with dry eye disease
New developments in treatment are shifting away from topical drops as first-line treatment, replacing them with delivery systems that include punctal plugs, rings, contact lenses, and injections. It should also be routine to consider minimally invasive glaucoma surgery (MIGS) for any glaucoma patient having cataract surgery. The iStent (Glaukos) is FDA-approved only for implantation during cataract surgery; other MIGS devices are available. Xen gel stent (Allergan) and endocyclophotocoagulation (ECP) are options; although all of these are beyond the scope of this article.
Innovative methods
Related: Minimize symptoms of dry eye disease in refractive surgery patients
Of course, some glaucoma patients will require dual and triple anti-hypertensive therapy to control their disease, and the toxic effects will need to be addressed. As with glaucoma therapy, we must consider new ways to treat OSD. Like glaucoma, the first line of treatment for patients with dry eye disease (DED) has been topical drops. In most treatment algorithms, patients start with artificial tears and lubricants; when found ineffective, topical prescription medication would be added.12 Escalating treatment-paralleling glaucoma-would lead to moisture goggles, scleral lenses, autologous serum, and, in the most severe cases, tarsorrhaphy.12,13
These treatments put a heavy burden on patients, especially those who are also being treated for glaucoma. We can expect the compliance on both fronts to suffer, with a negative impact on the efficacy of treatment for both conditions, not to mention the patients’ quality of life.
Click here to watch a video related to this article
Related: Know the hidden links among glaucoma, contact lenses, and the cornea
A fresh approach
With the development of InflammaDry (Quidel) testing for the inflammatory marker MMP-9, TearLab’s tear osmolarity testing, and the LipiScan Dynamic Meibomian Imager (Johnson & Johnson Vision), we can obtain more detailed information regarding patients’ corneal health.
Using these new diagnostic tools combined with our standbys of tear break-up time (TBUT), fluorescein and lisaamine green staining, meibomian gland expression, and a good clinical examination, we can drill down to the root cause of OSD. Gone are the days of every dry eye patient starting on artificial tears. Instead, practitioners tailor treatments to address the components of the disease based on clinical information.
Related: Surgical update 2019: What every OD needs to know
Hitting the market along with these advanced diagnostics are the additional topical therapies lifitegrast (Xiidra, Novartis) and new higher-concentration cyclosporine 0.09% (Cequa, Sun Pharma). Plus, practitiones can opt for procedures to treat dry eye like LipiFlow (Johnson & Johnson Vision), BlephEx (RySurg), intense pulsed light (IPL), and iLux (Alcon).
Drop-free treatment
I developed my Drop-Free Dry Eye Treatment (DDET) with the realization that patient compliance is a very real problem. My treatment relies on point-of-care testing and a procedure-based approach to OSD treatment. DDET embraces a paradigm shift centering on the use of cryo-preserved amniotic membrane (CAM; Prokera, BioTissue). This treatment addresses the compliance challenge and the subsequent reduced efficacy that comes with layering topical daily OSD treatments on top of glaucoma regimens.
Click here to watch a video related to this article
Related: How pain gates affect dry eye and chronic pain
DDET recognizes that it is essential to accurately assess the cause of OSD to provide the correct targeted treatment. InflammaDry indicates the presence of the inflammatory marker MMP-9; therefore, if the clinical examination agrees, we can avoid unnecessary anti-inflammatory topical medications. Punctal occlusion can be considered for those with non-inflammatory disease because it is effective for reducing symptoms of DED and reduces compliance concerns.14
Related: Scleral contact lenses help manage ocular surface disease
LipiScan meibography combined with meibomian gland expression and TBUT help when assessing OSD mechanisms. Meibomian gland dysfunction (MGD) has been reported to be present in 86 percent of patients with OSD.15 In my experience, identifying and treating MGD is an effective way to win patients and develop strong doctor–patient relationships. MGD treatment with LipiFlow, intense pulsed light (IPL), or iLux can yield a stabilized tear film, increased TBUT, enhanced comfort, and improved vision. A trained technician can perform these procedures while the doctor continues to see patients. Minimal at-home maintenance using a heat mask and lid hygiene extend the effects of treatment.
Related: Explore the relationship between dry eye and sleep
Amniotic membrane
I educate my OSD patients about the cause and effect of their dry eyes. MGD is often the cause, and the effect is frequently seen as superficial punctate keratitis. Their unhealthy corneal epithelium results in reduced visual acuity and discomfort. Many patients with chronic DED have severe keratitis but no discomfort due to their corneas becoming neurotrophic.16
Incorporating amniotic membrane treatment with CAM has changed the way I treat OSD. I had long used it to treat standard corneal injuries like burns and abrasions, with corneas healing in a matter of days. I opted to move CAM treatment from the end of the line for patients with severe DED up to a first-line treatment. My OSD patients are very receptive to treating their Dry Eye with CAM as an alternative to long-term daily drops.
Prokera also has anti-inflammatory properties17,18 and, as such, it has replaced the use of topical anti-inflammatory drops such as Restasis and Xiidra for most of my patients. The occasional placement of the membrane reduces inflammation as measured by InflammaDry and clinical observation.
