Amniotic membrane grafts help ocular surface disease
Inflammation is the hallmark symptom of all ocular surface disease, including dry eye disease (DED). Uncontrolled inflammation leads to chronic pain and irritation as well as delayed healing, tissue damage, and vision-threatening complications such as scarring and haze.1
Effective control of inflammation is an important strategy to promote healing and is fundamental to my treatment paradigm. I have a thriving DED practice within a cornea practice, and every day I see at least one patient seeking dry eye relief despite compliant use of various palliative measures.
Using amniotic membrane
Like many other optometrists, I have embraced the use of amniotic membrane (AM) tissue to control inflammation and rehabilitate the ocular surface for select DED patients as well as those who have keratitis, conjunctivitis, and blepharitis. A decade of experience and impressive outcomes with AM tissue supports my ongoing reliance on this therapeutic intervention, and a growing body of evidence validates my anecdotal observations.
As a proponent and successful user of AM tissue, I sometimes facilitate workshops on this topic. My key message at these events is that there are various types of AM tissue for ophthalmic use, and eyecare providers should try them all. By doing so, clinicians can see for themselves which products provide better clinical results and which fit in best with their overall practice dynamics.
Previously by Dr. Whitley: 4 steps to beating blepharitis
For optometrists who suspect that implanting AM grafts is beyond their level of expertise, nothing could be further from the truth. Implanting an AM tissue graft is as clear cut as applying a contact lens or inserting a punctal plug. When offering patients the option of AM tissue grafts, it can be reassuring to convey that the insertion process is simple.
That being said, it is equally important to manage patient expectations. Let patients know that dry eye is a chronic condition and that while the AM tissue is not a cure-all, it will play a key role among the multiple methods that can be used to manage their conditions.
Cryopreserved vs dehydrated
