Blue light: Why it matters

The topic of light-related damage to the eyes and adnexa has garnered more attention in recent years. Ultraviolet (UV) light damage has, for much time, been a concern because the incidence of sun damage (sunburn, skin cancers) has steadily been increasing.1
In parallel fashion, blue light has been studied and discussed in light of the widespread use of modern light bulbs and digital devices that emit blue light.
Related: Bad blue light, macular pigment, and prescriptive carotenoids
Spectrum of light
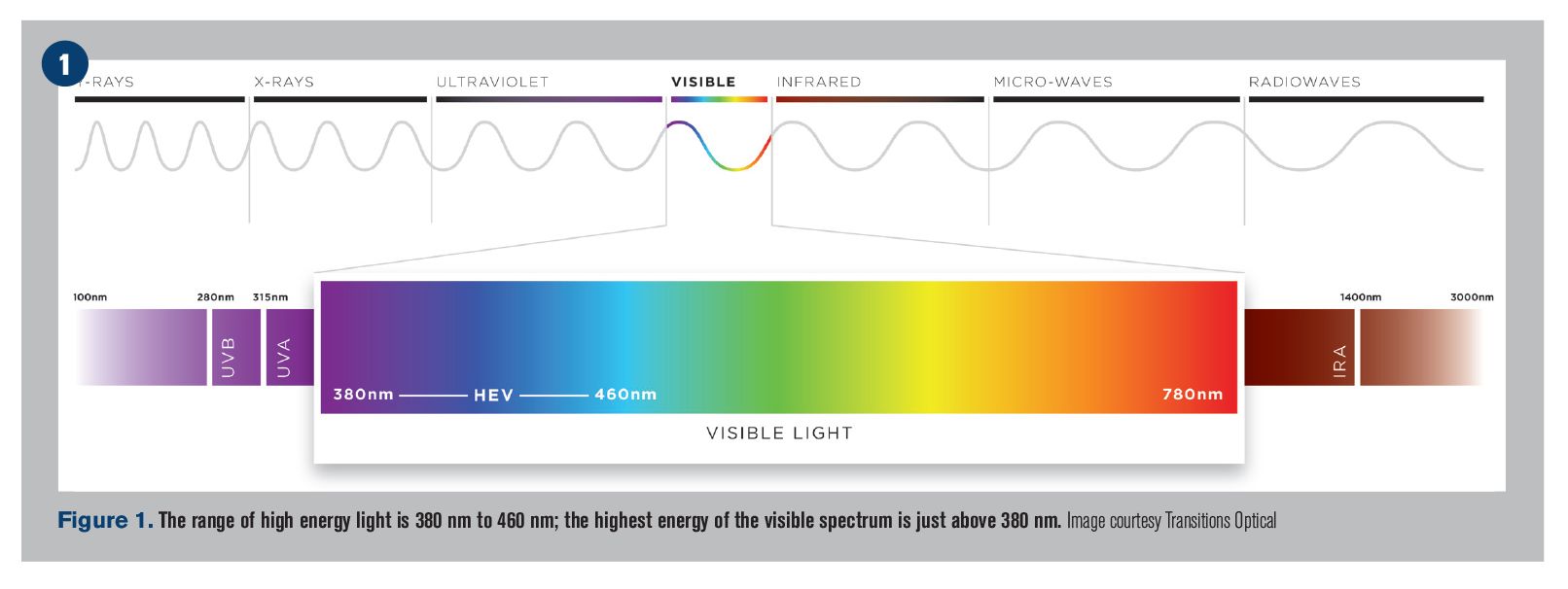
The light spectrum contains much more than what humans can see. Frequencies of light include microwaves, radio waves, and X-rays, to name a few.
The visible spectrum has only a very thin portion of wavelengths between 380 nm and 780 nm. The highest energy of the visible spectrum is immediately adjacent to the UV spectrum and is just above 380 nm (the range of high energy light is 380 nm to 460 nm).2
This high energy blue light scatters in our atmosphere and is the reason why the sky appears blue.
Blue light is also produced by light-emitting diodes (LEDs), which are more common than ever before. Because of LED efficiencies, traditional incandescent light bulbs have been replaced by LED bulbs in recent years. LED lighting is widely found in digital technologies, such as televisions, phones, and tablets for commercial usage.
This topic has come under scrutiny as the usage of digital devices increases more and more each year (and by younger individuals each year). A 2016 Vision Council report found that 60 percent of Americans use digital devices for more than five hours each day, and 70 percent of those use at least two or more devices at one time.3
Ocular light transmission
From an ocular health perspective, it has been long known that blue light is toxic to certain ocular structures.4 As we age, the ocular risk can change and shift. The longer the wavelength, the higher the proportion of light that passes through the cornea and reaches the lens and retina.
On average, the human cornea absorbs wavelengths below 300 nm, and the lens absorbs less than 400 nm.5 Upon closer analysis, though, these numbers change throughout life-a clear crystalline lens at birth and in childhood years transmits light at 300 nm+, whereas an adult (and more yellow crystalline lens) transmits at 400n m+.
Protection of children’s eyes is then especially important because light transmittance is higher at a younger age, allowing higher levels of UV and blue light to reach the lens and retina.6
The retina is at a higher risk as it absorbs light over 400 nm.7 Given that the spectrum of high-energy blue light is known to be 380 nm to 460 nm, there is a portion of blue light that is problematic. Ocular exposure to light around 435 nm (±20 nm) can induce irreversible cell death in the retinal pigment epithelium (RPE).2
Related: Sunlight and its effect on eye health
Blue light research
Historically, several large-scale population studies demonstrated the ocular risk to blue light.