Click here to watch a video related to this article
Related: Corneo-scleral topography allows for precise fitting
In practice, I have patients wear Prokera Clear for five days, then treat the contralateral eye for another five days. I use the monocular approach so patients can proceed with their normal routine. The patient’s vision is only moderately affected if the membrane aperture doesn’t line up with their line of sight. If keratitis is still present after removing the CAM at the end of five days, the patient and I decide whether to treat for another two to five days immediately or move to the second eye and return to the first eye later. I have found that many patients have a reduction in symptoms for five to seven months following treatment. When symptoms return, I typically treat with a shorter course of a two-day placement, again monocularly and treating the other eye successively. Patients are happy to get their ‘booster’ treatment and have their symptoms resolve, remembering the success of the previous treatment.
Related: New perspective and technologies affect glaucoma treatment
For patients with severe glaucoma who need multiple drops to be controlled or those resistant to a change in treatment that has worked for years, I have found Prokera can be a useful way to treat BAK-induced keratitis. Occasional CAM placement throughout the year can allow the effective glaucoma treatment to remain unchanged. I choose Prokera Clear for glaucoma patients in order to not occlude their vision and to have a clear opening for topical glaucoma medications to be administered. I have patients administer two drops at a time to ensure effective dosing while the CAM is in place.
Much like the move to making SLT a first-line treatment, by using CAM at the beginning of dry eye treatment we do our patients a tremendous service and build our practices with devoted patients who have healthier eyes.
Related: Offer IPL as a treatment for MGD and dry eye disease
Fewer drops, more success
As doctors, we have a great impact on our patients’ quality of life. We can tie them down with medications requiring frequent treatments, copays, and trips to the pharmacy or we can embrace advances and treat them accordingly. By getting out of our prescribing rut and writing prescriptions for BAK-free medications, we can reduce our patients’ chances of developing OSD. By performing SLT earlier, we can avoid or reduce self-administered medications and their associated compliance challenges. If we adopt a procedure-based approach to Dry Eye treatment, we can do much to reduce the compliance burden, improve our patients’ vision and comfort, and enhance their quality of life.
Click here to watch a video related to this article
Related: Novel drugs + delivery systems ease ocular pain and inflammation
References:
1. Pflugfelder SC, Baudouin C. Challenges in the clinical measurement of ocular surface disease in glaucoma patients. Clin Ophthalmol. 2011;5:1575–1583. doi: 10.2147/OPTH.S24410
2. Tsai JC. A comprehensive perspective on patient adherence to topical glaucoma therapy. Ophthalmology 2009;116:S30–S36.
3. Nordstrom BL, Friedman DS, Mozaffari E, Quigley HA, Walker AM. Persistence and adherence with topical glaucoma therapy. Am J Ophthalmol 2005;140:598–606.
4. Richardson C, Brunton L, Olleveant N, et al. A study to assess the feasibility of undertaking a randomized controlled trial of adherence with eye drops in glaucoma patients. Patient Prefer Adherence 2013;7:1025–1039.
5. Gooch N, Molokia SA, Condie R, et al. Ocular drug delivery for glaucoma management. Pharmaceutics 2012;4:197-211.
6. Mansberger SL, Sheppler CR, McClure TM, et al. Psychometrics of a new questionnaire to assess glaucoma adherence: The glaucoma treatment compliance assessment tool. Trans Am Ophthalmol Soc. 2013;111:1-16.
7. Budenz DL. A clinician’s guide to the assessment and management of nonadherence in glaucoma. Ophthalmology. 2009;116:S43–S47.
8. Sleath B, Blalock S, Covert D, et al. The relationship between glaucoma medication adherence, eye drop technique, and visual field defect severity. Ophthalmology. 2011;118:2398–2402.
9. Li X, Wang W, Zhang X. Meta-analysis of selective laser trabeculoplasty versus topical medication in the treatment of open-angle glaucoma. BMC Ophthalmol. 2015;15:107.
10. Wong MO, Lee JW, Choy BN, et al. Systematic review and meta-analysis on the efficacy of selective laser trabeculoplasty in open-angle glaucoma. Surv Ophthalmol. 2015;60:36–50.
11. The Glaucoma Laser Trial (GLT) and glaucoma laser trial follow-up study: 7. Results. Glaucoma Laser Trial Research Group. [No authors listed] Am J Ophthalmol. 1995;120718–731.
12. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5:75-92.
13. Nelson JD, Craig JP, Akpek EK et al. TFOS DEWS II Introduction. Ocul Surf. 2017;15:269-275.
14. Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017 Jul;15(3):575-628.
15. Lemp MA, Crews LA, Bron AJ, Foulks GN, Sullivan BD. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012; 31 (5): 472-478.
16. Goyal S, Hamrah P. Understanding Neuropathic Corneal Pain-Gaps and Current Therapeutic Approaches. Semin Ophthalmol 2016;31:59–70.
doi: 10.3109/08820538.2015.1114853
17. McDonald MB, Sheha H, Tighe S, et al. Treatment outcomes in the DRy Eye Amniotic Membrane (DREAM) study. Clin Ophthalmol 2018;12:677–681. doi: 10.2147/OPTH.S162203.
18. Tseng SCG. HC-HA/PTX3 purified from amniotic membrane as novel regenerative matrix: insight into relationship between inflammation and regeneration. Invest Ophthalmol Vis Sci 2016;57:ORSFh1–ORSFh8. doi: 10.1167/iovs.15-17637.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.




.png&w=3840&q=75)