A practical guide to the best of the current multifocal IOLs
Managing patient expectations is key to selecting the best lens
The field of presbyopia correction already includes many excellent IOLs that can offer a significant range of spectacle-free vision for a motivated patient, yet the field continues to evolve rapidly in search of lenses that offer better accommodation with less adverse effects. For a truly successful outcome, your patient must clearly understand their priorities, and you and your surgery center must understand the options. (Adobe Stock / Oktay)
The field of presbyopia-correcting IOLs has been evolving rapidly. Several new IOLs have entered the market in the past few years, and more are expected to become available in the future. Helping our patients navigate the decisions regarding these lenses often improves their satisfaction after cataract surgery. Patients look to us for advice on whether to consider a presbyopia-correcting IOL, what attributes to prioritize in their choice of lens, and whether their postoperative visual experiences are typical. Despite immense amounts of online information, this information is often hard to discover, obscured by marketing, and difficult to verify.
Our surgery center has kept up with the current explosion in multifocal IOLs, and we have learned many lessons by observation and by the assistance of patients who kindly share their experiences with us. This article will explain the advantages and disadvantages of the best of the current presbyopia-correcting IOLs, how the changing technology affects appropriate patient selection and counselling, and what to expect if your patient receives these lenses.
There is no free lunch in optics
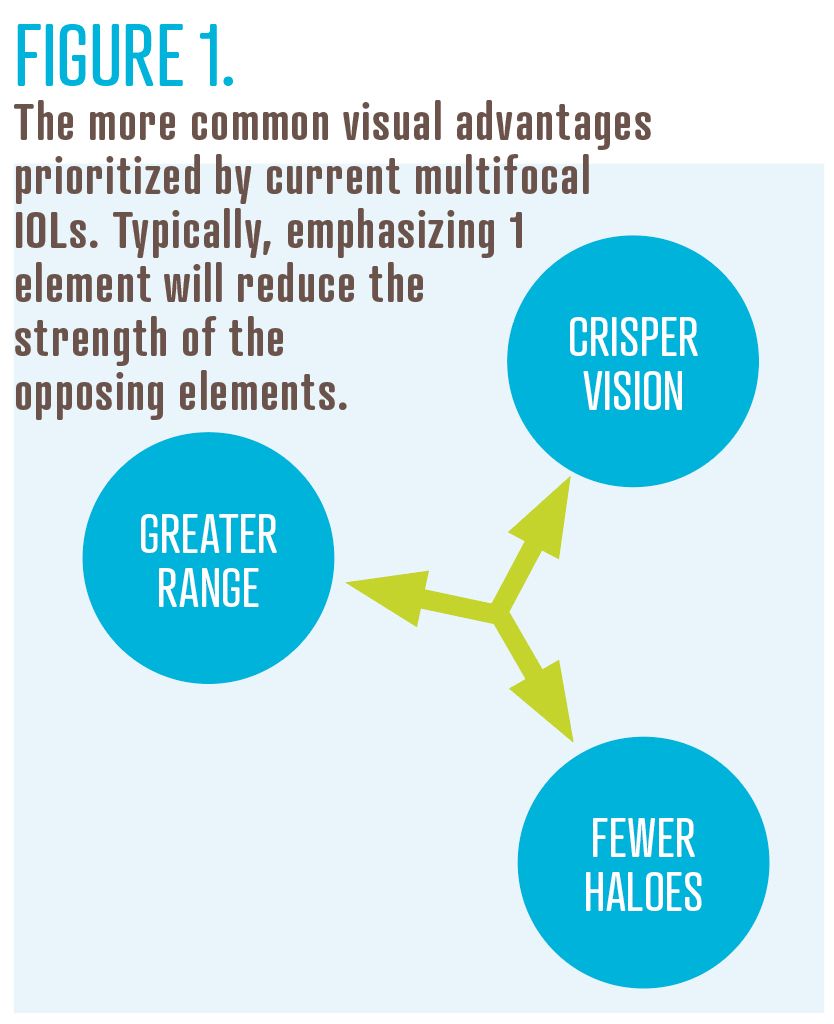
The laws of physics prohibit the creation of an ideal multifocal IOL; it is impossible to create a lens that can provide a perfect image at varying distances, with no aberrations and no loss of light. Therefore, the key to successful multifocal IOL selection is an intimate knowledge of the compromises inherent in each option. In addition, the more your patient can clearly state which strengths are the most desirable to them personally and which compromises are acceptable, the better their satisfaction will be with the final decision.1 Some of the more common strengths of the current multifocal IOLs are shown in Figure 1, where prioritizing 1 wing of the triad will generally result in a compromise in the other 2 wings.