Cryopreserved AM and dehydrated AM are the two types of AM tissue grafts available for ophthalmic use.
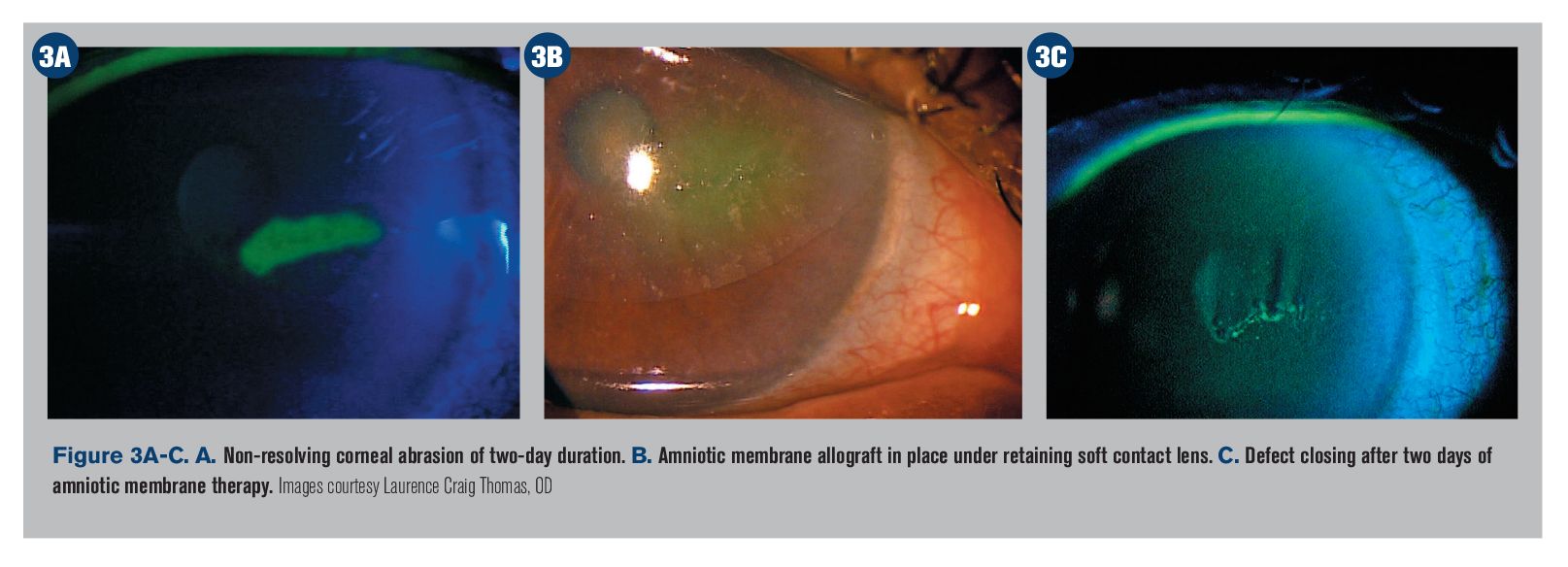
Prokera (Bio-Tissue) is the only cryopreserved ophthalmic AM tissue availabe, whereas several different dehydrated AM tissue grafts are available, including AmbioDisk (Katena) and BioDOptix (Integra LifeSciences).
AM extract autologous serum eye drops are also an option (Regener-Eyes, Regenerative Network International; Genesis; Ocular Science), but they differ from pre-shaped, ready-to-place AM tissue grafts.
The primary difference between the two AM tissue categories is how they are preserved. Cryopreserved AM (CAM)-Prokera-must be kept frozen, then brought to room temperature before application. Conversely, heat or chemical processes are used to preserve dehydrated AM (DAM), which is stored at room temperature and must be rehydrated for clinical use.
Related: Using amniotic membrane in the primary care office
Prokera is a self-retaining biologic corneal bandage that is fastened to an ophthalmic conformer ring that keeps the graft in place.
Placing Prokera takes a few simple steps.
I rinse the graft with sterile saline solution to prevent potential stinging from the preservation media and apply topical anesthetic.
Then, I hold the upper eyelid, ask the patient to look down, and insert Prokera into the superior fornix.
Next, I pull the lower eyelid down, slide Prokera under the lower eyelid, and check centration under the slit lamp.
Tape tarsorrhaphy is optional, but it’s a step that I always include because it helps keep the lid closed, keeps the device in place, and enhances comfort by preventing the patient from blinking.
The membrane dissolves as healing occurs. In my clinical experience, more inflammation there is, the faster the membrane will dissolve and releases its biological factors.
I usually follow up with patients in one week, but the membrane may dissolve in as few as two to three days.
In cases where the graft is still in place at the one-week follow-up, removal is simple: I apply topical anesthetic, pull the lower eyelid down, lift the lower edge of Prokera using a cotton swab or forceps, ask the patient to look down, apply gentle pressure on the upper eyelid, and slide Prokera out.
