Amniotic membranes: Clinical use for anterior segment disease
Several eye conditions may benefit from membrane application.
Most often, the placenta is discarded post partum, but some women choose to donate their placentas to an accredited tissue bank where they are thoroughly treated with antimicrobials before being processed for further use. (motortion / Adobe Stock)

Although the use of amniotic membranes (AMs) in eye care is relatively novel, the use of human placental tissue in medicine has been around for well over a century. In the early 1900s, human placental membranes were successfully utilized as a skin substitute. As technology and screening methods advanced, use of human placental membranes expanded across many medical disciplines including dentistry, podiatry, gynecology, plastics, urology, and orthopedics.1
The first documented use of human placental membranes in eye care was in 1940 when de Rotth reported success using an AM for the treatment of an ocular burn wound.2 Although the treatment was successful, the use of AMs then went out of favor until the early 1990s when improved processing and storage techniques were developed.
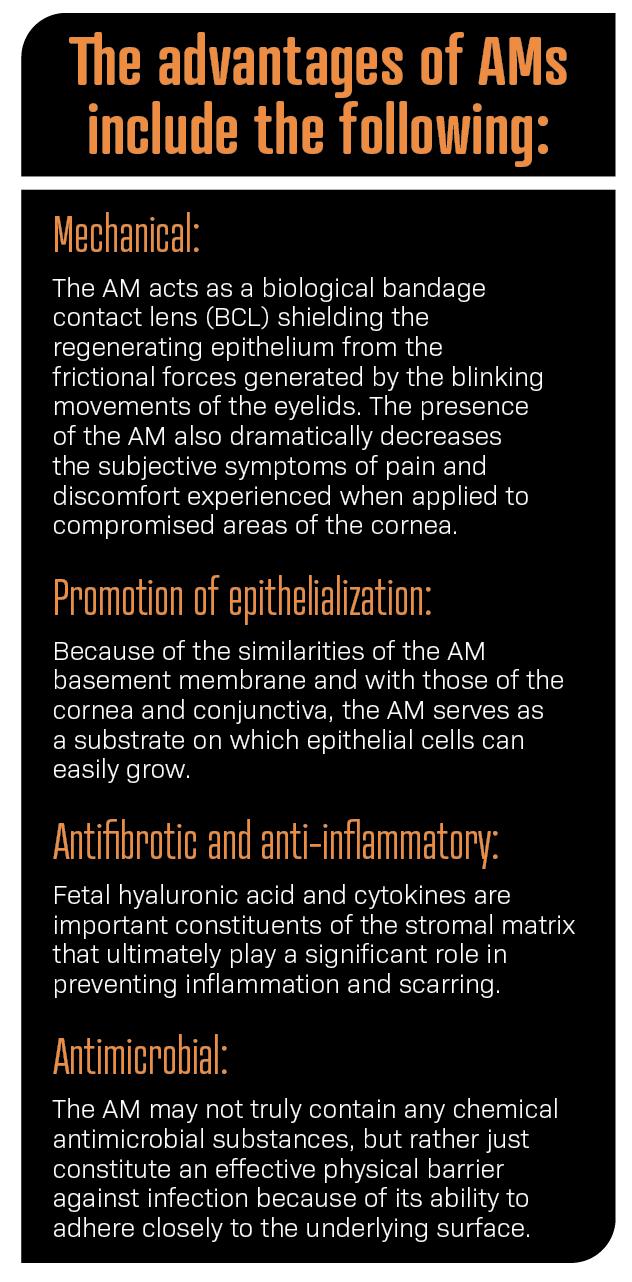
Advantages
The placenta is a remarkable, temporary organ that grows within the uterus, providing oxygen and nutrients to a growing fetus during pregnancy. Most often, the placenta is discarded post partum, but some women choose to donate their placentas to an accredited tissue bank where they are thoroughly treated with antimicrobials before being processed for further use.
The placenta consists of 2 layers—the amnion and the chorion. The chorion is the outer, vascular layer that is in direct contact with the uterine wall. The amnion is the inner, avascular layer which is in direct contact with the amniotic fluid. The amnion—one of the thickest membranes in the human body—consists of 3 layers: cuboidal epithelium, basement membrane, and stroma. The collagen makeup of the amniotic basement membrane is similar in composition to the basement membrane of the cornea and conjunctiva, creating an excellent foundation for accelerated healing after an ocular insult.
Preservation
Once the placental tissue has been treated and obtained from the tissue bank, the amnion and chorion are separated from each other by blunt dissection. The AM is then preserved by 1 of 2 methods: dehydration or cryopreservation.
Dehydration involves using a vacuum with low temperature heat to retain devitalized cellular components. However, this process is harsh and has been shown to cause protein denaturation, loss of function, and irreparable structural damage. Dehydrated AMs are FDA approved for wound coverage only. They have a shelf life of up to 5 years and do not require refrigeration during storage. These are applied to the eye in conjunction with a BCL.
Cryopreservation involves slow-rate freezing in order to avoid ice formation. This preservation technique retains the extracellular matrix components, such as heavy-chain hyaluronic acids, growth factors, fibronectin, and collagen, all of which promote anti-inflammatory effects and healing. The AM is then attached to a polycarbonate ring. The combination of the AM and ring are applied directly onto the eye. Cryopreserved AMs are cleared by the FDA as a class II medical device and are approved for use in wound coverage and healing. They have a shelf life of up to
2 years and require refrigeration or freezing for storage. If frozen, the AM must be thawed prior to use.