Multifocal IOLs are not a good option for everyone, whether due to patient temperament, the additional cost, the vagaries of neuroadaptation, the effect on daytime and nighttime vision, or simply an affection for glasses. Certain patients will never be pleased with multifocal IOLs and should not be pressured.2
However, improved optical properties in newer multifocal IOLs mean that more and more patients can be considered for these lenses. Long regarded with suspicion due to significant optical aberrations, the newest crop of multifocal IOLs have finally achieved a remarkable level of performance and are a good choice for many patients.
There have also been recent advancements in monofocal IOL technology, with several next-generation monofocal IOLs entering the market, including the Tecnis Eyhance (Johnson & Johnson Vision) and the RayOne EMV (Rayner). Although one of the noticeable improvements over conventional monofocal IOLs has been a small increase in the depth of focus, those IOLs are still not powerful enough to be considered extended-depth-of-focus (EDOF) IOLs and thus are not reviewed in this article.
The PanOptix IOL
The PanOptix IOL (Alcon) is still the only trifocal IOL available in the United States, and many surgeons have adopted it enthusiastically as an improvement over older bifocal IOLs. One of this IOL’s most attractive features is the usefulness of its 3 focal points—emmetropia, 24 in (+1.67 D), and 16 in (+2.50 D)—corresponding comfortably to many common activities. The PanOptix IOL is available in spherical powers and with toric correction of between approximately 1.00 and 2.60 D. It achieves its effect with a sophisticated series of diffractive steps molded onto its anterior surface.3
Diffractive optics reduce contrast sensitivity, the ability to discern objects with similar color and brightness, especially in low lighting. Because corneal or macular disease will also reduce contrast sensitivity, all diffractive IOLs are contraindicated in eyes with these diseases to avoid any additive effect.4 Even with its superior chromatic aberration control, the PanOptix IOL is still contraindicated in eyes with significant ocular surface disease, basement membrane dystrophy, epiretinal membranes, and diabetic retinopathy.
Like all diffractive lenses, the PanOptix IOL produces glare, haloes, and starbursts, collectively known as dysphotopsias. The PanOptix technically has 4 focal points, 2 of which overlap to strengthen distance acuity. This strategy also works to reduce dysphotopsias to some extent.5
The PanOptix IOL tends to provide good distance, intermediate, and near vision, with nighttime aberrations that are acceptable to most patients. For a patient who desires good vision across a wide range of distances, the PanOptix IOL is a great choice.