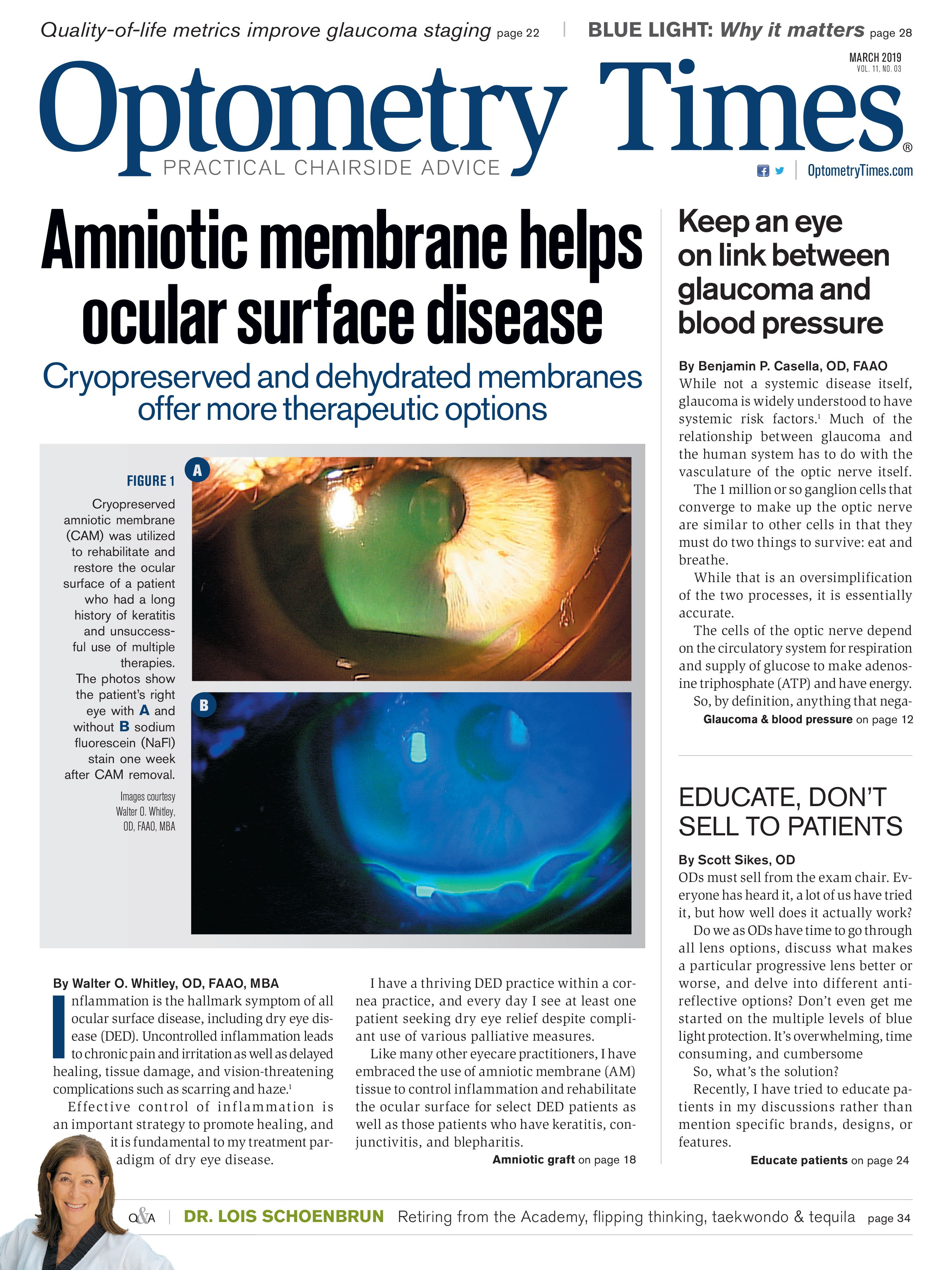
Placing dehydrated AM requires additional tools, such as a lid speculum, a Weck-Cel sponge, and a bandage contact lens.
A bandage lens must be placed on top of the membrane to keep it fixated. Some dehydrated AMs are packaged along with a contact lens; these AMs cannot be used with any bandage lens, only the accompanying lens.
With dehydrated AM graft, apply topical anesthetic, insert a speculum; debride the cornea if indicated; place the membrane basement side down with forcepts; center Weck-Cel sponge; place a bandage contact lens on top of it, making sure both are centered; and finally remove the speculum, making sure to avoid disturbing placement of the membrane or contact lens.
