The myopia epidemic: Are new therapies in sight?
Identifying the distinct pathways in myopic and hyperopic defocus signals could lead to new anti-myopia drugs.

Y. Shira Kresch, OD, MS, FAAO, is clinical instructor of optometric sciences in the Department of Ophthalmology at Columbia University Irving Medical Center.

Treatment and prevention of myopia are limited by a lack of understanding of its underlying mechanisms. However, a recent animal study has uncovered key signaling pathways that may be responsible for the retinal responses to defocus and are therefore potential therapeutic targets.
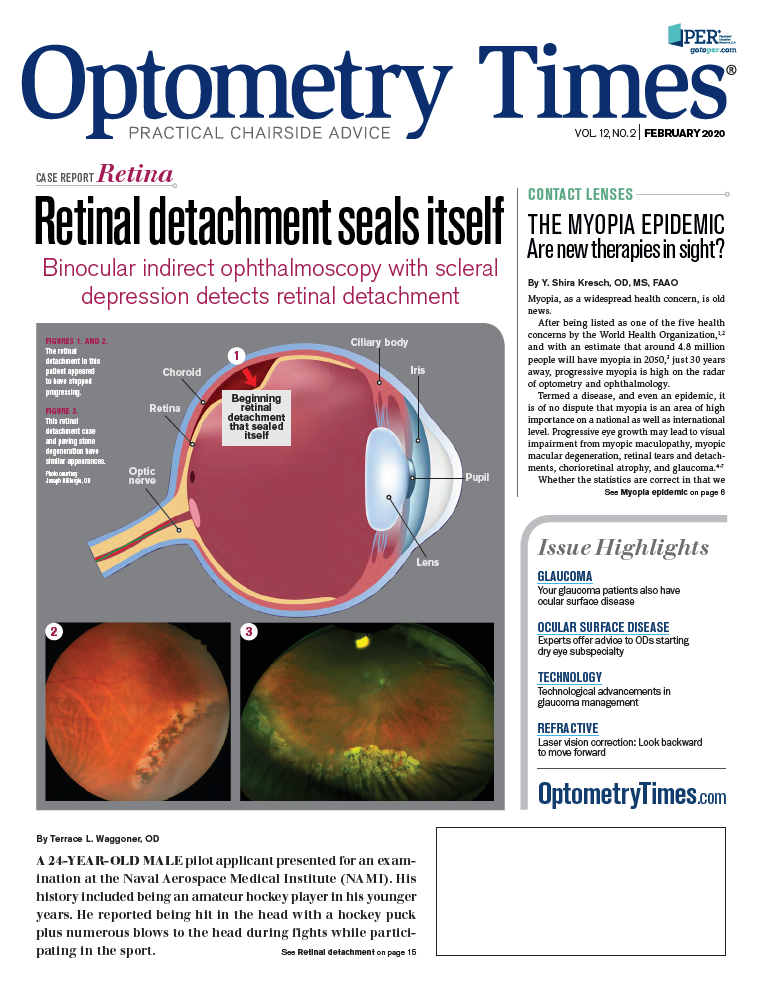
Myopia, as a widespread health concern, is old news.
After being listed as one of the five health concerns by the World Health Organization,1,2 and with an estimate that around 4.8 million people will have myopia in 2050,3 just 30 years away, progressive myopia is high on the radar of optometry and ophthalmology.
Termed a disease, and even an epidemic, it is of no dispute that myopia is an area of high importance on a national as well as international level. Progressive eye growth may lead to visual impairment from myopic maculopathy, myopic macular degeneration, retinal tears and detachments, chorioretinal atrophy, and glaucoma.4-7
Whether the statistics are correct in that we are facing a pending health crisis or not, myopia warrants careful attention to determine proper evidence-based approaches to management.
Related: Surgical, medical approaches making waves in presbyopia
Refractive and pharma options
There are two clinical approaches to retard progression of myopia: refractive and pharmaceutical.