Clinical applications
There are a plethora of potential uses of AMs in clinical practice but, unfortunately, AMs are not routinely considered first-line therapy for any acute condition in eye care. In fact, according to the Centers for Medicare & Medicaid Services 2016 Provider Utilization and Payment Data, only 314 doctors of optometry reported the CPT code 65778 (amniotic membrane insertion). This equates to less than 1% of practicing optometrists in the United States.
Use of an AM can be considered in any clinical scenario when the practitioner desires to promote faster healing, decrease inflammation, and prevent scarring. AMs can be incredibly advantageous in the management of several eye conditions, including corneal abrasions, recurrent corneal erosions (RCE), corneal ulcers, and dry eye disease (DED).
An RCE is characterized by a disturbance at the level of the corneal epithelial basement membrane, resulting in defective adhesions and recurrent breakdown of the epithelium. Patients with RCEs often show increased levels of enzymes such as matrix metalloproteinases (MMPs) that dissolve the basement membrane and its anchoring components including integrins, laminin, and type VII collagen. RCE is caused most commonly by mechanical trauma to the superficial cornea, resulting in a corneal abrasion, and is also seen in patients with Epithelial Basement Membrane Dystrophy (EBMD).3 Use of an AM protects the cornea from eyelid trauma while encouraging epithelial regrowth and adhesion. In addition, AMs contain inhibitors of MMPs and active matrix components including collagen type VII and laminin, essential for regenerative healing and prevention of recurrence.
AMs have been used successfully in nonhealing infectious ulcers due to bacteria, fungi, viruses, and protozoa. The nonhealing of the ulcer despite sufficient antimicrobial treatment in these cases may be due to the release of proinflammatory mediators, proteolytic enzymes, and collagenases by the microorganisms. The use of an AM is intended to impede protease activity and promote re-epithelialization and faster healing in hopes of avoiding cornea transplantation. Data from one study consisting of 149 patients with nonhealing corneal ulcers showed that 70% of patients achieved sufficient epithelial closure with a single AM. Treatment failure was observed in 30% of patients. The highest closure rates were found in bacterial ulcers, herpetic ulcers, and neurotrophic ulcers, whereas the lowest closure rates were found in ulcers after corneal surgery and ulcers associated with rheumatic disease.4 AMs can also be considered as adjunctive therapy in normal corneal ulcers, especially when they are located within the visual axis and are associated with a notable inflammatory response.
The Dry Eye Amniotic Membrane (DREAM) study consisted of 97 eyes of 84 patients who exhibited severe signs and symptoms of DED despite maximum medical and pharmaceutical interventions. After cryopreserved AM treatment for approximately 5 days, 88% of patients demonstrated an improved ocular surface along with a notable average reduction in their Dry Eye Workshop (DEWS) score. Only 10% of eyes required repeated treatment to complete healing. There were no significant adverse events reported in this study.5 In addition, the Tear Film & Ocular Surface Society (TFOS) DEWS II has recognized AMs as a viable treatment option in stage 4 of their evidence-based, multistaged management algorithm of DED.6
Patient management tips
After application of the AM, patients should be instructed to avoid rubbing the eyes to prevent secondary injury. The patient may need to avoid driving because vision in the eye with the AM will be significantly reduced.
Topical medications can be used concurrently, as medication penetration has not been found to be an issue with AMs. Sodium Fluorescein can be applied to assess the cornea with a cryopreserved AM but not with a dehydrated AM because of the BCL. In addition, IOP can be assessed with a noncontact or rebound tonometer.
Patients generally tolerate an AM well, but the most common complaint is discomfort, especially due to the awareness of the polycarbonate ring of the cryopreserved AM. To mitigate this awareness, a temporary lid tarsorrhaphy can be helpful.
Prior to application, the cryopreserved AM must be thoroughly rinsed off with saline to remove the storage solution containing glycerol. Otherwise, the patient will experience a severe burning sensation from the glycerol.
The follow-up schedule varies from patient to patient depending on the diagnosis. Essentially, the follow-up is to determine whether the membrane has been dissolved by the eye. Eyes with mild anterior segment disease may take 5 to 7 days, whereas those with severe cases may have dissolution within 24 hours.
Coding and billing
When coupled with an appropriate diagnosis code, the CPT code for placement of an AM on the ocular surface for wound healing is 65778. Reimbursement for this code already includes compensation for the office visit (either 920XX or 992XX) related to the decision to perform this procedure. There is a zero-day global period, thus each follow-up is billable as long as general requirements for an office visit are met.
Conclusion
Although underutilized in optometry, AMs can improve clinical outcomes in many cases of anterior segment disease. Their benefits far outweigh their risks and should be considered whenever the clinician is seeking faster healing, reduced inflammation, and scar prevention.
References
1. Davis JW. Skin transplantation with a review of 550 cases at the Johns Hopkins Hospital. Johns Hopkins Med J. 1910;15:307-396.
2. de Rotth A. Plastic repair of conjunctival defects with fetal membranes. Arch Ophthalmol. 1940;23:522-525. doi:10.1001/ARCHOPHT.1940.00860130586006
3, Miller DD, Hasan SA, Simmons NL, Stewart MW. Recurrent corneal erosion: a comprehensive review. Clin Ophthalmol. 2019;13:325-335. doi:10.2147/OPTH.S157430
4. Schuerch K, Baeriswyl A, Frueh BE, Tappeiner C. Efficacy of amniotic membrane transplantation for the treatment of corneal ulcers. Cornea. 2020;39(4):479-483. doi:10.1097/ICO.0000000000002179
5. McDonald MB, Sheha H, Tighe S, et al. Treatment outcomes in the DRy Eye Amniotic Membrane (DREAM) study. Clin Ophthalmol. 2018;12:677-681. doi:10.2147/OPTH.S162203
6. Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017;15(3):575-628. doi:10.1016/j.jtos.2017.05.006

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.