ODs must examine more than just eyes

Today, comprehensive care in optometry requires observation of the entire patient.
Historically, the term “general survey” or “general appearance” is a fundamental component of the physical examination in medicine. In addition, doctors of optometry are familiar with the mandatory coding requirements of intermediate and comprehensive level ophthalmological examinations, which include the rather poorly defined component, “general medical observation.”1
Meaningful use requirements recently contributed to a general observation emphasis by adding height, weight, and body mass index to documentation.
Beyond technology
Technological advancements (ocular coherence tomography [OCT], ultra-widefield imaging), scope of practice enhancements (oral pharmaceuticals, injections, lasers), and telemedicine have produced interesting times for ODs.
It is not difficult to envision opportunities to provide better care via technology. The ability to detect patterns or correlations in data (machine learning) will revolutionize many professions and specialties, possibly succeeding in improved diagnoses, predictive capabilities, and treatments.2
Related: How OCT can help a smaller practice
However, we should consider the future of the physical components of comprehensive eye examinations, their emphases, and their possible de-emphases. It’s possible that decreasing the emphasis on complete physical examination will have associated negatives for patients.
The adage regarding nothing new existing under the sun applies here.
For example, cardiologist CK Phoon predicted a decreased role for physical examination for diagnosis over 17 years ago but reminded readers of the important positives of the physician-patient interaction, including:3
• Careful listening
• Touch as part of the healing process
• Berger’s “hierarchy of clinical observations” (diagnosis, personal characteristics of appearance and behavior, interactions/functioning of the family, insight into physician’s own feelings and behaviors)
• Physician status
• Control of the relationship
I contend that general appearance, the inclusion of such observations, and the maintenance of the doctor-patient relationship are crucial to the proper and optimal care of optometry patients.