The Synergy IOL
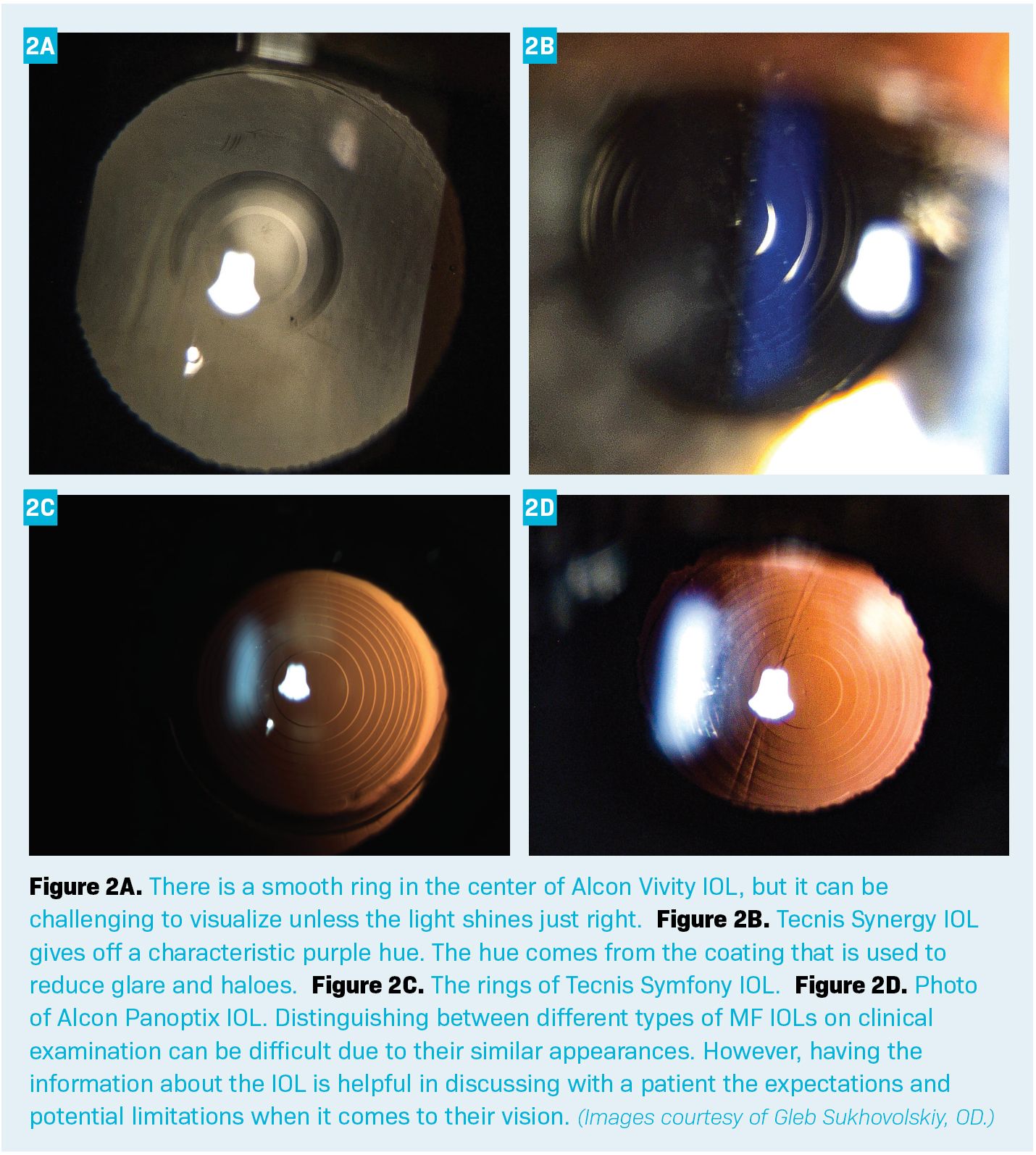
Like the PanOptix, the Tecnis Synergy IOL (Johnson & Johnson Vision) is a diffractive multifocal, though with a slightly different mechanism. The Synergy IOL has 1 focal point at plano and a broad range of near vision, from approximately 26 in (1.50 D) to 13 in (3.00 D). The Synergy IOL is available in spherical powers and as a toric version with astigmatism correction from 1.00 to 2.60 D.6 The design of the Synergy IOL borrows several successful elements from the TECNIS Symfony IOL, including an EDOF design (here used to cover the near range), minimization of chromatic aberration, and reduction of spherical aberration. The Synergy IOL has a syncopated concentric sawtooth pattern lathed onto its posterior surface, as well as a frosted edge to reduce dysphotopsias.7 Patients often notice slightly better very near vision with the Synergy IOL compared with the PanOptix IOL.8
The more aggressive range should produce greater glare and haloes, but the Synergy uses a violet light filter on the posterior surface that blocks wavelengths from 360 to 460 nm, reducing these aberrations. On average, patients rate the glare and haloes as similar to those of the PanOptix IOL. The Synergy IOL is contraindicated for any case of corneal or macular disease due to the compounding effect of contrast sensitivity degradation.