Refractive modalities include:
• Multifocal soft contact lenses of center-distance design
• Orthokeratology
• Progressive or bifocal spectacles
Effectivity of these designs is hypothesized to be mostly secondary to inducing peripheral myopic-rather than hyperopic-defocus, in addition to decreasing accommodative lag.8
Related: How to build a myopia control practice
Refractive approaches to decrease axial growth progression have been attempted since the early 1900s and are discussed extensively across the literature. Briefly, emmetropization, the process whereby eye growth is matched to optical power, is largely driven by optical feedback.9-23 Hyperopic defocus (where light falls behind the retina) and myopic defocus (where light falls in front of the retina) have been shown to increase or decrease the rate of axial length growth, respectively. This has been studied in several animals, including primates, tree shrews, guinea pigs, mice, chickens, and fish.
Related: Unlock the potential of refractive surgery
The effect of optical defocus on emmetropization is theorized to be primarily a localized retinal phenomenon since experimental defocus caused changes in axial elongation even in eyes in which the optic nerve was severed,24-26 as well as in eyes subjected to segmental positive or negative defocus. It is assumed that this balance of positive and negative defocus ultimately leads to the final axial length of the eye.
Pharmaceutical
In the pharmaceutical category, certain anti-cholinergic agents, most notably atropine, have been shown to be effective at slowing the rate of axial elongation.
Atropine has gained increasing popularity recently because of the success it showed in the Atropine in the Treatment Of Myopia (ATOM) 1 and ATOM 2 studies, and it has even attained Level 1 evidence in slowing the growth of myopia, according to the American Academy of Ophthalmology.27 In spite of this, there are significant issues with its implementation.
See more: Minimize symptoms of dry eye disease in refractive surgery patients
Namely, we do not know the mechanism through which atropine slows axial growth. Does it have to do with the choroid? Dopamine? Accommodation? Increased sunlight exposure? This remains a mystery.
Additionally, there is limited evidence as to the most effective dosage in non-Asian children and no evidence on appropriate tapering schedules. This is complicated by the fact that there have not yet been biomarkers identified to aid in determination of which children of various ethnicities would do well with atropine as opposed to other modes of treatment.
Related: Patching, atropine may suit moderate or severe amblyopia
Finally, although atropine 0.01% is associated with minimal to no side effects, higher doses of atropine are responsible for uncomfortable visual phenomena, such as photophobia and blurred vision.28
However, even with such concerns, atropine works and is considered by most to be the most effective modality at retarding axial elongation, with the strongest evidential support.
Related: How to manage refractive surgery surprises
Potential gene therapy intervention
Given that the lack of additional pharmaceutical interventions is largely due to the uncertainties concerning the pathophysiology of optical development, the recently published work of Andrei Tkatchenko, MD, PhD, associate professor of ophthalmic sciences (in ophthalmology, and pathology and cell biology), is of particular significance.29
Several previous theories have been suggested regarding the development of myopia. The conventional assumption has been that there is a single genetic pathway that is responsible for a general “defocus.” This single pathway is supposed to be inclusive of both hyperopic and myopic defocus just with opposite triggering signals. One pathway would need to be signaled appropriately with positive defocus in order to retard growth.
Related: Macular diseases: Emerging best practices for diagnosis, management and follow-up protocols
Dr. Tkatchenko has suggested that this is not the case. Through his laboratory research on common marmosets, he showed that the primate retina is not only able to distinguish between hyperopic and myopic defocus but does so by activation or suppression of distinct signaling pathways in response to the different signs of defocus. This is novel and has been deemed bidirectional emmetropization by the sign of optical defocus (BESOD).