In addition, physical characteristics such as gender, race, and build obviously provide information related to probable or improbable visual and systemic diagnoses.
Body weight and diabetes
While the tall, slender build associated with Marfan’s syndrome is relatively rare in general practice, the problems of obesity and its associated disorders are common in the United States. The astute clinician, for instance, might note the general distribution of adipose tissue of obesity from the truncal distribution of fat seen in Cushing and metabolic syndrome.
As entry points into the medical system, optometrists could have a powerful effect on patients’ health via simple observation relating to prediabetes.
Related: How diabetes affects your patients
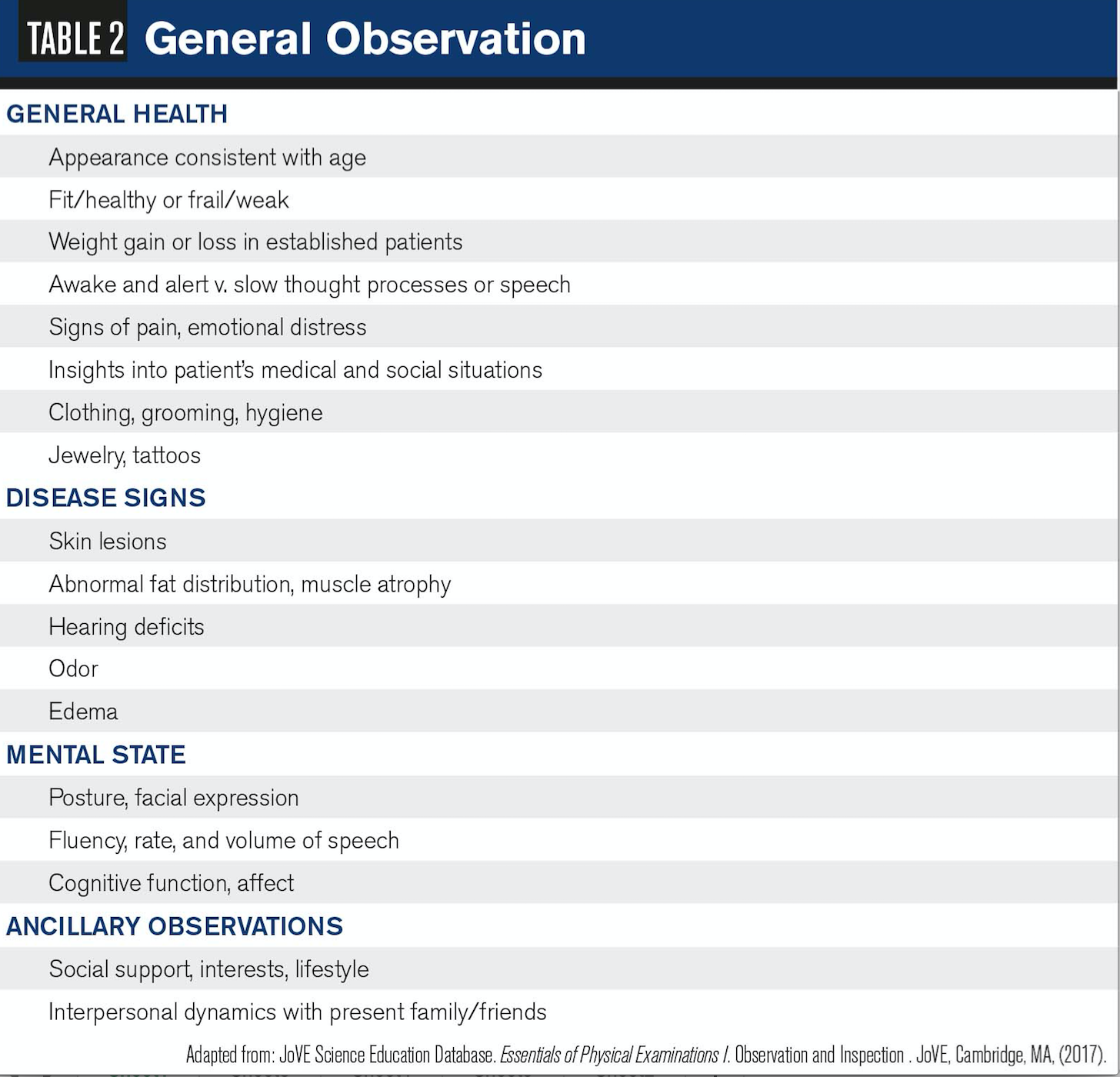
A recent survey of 140 primary-care providers (internal medicine, family medicine, internal medicine-pediatrics, nine nurse practitioners, and one physician assistant) found that only 6 percent correctly identified the 11 risk factors (Table 1) necessitating screening via the American Diabetes Association (ADA) guidelines. Plus, 30 percent of these providers were unfamiliar with the ADA guidelines.4
Obesity and a large neck circumference are associated with obstructive sleep apnea-a condition with numerous ocular associations such as floppy eyelid syndrome, glaucoma, papilledema, nonarteritic anterior ischemic optic neuropathy, and retinal vein occlusion.5,6
Furthermore, the OD might note obvious weight gain or weight loss in established patients, prompting concerns for endocrine disease, anorexia, or malignancy. Also, if a patient’s clothing does not correspond to the current temperature or weather, it may be an indication of poor circulation, thyroid disorders, or an altered mental state.7
Related: Ocular manifestations of diabetes: some clues for eyecare professionals
Physical movement
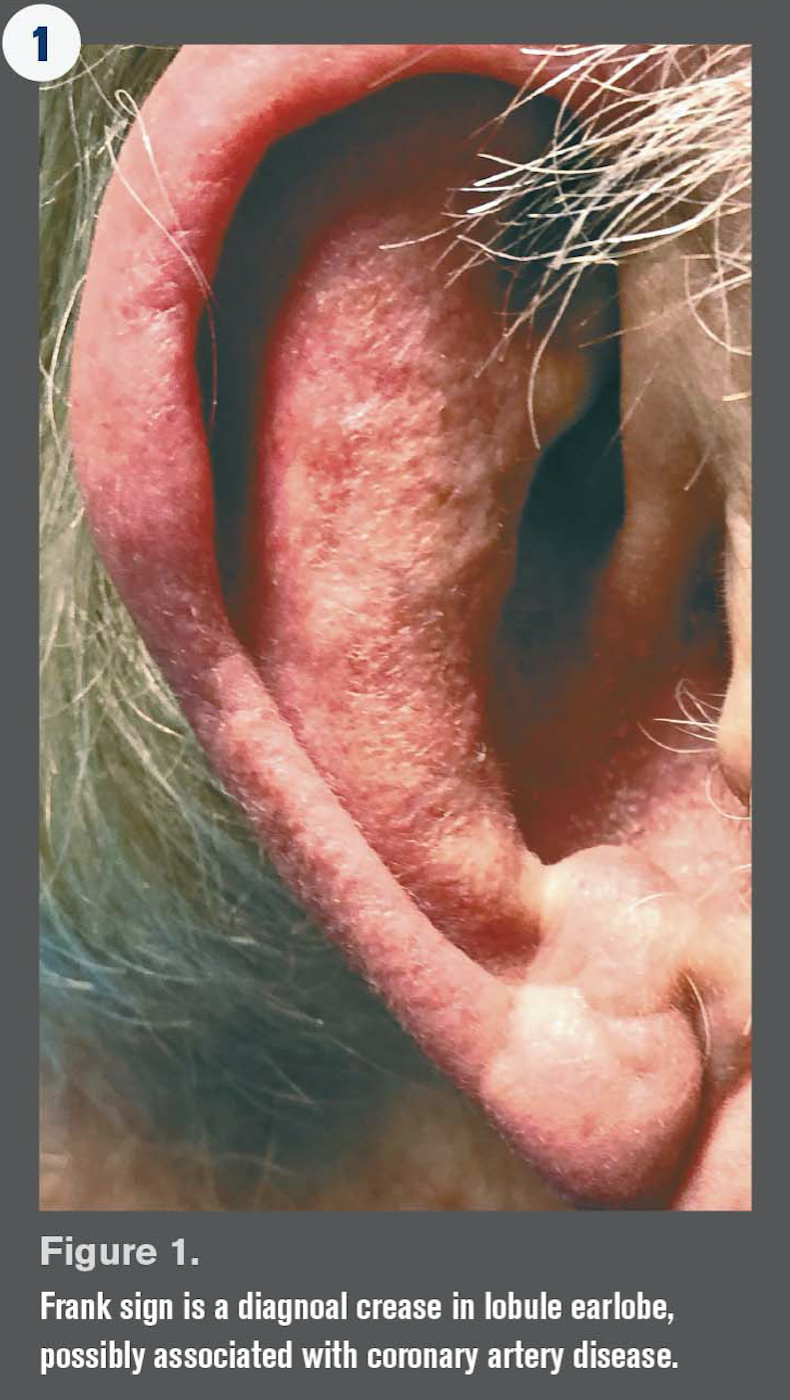
Another observation that the doctor should note would be the obvious deformities that relate to optimal care as well as assistive device usage such as canes and walkers. Common findings and their potential usefulness in geriatrics are summarized in Table 2.