The Synergy IOL is a great choice for patients who want good distance, intermediate, and near vision, and particularly those who have enjoyed and want to preserve very near vision and who do not mind some nighttime aberrations.
The EDOF IOLs
EDOF IOLs trade less satisfying near visual acuity in exchange for crisper distance vision and fewer aberrations. They tend to be a good choice for patients who are concerned about the risk of nighttime glare and haloes, those who are prevented from getting a diffractive multifocal IOL because of mild corneal or macular disease, and those who do not prioritize very near vision.
EDOF IOLs are defined by the FDA as lenses that provide Snellen visual acuity to within 1 letter of that provided by a monofocal IOL, and a depth of field that is at least 0.50 D greater than a monofocal.9 Depending on pupil size, most monofocals already provide 0.75 D to 1.00 D of depth of field, so an additional 0.50 D of depth of field increases that from 1.25 D to 1.50 D. This brings objects that are only 24 to 30 in away into focus, encompassing vehicle dashboards, computer monitors, and tablets.
EDOFs are well suited for patients who want some depth of field to increase their glasses independence but do not mind resorting to reading glasses for close work or work in dim light. They tend to perform very well for active individuals who spend a lot of time outdoors and want some near function but will not tolerate compromises to their distance vision.
Although Bausch + Lomb’s Crystalens (2003) and Johnson & Johnson’s Tecnis +2.75 (2015) both arguably fit into the EDOF category, neither is used much anymore; the pseudo-accommodative movement of the Crystalens rarely worked as hoped, and the older optics of the Tecnis have fallen out of favor.10 Therefore, we will primarily cover 2 newer EDOF IOLS: the Vivity and the Symfony.
The Vivity IOL
In contrast to the diffractive multifocal IOLs, the Vivity IOL (Alcon) is a nondiffractive (or refractive) lens, using sophisticated optical elements on its anterior and posterior surfaces to elongate the range of focus significantly. The Vivity functions as an EDOF IOL, with continuous vision from infinity to approximately 26 in (+1.50 D).11 The Vivity is available as a spherical and a toric version, with toric powers compensating for 1.00 to 2.45 D of corneal cylinder.12
Despite its weaker performance at near when compared with other MFIOLs, patients have been enthusiastic about the Vivity; one big reason for this is the near absence of glare and haloes. A great benefit of its nondiffractive design is having similar nighttime aberrations to those of a monofocal IOL. Patients commonly describe their vision through this lens as “natural.”13
Because of the minimal aberrations, the Vivity IOL can sometimes be implanted in patients with mild corneal or macular disease, as long as they receive appropriate counselling. Thus, the Vivity has expanded our pool of potential candidates for presbyopia-correcting IOLs. According to one study, although the Vivity IOL can be implanted in eyes with mild epiretinal membranes, the macular pathology may negate much of the EDOF effect, effectively leaving the patient with an expensive monofocal.14
The Vivity provides good distance and intermediate vision, but like other EDOFs, it does not typically allow for good uncorrected near vision. If acceptable to the patient, a minimonovision strategy can bolster near vision considerably. The Vivity IOL is a great lens for patients who want good distance and intermediate vision, do not mind wearing reading glasses for some near tasks, and would dislike any glare or haloes.
The Symfony IOL
The TECNIS Symfony EDOF IOL (Johnson & Johnson) uses diffraction to split light between 2 close foci, resulting in a bifocal IOL with focal peaks at plano and at +1.75 D (22 in). These peaks merge such that in most lighting conditions, patients experience a continuous range of good vision all the way from infinity to intermediate distance. In dim lighting, a perceptive patient may notice 2 separate peaks.15 The Symfony IOL comes in a spherical and a toric version; the toric model can correct for corneal astigmatism of between 1.0 to 2.6 D.16
The Symfony is a diffractive lens with a concentric sawtooth surface pattern on the anterior surface.17 This IOL may produce glare, haloes, and starbursts similar to those of the Synergy.