Additionally, Dr. Tkatchenko’s lab identified key signaling pathways that may be responsible for the retinal responses to either positive or negative defocus and can therefore be potential therapeutic targets. Furthermore, 29 genes that were differentially expressed upon imposed defocus in this animal model are also found in myopia-related loci in humans, raising the possibility of potential gene therapy intervention.29
While progressive myopia is of serious concern, with potential visual impairment in a significant number of the world’s population, the vigilance of the optometric community to address this concern head-on, and a readiness to implement evidence-based interventions as they become available, remains of high importance.
Related: Review clinical highlights of new myopia control lens
References:
1. Pararajasegaram R. VISION 2020-the right to sight: from strategies to action. Am J Ophthalmol. 1999;128(3):359-360.
2. Pizzarello L, Abiose A, Ffytche T, Duerksen R, Thulasiraj R, Taylor H, et al. VISION 2020: The Right to Sight: a global initiative to eliminate avoidable blindness. Arch Ophthalmol. 2004;122(4):615-620.
3. Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-1042.
4. Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31(6):622-660.
5. Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005;25(5):381-391.
6. Verhoeven VJ, Wong KT, Buitendijk GH, Hofman A, Vingerling JR, Klaver CC. Visual consequences of refractive errors in the general population. Ophthalmology 2015;122:101-109.
7. Flaxman SR, Bourne RRA, Resnikoff S, Ackland P, Braithwaite T, Cicinelli MV, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(12):e1221-e1234.
8. Cooper J, Tkatchenko A. A review of current concepts of the etiology and treatment of myopia. Eye Contact Lens. 2018; 44(4): 231-247.
9. Smith EL 3rd, Hung LF. The role of optical defocus in regulating refractive development in infant monkeys. Vision Res. 1999;39(8):1415-1435.
10. Hung LF, Crawford ML, Smith EL. Spectacle lenses alter eye growth and the refractive status of young monkeys. Nat Med. 1995;1(8):761-765.
11. Smith EL 3rd, Harwerth RS, Crawford ML. Spatial contrast sensitivity deficits in monkeys produced by optically induced anisometropia. Invest Ophthalmol Vis Sci. 1985;26(3):330-342.
12. Whatham AR, Judge SJ. Compensatory changes in eye growth and refraction induced by daily wear of soft contact lenses in young marmosets. Vision Res. 2001;41(3):267-273.
13. Graham B, Judge SJ. The effects of spectacle wear in infancy on eye growth and refractive error in the marmoset (Callithrix jacchus). Vision Res. 1999;39(2):189-206.
14. Cottriall CL, McBrien NA. The M1 muscarinic antagonist pirenzepine reduces myopia and eye enlargement in the tree shrew. Invest Ophthalmol Vis Sci. 1996;37(7):1368-1379.
15. Metlapally S, McBrien NA. The effect of positive lens defocus on ocular growth and emmetropization in the tree shrew. J Vis. 2008;8(3):1-12.
16. Norton TT, Siegwart JT Jr. Animal models of emmetropization: matching axial length to the focal plane. J Am Optom Assoc. 1995;66(7):405-414.
17. Howlett MH, McFadden SA. Spectacle lens compensation in the pigmented guinea pig. Vision Res. 2009;49(2):219-227.
18. Schaeffel F, Glasser A, Howland HC. Accommodation, refractive error and eye growth in chickens. Vision Res. 1988;28(5):639-657.
19. Irving EL, Sivak JG, Callender MG. Refractive plasticity of the developing chick eye. Ophthalmic Physiol Opt. 1992;12(4):448-456.
20. Irving EL, Callender MG, Sivak JG. Inducing myopia, hyperopia, and astigmatism in chicks. Optom Vis Sci. 1991;68(5):364-368.
21. Nevin ST, Schmid KL, Wildsoet CF. Sharp vision: a prerequisite for compensation to myopic defocus in the chick? Curr Eye Res. 1998;17(3):322-331.
22. Troilo D, Totonelly K, Harb E. Imposed anisometropia, accommodation, and regulation of refractive state. Optom Vis Sci. 2009;86(1):E31-E39.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.