Inspection of the patient rising from sitting and gait may provide evidence of orthostatic hypotension (OH), Parkinson's disease (PD), mobility problems, visual difficulty, risk of falling, and other disorders.
OH-decreased blood pressure from gravity with change of position-by itself may not be linked to falls; however, OH in patients with uncontrolled hypertension or systolic OH after one minute from standing are at increased risk.8,9
Previously by Michael W. Ohlson, OD, FAAO: 8 questions to ask before your next CE class
Autonomic nervous system dysfunction, including OH, may also be associated with Sjögren syndrome, and falling risk can be exacerbated by vision loss.10,11
Patients with PD may exhibit motor symptoms:12
• Bradykinesia (slowness of movements with progressive amplitude or speed loss upon rapid alternating movements)
• Hypomimia (decreased blinking and facial expression)
• Hypophonia (softer voice)
• Rest tremor (when the body part is at rest and supported, the “pill rolling variant)
• Rigidity (increased muscle tone with passive movement)
• Postural or gait impairment (stooped, slow, short shuffling steps with decreased arm swing)
Nonmotor signs and symptoms of PD may include:12
• Apathy
• Anxiety
• Depression
• OH, excessive sweating
• Seborrhea
• Sialorrhea (drooling)
• Sleep disorders
• Hyposmia (decreased sense of smell)
• Decreased visual contrast and color discrimination
• Decreased motion perception
• Cognitive/neurobehavioral abnormalities
• Pain
• Paresthesias
• Fatigue
These features may be noticeable years before the motor signs manifest, thus providing possible diagnostic value.12

Facial features
In addition to noting physical appearance, another fundamental observation doctors should note is the presence or absence of eyewear, strabismus, and so on. Even simple observations should include height and arm length as they relate to the likely working distances in the presbyopic population-an important visual concern-as well as observations of the head, faces, ears, and neck.
Remarks about the eyes and face are second nature in optometry, revealing dermatological (rosacea) and autoimmune (lupus) disease, cranial nerve dysfunction (ptosis, asymmetry), skin cancers, edema (kidney failure, Cushing syndrome), and temporal wasting (giant cell arteritis).