Related: Amniotic membrane in ocular surface disease
The science
AM tissue is a disease-modifying therapy that aids corneal epithelialization, reduces inflammation and fibrosis, prevents structural damage, and boasts antimicrobial properties.2
Many of the beneficial effects of AM are attributed to biomolecules, including fibronectin; hepatocyte growth factor (HGF); epidermal growth factor (EGF); basic fibroblast growth factor (bFGF); transforming growth factor (TGF); and collagen types I, III, IV, and V, which are a direct source of corneal regeneration.3,4
This cocktail of natural cytokines enhances tissue thickness, provides a scaffold for epithelialization, and enhances capillary formation-essentially stimulating growth to repair and restore soft tissue.5,6 What’s more, AM expresses HLA-G, which gives it the ability to graft damaged tissue without triggering an immune response,7 and naturally blocks the TGF-β receptor responsible for scar tissue development.8
While studies show that AM is imbued with these influential cellular power brokers, the anti-inflammatory and regenerative properties associated with these biologics are retained in different amounts or lost depending on the preservation process used.
For instance, cryopreserved AM contains (HC)-hyaluronan (HA)/pentraxin 3 (PTX3), the biological compound that is associated with AM’s antiinflammatory, antiscarring, and regenerative properties.9,10 HC-HA/PTX3 is not, however, present in dehydrated amniotic tissue.11 This distinction is borne out in the U.S. Food & Drug Association (FDA) labeling of these products: Prokera cryopreserved AM is the only tissue cleared by the FDA for its protective, wound healing, and anti-inflammatory effects.12
Relevant research
A 2018 retrospective study demonstrated that a single application of Prokera self-retained cryopreserved amniotic membrane (CAM) can accelerate the recovery of the corneal surface and help reduce signs and symptoms of DED for at least three months.13
This study, known as the Dry Eye and Amniotic Membrane (DREAM) study (not to be confused with the other well-known dry eye DREAM study14), looked at 97 eyes of 84 patients who exhibited severe DED despite maximal medical treatments including topical artificial tears, cyclosporine-A, serum, antibiotics, and steroids. Study participants exhibited superficial punctate keratitis, filamentary keratitis, exposure keratitis, neurotrophic keratitis, and corneal epithelial defect.
After 5.4 days of CAM treatment, patients demonstrated an improved ocular surface along with a notable reduction of the severity of their overall Dry Eye Workshop (DEWS) score.13 These findings are consistent with previous studies.15,16
Related: Treating inflammation tackles filamentary keratitis
AM in my practice
I typically use AM for moderate-to-severe DED patients. If they have been prescribed anti-inflammatory eye drops and oral omega-3 supplements, performed lid hygiene, and had their meibomian glands expressed, but I have not seen healing after one month or more, I will recommend AM.
I always start with CAM and move to DAM only in rare cases in which the patient is intolerant of the conformer ring with CAM. When a patient complains of irritation, it often dissipates within 24 hours.
It has been suggested that proteins in the cryopreserved preparations are more plentiful and active,17 and the consistently successful results seen in my practice suggest this is true. However, I also see remarkable results from DAM in select patients.
Keep in mind that when AM is used with recalcitrant DED patients who have advanced disease, at times patients will require several AM tissue grafts consecutively or over a period of months. That doesn’t mean the membrane didn't work; it means the patient has advanced surface disease.
Nerve regeneration
Patients who have neuropathic corneal pain are also ideal candidates for AM grafts.
Morkin and colleagues found that neuropathic corneal pain due to damaged trigeminal nerve terminals significantly improved by about 72 percent within an average of six days of CAM treatment.16
Patients who found the graft uncomfortable and had it removed within four days still showed 63 percent improvement in pain scores even with the abbreviated placement. In this study, corneal nerve regeneration was shown via confocal microscopy.18
John was the first to show that CAM’s increase in corneal nerve density and improved corneal sensitivity is correlated with corneal nerve regeneration.15 Before this study, no therapeutic modality had been shown to regenerate corneal nerves.
In the study, patients exhibited a significant increase in central corneal nerve density for up to three months as well as significant improvement in their DEWS score, pain score, tear film break-up time, fluorescein staining, and Standard Patient Evaluation of Eye Dryness (SPEED) score.