One of the more ingenious strategies employed by the Symfony is a reduction in chromatic aberration that is achieved by manipulation of the diffractive design. This results in superior contrast sensitivity compared with most other presbyopia-correcting IOLs.18 This same design strategy has been employed in the Synergy IOL. Even with its superior chromatic aberration control, the Symfony is still contraindicated in the presence of any corneal or macular disease.
The Symfony tends to provide good distance and intermediate vision but does not perform well at near vision. Some patients are amenable to a strategy of minimonovision, whereby the nondominant eye is targeted at –0.50 D; this slight adjustment can give more functional uncorrected near vision.19 With the success of the Synergy, which employs similar optics but achieves a more powerful range, many surgical centers have seen the use of the Symfony IOL decrease. In general, the Symfony is a good IOL for patients who desire good distance and intermediate vision and do not mind some compromise to their near vision and some nighttime aberrations.
In the pipeline
A new type of EDOF IOL has been recently FDA approved in the United States—the IC 8 small-aperture IOL (AcuFocus, Inc)—although it is yet to be released for widespread use. The design involves creating a pinhole effect with a 3.23-mm central black circular mask with a 1.36-mm central aperture. 20The mask has more than 3200 microperforations to limit any negative effect on patient’s field of vision. The pinhole effect provided by this IOL may allow for good distance, intermediate vision, and potentially functional near vision. We have yet to try this IOL in practice.
Many companies are looking far past the current options of diffractive or refractive multifocal IOLs, toward what is often referred to as the “Holy Grail” of IOLs: a truly accommodating IOL. Such an IOL could change its refractive power, driven by contraction of the ciliary body—just as in a prepresbyopic human eye. Presently, the leaders are the FluidVision (Alcon), the modular Juvene (LensGen, Inc), and the JelliSee (JelliSee Ophthalmics, Inc); the first 2 of these are already undergoing human trials.21 The JelliSee claims to deliver an astonishing 6 D of true accommodation.22
In addition to the careful consideration of your patient’s priorities and of the characteristics of each IOL, priority should be given to the preferences of your cataract surgeon. Many surgeons find that some multifocal IOLs work well in their hands, whereas others do not—this should be respected.
The field of presbyopia correction already includes many excellent IOLs that can offer a significant range of spectacle-free vision for a motivated patient, yet the field continues to evolve rapidly in search of lenses that offer better accommodation with less adverse effects. For a truly successful outcome, your patient must clearly understand their priorities, and you and your surgery center must understand the options.
References
Alió JL, Pikkel J, eds. Multifocal Intraocular Lenses: The Art and the Practice. Springer Cham; 2014.
Braga-Mele R, Chang D, Dewey S, et al. Multifocal intraocular lenses: relative indications and contraindications for implantation. J Cataract Refract Surg. 2014;40(2):313-322. doi:10.1016/j.jcrs.2013.12.011
Kohnen T, Marchini G, Alfonso JF, et al. Innovative trifocal (quadrifocal) presbyopia-correcting IOLs: 1-year outcomes from an international multicenter study. J Cataract Refract Surg. 2020;46(8):1142-1148. doi:10.1097/j.jcrs.0000000000000232
Alió JL, Pikkel J. Multifocal intraocular lenses: preoperative considerations. In: Alió JL, Pikkel J, eds. Multifocal Intraocular Lenses: The Art and the Practice. Springer Cham; 2014:29-38.