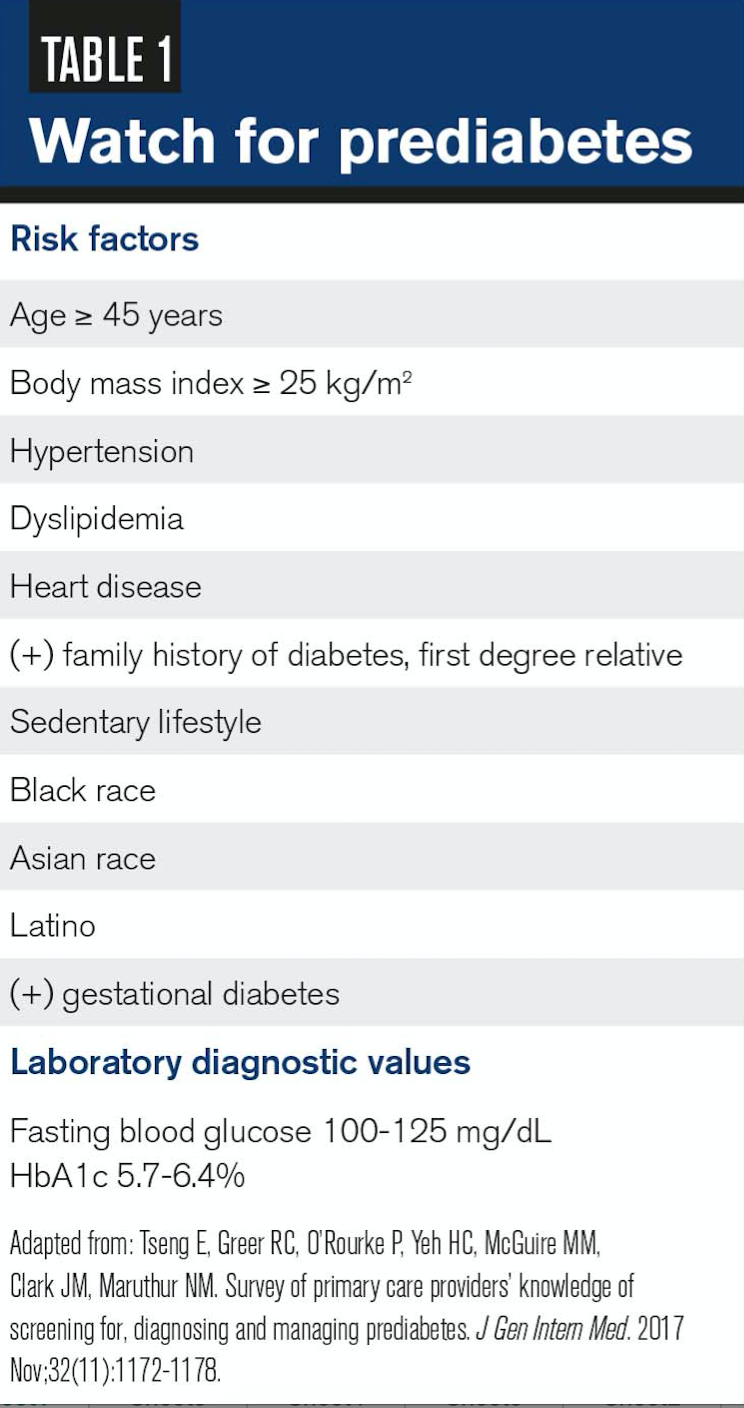
Simple inspection of the nose and external ear is recommended for both dermatological and eyewear concerns. Keep in mind that an earlobe crease (Frank’s sign) may be related to coronary artery disease (Figure 1).13
Additionally, facial expression may quickly demonstrate a mask-like appearance from Parkinsonism, depression, agitation, pain, or anxiety; and Acanthosis nigricans (AN) on the neck has been associated with diabetes. In a population of pediatric patients, AN was associated with poorer outcomes in the treatment of obesity.14
While often benign, AN has associations with:15
• Obesity
• Hypothyroidism
• Acromegaly
• Polycystic ovary disease
• Type 1 diabetes
• Cushing and Addison diseases
• Pinealoma
• Pituitary basophilism
• Ovarian hyperthecosis
• Stromal luteoma
• Ovarian dermoid cysts
• Prader-Willi syndrome
• Leprechaunism
• Lipoatrophic diabetes
• Pineal hyperplasia syndrome
• Alstrom syndrome
Furthermore, methamphetamine use can cause significant dental problems and breath odor may indicate poor hygiene, ketoacidosis (fruity), infection, tobacco, or ethanol.7,16
The patient’s voice may provide diagnostic clues for disease (hoarseness with hypothyroidism), mood, or relationships (both positive and negative) with those accompanying the patient to the examination.
Hands
Shaking hands can provide evidence of muscle weakness, frailty, joint tenderness, poor circulation, endocrine disease, or anxiety.