First, the Chesapeake Bay waterman study had several iterations of meta-analysis and an association was identified between cumulative blue light exposure and age-related macular degeneration (AMD).8
Similarly, the Beaver Dam Eye Study concluded that exposure to bright visible light might be associated with AMD.9
Finally, the Visual Impairment Project suggested that individuals with more sunlight exposure are at a significantly increased risk for AMD.7
As such, sunlight (and more specifically, cumulative blue light) has been identified as a risk factor for AMD. A specific photosensitive visual pigment appears to be involved in this retinal toxicity, and it is referred to as A2E (N-retinylidene-N-retinylethanolamine).
A 2013 study defined the most toxic wavelengths of light in an in-vitro model. The researchers’ conclusion was that the most loss of retinal cell viability occurred between 415 nm and 455 nm.2
What is additionally worrisome is that retinal cell death occurs via apoptosis (a continual cascade of death of neighboring cells) and likely causes AMD to be so visually destructive.10
Also by Dr. Lievens: Video: Why contact lens wearers should use hydrogen peroxide
Sun and sleep
Confusion exists about where the risk of ocular damage originates. Blue light emits from the sun, digital devices, and LEDs; know that the sun provides a much greater amount of blue light than digital devices or LEDs.11
Though we spend many hours per day on illuminated screens and computer technologies, it has been proposed that the blue light hazard from said devices may not approach dangerous limits.12
What is known, though, is that digital device usage can wreak havoc on our sleep patterns by interfering with human circadian rhythms.
In the absence of blue light, ganglion cells in the human retina stimulate the pineal gland to release melatonin, a hormone which lets our bodies know it is time for sleep. This is in contrast to the presence of blue light, which suppresses melatonin production-our bodies are alert, energized, and ready for work and play. This can be a challenge because many Americans look at their digital devices right before bed.
What ODs can do
Blue light protection is becoming a common topic, and some patients are aware of it. Similarly, ultraviolet (UV) protection is widely known, but a specific consideration to protect the eyes against UV rays is limited at best.
Fortunately, these two topics are easy to discuss together. Protections for both blue light and UV have been combined into singular products. This results in a quick and seamless doctor-patient discussion and resonates very well.
Given the ocular risks from UV light and the increasing usage of digital devices (albeit a lower blue light risk), patients need to know how to protect themselves. Spectacle lenses that protect against both forms of light are easy to prescribe. Part of ODs’ responsibility of patient care is to look for opportunities to prevent problems. This is a prime example of that.
Read/listen to more about Dr. Lievens
About the author
Dr. Lievens worked in private practice and an ophthalmology referral center, and he served in the United States Air Force. He is the cocreator of the funduscopic grading card and is a Region Chair of the American Academy of Optometry’s Admittance Committee. Dr. Lievens is an avid sports fan and exercise enthusiast. He and his wife routinely attempt to combine the fun of exercise with the thrill of dressing up for the gym by working out in costumes.
clievens@sco.edu
References:
1. Rogers HW, Weinstock MA, Harris AR, Hinckley MR, Feldman SR, Fleischer AB, Coldiron BM. Estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol. 2010 Mar;146(3):283-287.
2. Arnault E, Barrau C, Nanteau C, Gondouin P, Bigot K, Viénot F, Gutman E, Fontaine V, Villette T, Cohen-Tannoudji D, Sahel JA, Picaud S. Phototoxic action spectrum on a retinal pigment epithelium model of age-related macular degeneration exposed to sunlight normalized conditions. PLoS One. 2013 Aug 23;8(8):e71398.
3. The Vision Council. Digital Eye Strain. Available at: https://www.thevisioncouncil.org/content/digital-eye-strain. Accessed 2/12/19.
4. Braunstein RE, Sparrow JR. A blue-blocking intraocular lens should be used in cataract surgery. Arch Ophthalmol. 2005 Apr;123(4):547-9.
5. Pescosolido N, Barbato A, Giannotti R, Komaiha C, Lenarduzzi F. Age-related changes in the kinetics of human lenses: prevention of the cataract. Int J Ophthalmol. 2016 Oct 18;9(10):1506-1517.
6. Behar-Cohen F, Baillet G, de Ayguavives T, GarcÃa PO, Krutmann J, Peña-GarcÃa P, Reme C, Wolffsohn JS. Ultraviolet damage to the eye revisited: eye-sun protection factor (E-SPF), a new ultraviolet protection label for eyewear. Clin Ophthalmol. 2014;8:87-104.
7. Yam JC, Kwok AK. Ultraviolet light and ocular diseases. Int Ophthalmol. 2014 Apr;34(2):383-400.
8. Taylor HR, West S, Muñoz B, Rosenthal FS, Bressler SB, Bressler NM. The long-term effects of visible light on the eye. Arch Ophthalmol. 1992 Jan;110(1):99-104.
9. Klein BE, Howard KP, Iyengar SK, Sivakumaran TA, Meyers KJ, Cruickshanks KJ, Klein R. Sunlight exposure, pigmentation, and incident age-related macular degeneration. Invest Ophthalmol Vis Sci. 2014 Aug 14;55(9):5855-61.
10. Sparrow JR, Nakanishi K, Parish CA. The lipofuscin fluorophore A2E mediates blue light-induced damage to retinal pigmented epithelial cells. Invest Ophthalmol Vis Sci. 2000 Jun;41(7):1981-9.
11. Okuno T, Saito H, Ojima J. Evaluation of blue-light hazards from various light
sources. Dev Ophthalmol. 2002;35:104-12.
12. O’Hagan JB, Khazova M, Price LL. Low-energy light bulbs, computers, tablets and the blue light hazard. Eye (Lond). 2016 Feb;30(2):230-3.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.