Kohnen T, Herzog M, Hemkeppler E, et al. Visual performance of a quadrifocal (trifocal) intraocular lens following removal of the crystalline lens. Am J Ophthalmol. 2017;184:52-62. doi:10.1016/j.ajo.2017.09.016
Ribeiro F,J Ferreira TB, Silva D, Matos AC, Gaspar S. Visual outcomes and patient satisfaction after implantation of a presbyopia-correcting intraocular lens that combines extended depth-of-focus and multifocal profiles. J Cataract Refract Surg. 2021;47(11):1448-1453. doi:10.1097/j.jcrs.0000000000000659
Gabrić N, Gabrić I, Gabrić K, Biščević A, Piñero DP, Bohač M. Clinical outcomes with a new continuous range of vision presbyopia-correcting intraocular lens. J Refract Surg. 2021;37(4):256-262. doi:10.3928/1081597X-20210209-01
Ferreira TB, Ribiero FJ, Silva D, Matos AC, Gaspar S, Almeida S. Comparison of refractive and visual outcomes of 3 presbyopia-correcting intraocular lenses. J Cataract Refract Surg. 2022;48(3):280-287. doi:10.1097/j.jcrs.0000000000000743
Kohnen T, Suryakumar R. Extended depth-of-focus technology in intraocular lenses. J Cataract Refract Surg. 2020;46(2):298-304. doi:10.1097/j.jcrs.0000000000000109
de Vries NE, Webers CA, Touwslager WR, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37(5):859-865. doi:10.1016/j.jcrs.2010.11.032
Kohnen T. Nondiffractive wavefront-shaping extended range-of-vision intraocular lens. J Cataract Refract Surg. 2020;46(9):1312-1313. doi:10.1097/j.jcrs.0000000000000247
Ibid.
Arrigo A, Gambaro G, Fasce F, Aragona E, Figini I, Bandello F. Extended depth-of-focus (EDOF) AcrySof IQ Vivity intraocular lens implant: a real-life experience. Graefes Arch Clin Exp Ophthalmol. 2021;259(9):2717-2722. doi:10.1007/s00417-021-05245-6
Jeon S, Choi A, Kwon H. Clinical outcomes after implantation of extended depth-of-focus AcrySof Vivity intraocular lens in eyes with low-grade epiretinal membrane. Graefes Arch Clin Exp Ophthalmol. 2022;260(12):3883-3888. doi:10.1007/s00417-022-05751-1
Loicq J, Willet N, Gatinel D. Topography and longitudinal chromatic aberration characterizations of refractive-diffractive multifocal intraocular lenses. J Cataract Refract Surg. 2019;45(11):1650-1659. doi:10.1016/j.jcrs.2019.06.002
Carones F. Residual astigmatism threshold and patient satisfaction with bifocal, trifocal and extended range of vision intraocular lenses (IOLs). Open J Ophthalmol. 2017;7(1):1-7. doi:10.4236/ojoph.2017.71001
Davison JA, Simpson MJ. How does the ReSTOR lens work? Review Refr Surg. 2004:18-20.
Loicq J, Willet N, Gatinel D. Topography and longitudinal chromatic aberration characterizations of refractive-diffractive multifocal intraocular lenses. J Cataract Refract Surg. 2019;45(11):1650-1659. doi:10.1016/j.jcrs.2019.06.002
Sandoval HP, Lane S, Slade S, Potvin R, Donnenfeld ED, Solomon KD. Extended depth-of-focus toric intraocular lens targeted for binocular emmetropia or slight myopia in the nondominant eye: visual and refractive clinical outcomes. J Cataract Refract Surg. 2019;45(10):1398-1403. doi:10.1016/j.jcrs.2019.05.019
Sánchez-González JM, Sánchez-González MC, De-Hita-Cantalejo C, Ballesteros-Sánchez A. Small aperture IC-8 extended-depth-of-focus intraocular lens in cataract surgery: a systematic review. J Clin Med. 2022;11(16):4654. doi:10.3390/jcm1164654
Garg S, De Jesus MT, Fletcher LM, Chayet A, Barragán E, Casey P. Twelve-month clinical outcomes after implantation of a new, modular, anterior shape-changing fluid optic intraocular lens. J Cataract Refract Surg. 2022;48(10):1134-1140. doi:10.1097/j.jcrs.0000000000000935
Technology. JelliSee Ophthalmics, Inc. Accessed January 25, 2023. http://www.jellisee.com/technology.html

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.