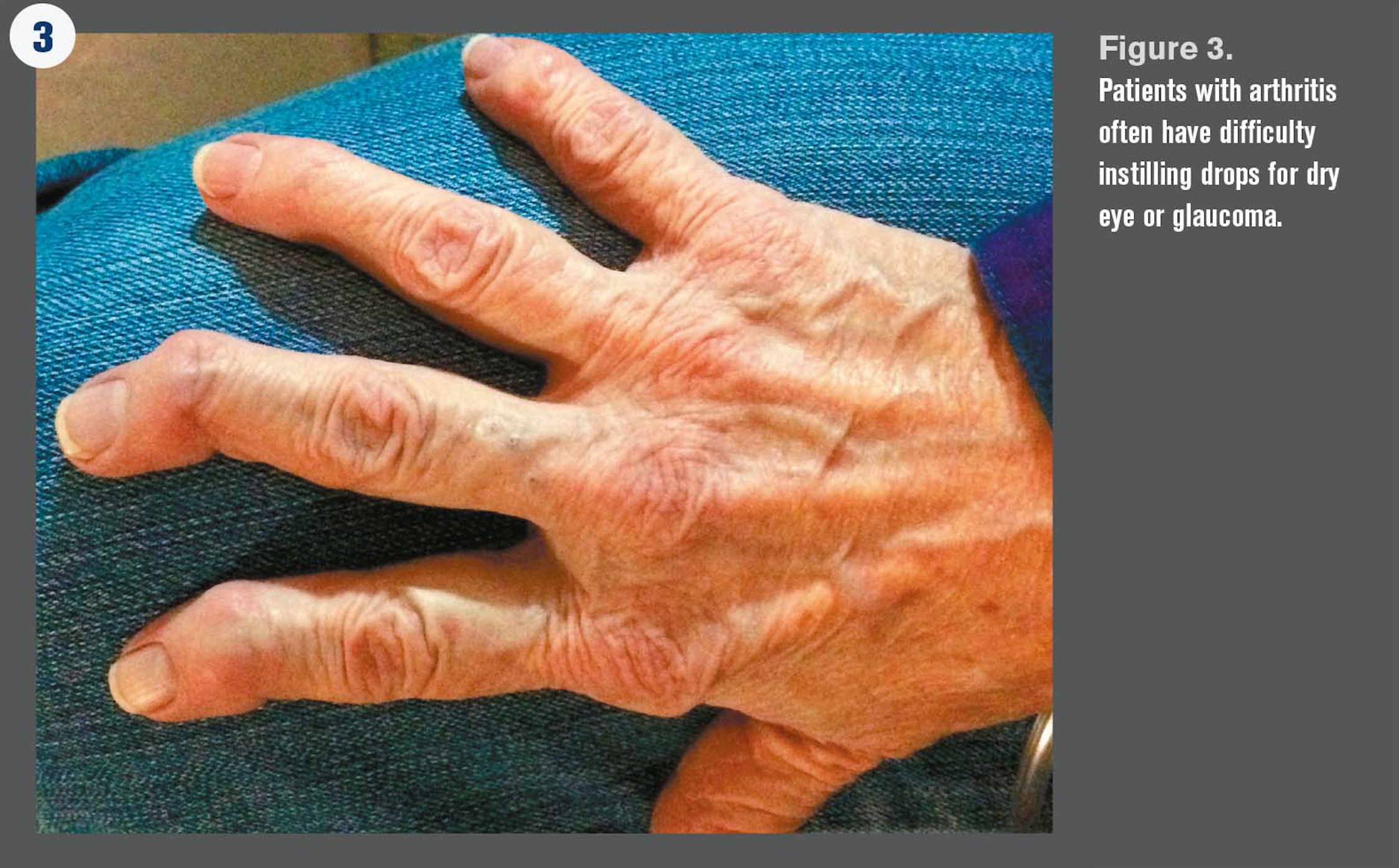
Some patients wear magnets or copper jewelry for presumed relief from osteoarthritis (OA) (Figures 2 and 3) or rheumatoid arthritis (RA) stiffness and pain; while not demonstrated as effective, observation may indicate a relevant problem.17,18
Ocular pseudoexfoliation syndrome, a systemic condition, may also be associated with OA of the knee as well as hypertension (HTN), coronary artery disease, cerebrovascular accident, sensoneurial hearing loss, and Alzheimer disease.19
Moreover, the impaired hand function (pain, inflammation, muscle weakness, deformities, and reduced grip force) caused by RA is a major cause of disability.20 In addition, noting the presence of hand deformities is clinically useful because onset occurs early in the disease process.21
Inspection of the hands may be crucial for the patient with dry eye or glaucoma because significant OA or RA may limit the ability to instill ophthalmic solutions, emulsions, suspensions, and gels.
A recent occupational therapy study found that 62 percent of RA patients had difficulty instilling eye drops; this population was 4.5 times more likely to have difficulty when compared to a population of ophthalmology clinic patients.22
Pediatric patients
Infants and children could have undiagnosed deformities, abnormal head size or shape, abnormal facies, poor nutritional status, and size or build inappropriate for age. Note that ODs are mandatory reporters of suspected abuse.
As with adult patients, the doctor may observe abnormal gait or tics.
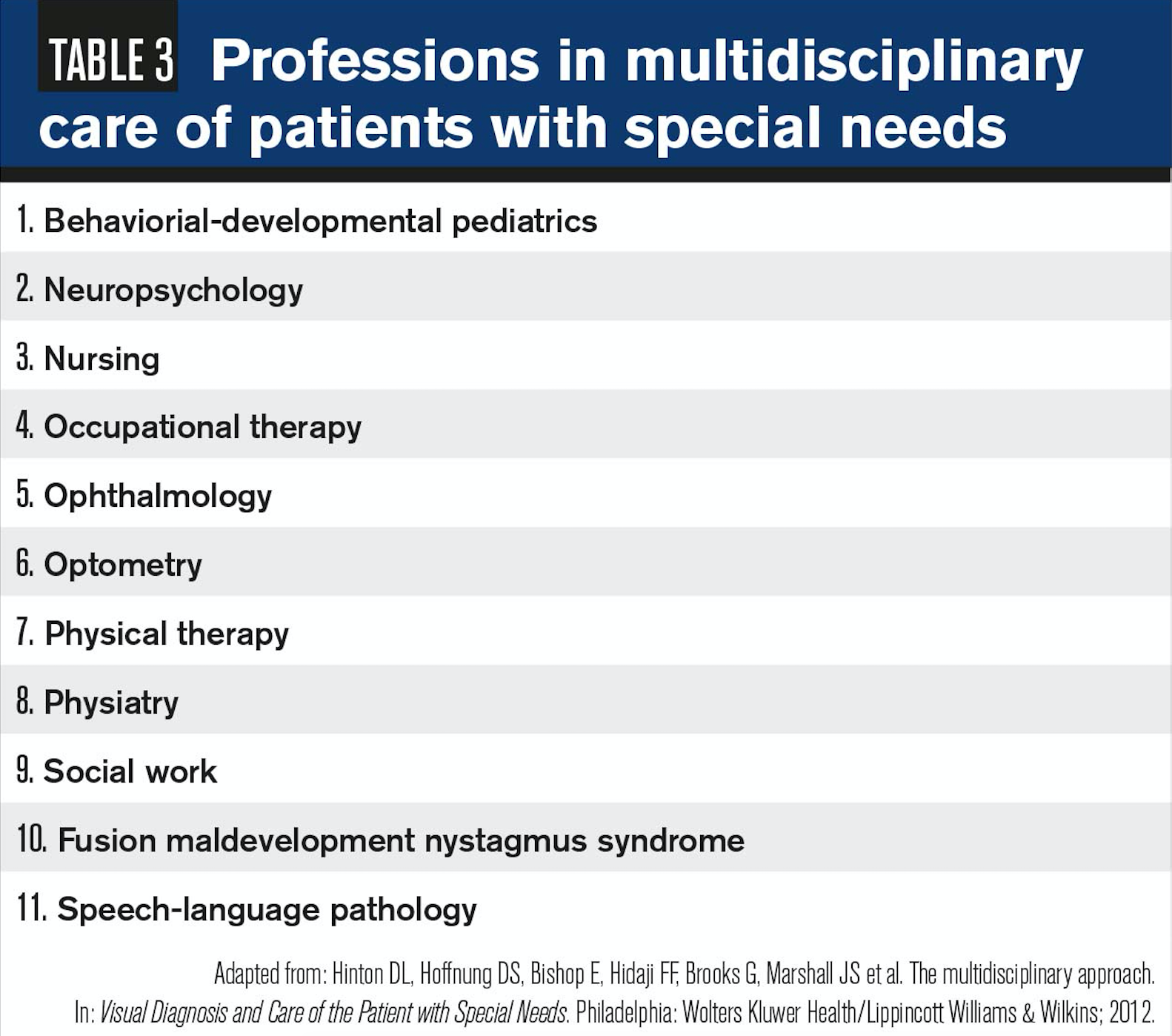
While beyond the scope of this article, it’s not unusual for ODs to examine pediatric special populations such as cerebral palsy, Down syndrome, autism, attention deficit hyperactivity disorder, and developmental delay as well as those of all ages with acquired brain injury, psychiatric illness, and neurodegenerative disease.23 General observation of these patients may be beneficial in the multidisciplinary/team approach (Table 3).
Gross observation
Observing a patient’s shoes can provide evidence of altered mental status or mood; ankle edema could indicate kidney or cardiovascular disease.
A shoe altered to allow an open toe could indicate gout.
Ocular manifestations of gout may include deposits of uric acid crystals in the conjunctiva, cornea, iris, and sclera; and hyperemia of the conjunctiva and episclera.24 Relevant comorbidities of gout include dry eye disease (DED), uveitis, cataract, glaucoma, metabolic syndrome, chronic kidney disease, and congestive heart failure.25
Related: Dry eye protocol for any practice
Shortness of breath or wheezing may be noted, heightening concerns for patients treated with beta blockers, which may indicate asthma, chronic obstructive pulmonary disease, cardiovascular disease, and obstructive sleep apnea. Ophthalmic timolol largely avoids the first-pass metabolism with about 80 percent of the medication systemically absorbed; this may result in symptomatic bradycardia, bronchospasm, heart conduction disorders, OH, syncope, and falls.26
Likewise, physical appearance and behavior provide clues to the mental status of the patient. Relevant aspects to optometrists may include grooming, emotional status, body language, mood, feelings, consciousness level, memory, attention span, voice quality (rate, volume, tone, coherence), and comprehension.
While the relationship remains unclear and prospective studies are needed, there is an association between DED symptoms and depression.27
A recent systematic review and meta-analysis found the overall prevalence of depression in eye disease patients to be 25 percent with the highest prevalence found in DED patients (29 percent).28 There is also a statistically significant association between DED and anxiety.29
Affect, the optometrist’s observation of the patient’s emotional state, is important, and mood, the patient’s subjective report or perception of his internal emotional state over the last weeks, may be clinically useful for management.
These conditions are not rare; Lee et al utilized a single question (“Do you often feel sad or depressed?”) to screen geriatric eye patients for depression with 20 percent noted as positive.30 Recommending referral, further evaluation, and treatment could provide life-altering benefits to the patient and her loved ones.
When creating treatment plans, ODs should also observe and consider:31
• Thought process (flow of thought)
• Thought content (obsessions, phobias)
• Insight (understanding and awareness of conditions)
• Judgment (the ability to identify consequences of actions)
Putting into practice
As we reflect upon the nature of modern optometry and our roles, the importance of general medical observation to proper care becomes clear. Many experienced practitioners utilize observation skills and senses honed over time perhaps without realizing the occurrence.
Related: How I am embracing the medical model in optometry
ODs cite themselves as primary-care providers and for good reason:32
• We evaluate and manage acute problems
• We provide and collaborate in the ongoing care of patients with one or more chronic conditions
• We offer early detection and education (consider HTN, diabetes, and falls)
• We coordinate referrals
Several of the “Cs” of primary care mesh well with optometry and general medical observation. These include:33
• Continuity (seeing patients over time, longitudinal)
• Comprehensiveness (substantial comorbidities, chronic conditions)
• Coordination (arranging referrals), contact-first (may represent entry into medical system)
• Communication (communicating effectively with patients),
• Collaboration (working well with teams or other healthcare providers, partnering with patients)
• Compliance (monitoring and enhancing compliance to care)
Sir William Osler, a Canadian physician and one of the four founding professors of Johns Hopkins Hospital, once said: “Learn to see, learn to hear, learn to feel, learn to smell, and know that by practice alone can you become expert.”34
Osler would have made a fine optometrist.
Read more by Michael W. Ohslon, OD, FAAO
References:
1. Asbell RL. Perils of the eye codes. Retina Today. 2017 Mar;28-31.
2. Rourke S. 5 FAQ about machine learning. Medscape. July 31, 2017. Available at: http://www.medscape.com/viewarticle/883382 Accessed August 13, 2017.
3. Phoon CK. Must doctors still examine patients? Perspect Biol Med. 2000 Summer;43:548-561.
4. Tseng E, Greer RC, O’Rourke P, Yeh HC, McGuire MM, Clark JM, Maruthur NM. Survey of primary care providers’ knowledge of screening for, diagnosing and managing prediabetes. J Gen Intern Med. 2017 Nov; 32(11):1172-1178.
5. Semelka M, Wilson J, Floyd R. Diagnosis and treatment of obstructive sleep apnea in adults. Am Fam Physician. 2016 Sep 1;94(5):355-360.
6. Lettieri CJ. The 5 most common ocular manifestations of obstructive sleep apnea. Medscape. October 2, 2013. Available at: http://www.medscape.com/viewarticle/811875 Accessed August 13, 2017.
7. Berk SL, Verghese A. General appearance. In: Walker HK, Hall WD, eds. Clinical Methods, 3rd edition. Boston: Butterworths; 1990:987-989.
8. Gangavati A1, Hajjar I, Quach L, Jones RN, Kiely DK, Gagnon P, Lipsitz LA. Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. J Am Geriatr Soc. 2011 Mar;59(3):383-389.
9. Ong HL, Abdin E, Seow E, Pang S, Sagayadevan V, Chang S, Vaingankar JA, Chong SA, Subramaniam M. Prevalence and associative factors of orthostatic hypotension in older adults: Results from the Well-being of the Singapore Elderly (WiSE) study. Arch Geron Geriatr. 2017 Sep;72:146-152.
10. Goodman BP, Crepeau A, Dhawan PS, Khoury JA, Harris LA. Spectrum of autonomic nervous system impairment in Sjögren syndrome. Neurologist. 2017 Jul;22(4):127-130.
11. Lee AG, Friedman DS. Vision loss and falls. In: Lee AG, Beaver HA, eds. Geriatric Ophthalmology: A Competency-based Approach. New York: Springer; 2009:83-87.
12. Massano J, Bhatia KP. Clinical approach to Parkinson’s disease: features, diagnosis, and principles of management. Cold Spring Harb Perspect Med. 2012 Jun;2 (6).
13. Agouridis AP, Elisaf MS, Nair DR, Mikhailidis DP. Ear lobe crease: a marker of coronary artery disease? Arch Med Sci. 2015 Dec 10;11(6):1145-1155.
14. Dalle Valle M, Laatikainen T, Lehikoinen M, Nykänen P7, Jääskeläinen J. Paediatric obesity treatment had better outcomes when children were younger, well motivated and did not have acanthosis nigricans. Acta Paediatrica. 2017 Nov;106(11):1842-1850.
15. Somaiah S, Bhimji S. Acanthosis nigricans. StatPearls. Available at: https://www.ncbi.nlm.nih.gov/books/NBK431057/. Accessed 11/15/18.
16. Winslow BT, Voorhees KI, Pehl KA. Methamphetamine abuse. Am Fam Physician. 2007 Oct 15;76(8):1169-74.
17. Richmond SJ, Brown SR, Campion PD, Porter AJ, Moffett JA, Jackson DA, Featherstone VA, Taylor AJ. Therapeutic effects of magnetic and copper bracelets in osteoarthritis: a randomised placebo-controlled crossover trial. Complement Ther Med. 2009 Oct-Dec;17(5-6):249-56.
18. Richmond SJ, Gunadasa S, Bland M, MacPherson H. Copper bracelets and magnetic wrist straps for rheumatoid arthritis – analgesic and anti-inflammatory effects: a randomised double-blind placebo controlled crossover trial. PLoS ONE. 2013 Sep 16;8(9): e71529.
19. Ucar M, Sarp U, Kirboga K, Adam M, Arik HO, Gundogdu F. Is there an association between pseudoexfoliation syndrome and knee osteoarthritis? Z Rheumatol. 2015 Nov;74(9):819-23.
20. Rydholm M, Book C, Wikström C, Turesson C. Despite early improvement, patients with rheumatoid arthritis still have impaired grip force 5 years after diagnosis. Ann Rheum Dis. 2015;74:430.
21. Johnsson PM, Eberhardt K. Hand deformities are important signs of disease severity in patients with early rheumatoid arthritis. Rheumatology. 2009 Nov;48(11):1398-1401.
22. Adamson E, Kendall G. Difficulty in eye drop administration for people with rheumatoid arthritis. Br J Occup Ther. 2016 Sept;79(9):519-520.
23. Taub MB, Bartuccio M, Maino DM. Visual Diagnosis and Care of the Patient with Special Needs. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2012.
24. Lin J, Zhao GQ, Che CY, Yang SS, Wang Q, Li CG. Characteristics of ocular abnormalities in gout patients. Int J Ophthalmol. 2013 Jun 18;6(3):307-11.
25. Sharon Y, Schlesinger N. Beyond joints: a review of ocular abnormalities in gout and hyperuricemia. Curr Rheumatol Rep. 2016 Jun;18(6):37.
26. Mäenpää J, Pelkonen O. Cardiac safety of ophthalmic timolol. Expert Opin Drug Saf. 2016 Nov;15(11):1549-1561.
27. Hallak JA, Tibrewal S, Jain S. Depressive symptoms in dry eye disease patients: a case-control study using the Beck Depression Inventory. Cornea. 2015 Dec;34(12):1545-1550.
28. Zheng Y, Wu X, Lin X, Lin H. The prevalence of depression and depressive symptoms among eye disease patients: a systematic review and meta-analysis. Sci Rep. 2017 Apr 12;7:46453
29. van der Vaart R, Weaver MA, Lefebvre C, Davis RM. The association between dry eye disease and depression and anxiety in a large population-based study. Am J Ophthalmol. 2015 Mar;159(3):470-4.
30. Lee AG. Vision loss and depression. In: Lee AG, Beaver HA, eds. Geriatric Ophthalmology: A Competency-based Approach. New York: Springer; 2009:65-70.
31. Snyderman D, Rovner BW. Mental status examination in primary care: a review. Am Fam Physician. 2009 Oct 15;80(8):809-814.
32. Bowker NK. Public health aspects of older adult patient care. In: Rosenbloom AA, ed. Vision and Aging. St. Louis: Butterworth Heinemann; 2007:365-380.
33. Kroenke K. The many C’s of Primary Care. J Gen Intern Med. 2004 Jun;19(6):708-709.
34. Bryan CS. Osler: Inspirations rom a Great Physician. New York: Oxford University Press; 1997.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.