Researchers surmise that the lasting effect of a placement of CAM for DED may be attributed to corneal nerve regeneration given that corneal nerves play a vital role in epithelial regeneration and tear film stability through reflex tearing and blinking.
Related: Using the SPEED questionnaire to identify dry eye
Conclusion
It’s important for ODs to evaluate all available AM technology. While there is considerable literature about natural AM and CAM, there is less research about DAM, which makes it necessary to apply a hands-on approach to weigh its pros and cons.
In my opinion, CAM offers a solid body of evidence supporting its ability to heal the ocular surface, initiate corneal nerve regeneration, and improve the signs and symptoms of DED, and my own anecdotal observations support this. DAM, too, is effective at improving the signs and symptoms of DED-in my hands and according to anecdotal reports.
Ultimately, eyecare providers need to try cryopreserved and dehydrated AM, review the literature, and challenge themselves to decide how to incorporate these tools into their practices to offer additional treatment options to their patients.

References:
1. Rhee MK, Mah FS. Inflammation in Dry Eye Disease: How Do We Break the Cycle? Ophthalmology. 2017 Nov;124(11S):S14-S19.
2. Talmi YP, Sigler L, Inge E, Finkelstein Y, Zohar Y. Antibacterial properties of human amniotic membranes. Placenta. 1991 May-Jun;12(3):285-8.
3. Nakamura T, Yoshitani M, Rigby H, Fullwood NJ, Ito W, Inatomi T, Sotozono C, Nakamura T, Shimizu Y, Kinoshita S. Sterilized, freeze-dried amniotic membrane: a useful substrate for ocular surface reconstruction. Invest Ophthalmol Vis Sci. 2004 Jan;45(1):93-9.
4. Dudok DV, Nagdee I, Cheung K, Liu H, Vedovelli L, Ghinelli E, Kenyon K, Parapuram S, Hutnik CM. Effects of amniotic membrane extract on primary human corneal epithelial and limbal cells. Clin Exp Ophthalmol. 2015 Jul;43(5):443-8.
5. Grzywocz Z, Pius-Sadowska E, Klos P, Gryzik M, Wasilewska D, Aleksandrowicz B, Dworczynska M, Sabalinska S, Hoser G, Machalinski B, Kawiak J. Growth factors and their receptors derived from human amniotic cells. Folia Histochem Cytobiol. 2014;52(3):163-70.
6. Koizumi NJ, Inatomi TJ, Sotozono CJ, Fullwood NJ, Quantock AJ, Kinoshita S. Growth factor mRNA and protein in reserved human amniotic membrane. Curr Eye Res. 2000 Mar;20(3):173-7.
7. Kubo M, Sonoda Y, Muramatsu R, Usui M. Immunogenicity of human amniotic membrane in experimental xenotransplantation. Invest Ophthalmol Vis Sci. 2001 Jun;42(7):1539-46.
8. Lee SB, Li DQ, Tan DT, Meller DC, Tseng SC. Suppression of TGF-Ã signaling in both normal conjunctival fibroblasts and pterygial body fibroblasts by amniotic membrane. Curr Eye Res. 2000 Apr;20(4):325-34.
9. He H, Zhang S, Tighe S, Son J, Tseng SC. Immobilized heavy chain-hyaluronic acid polarizes lipopolysaccharide-activated macrophages toward M2 phenotype. J Biol Chem. 2013 Sep 6;288(36):25792-803.
10. Tseng SC. HC-HA/PTX3 purified from amniotic membrane as novel regenerative matrix: insight into relationship between inflammation and regeneration. Invest Ophthalmol Vis Sci. 2016 Apr 1;57(5):ORSFh1-8.
11. Cooke M, Tan EK, Mandrycky C, He H, O'Connell J, Tseng SC. Comparison of cryopreserved amniotic membrane and umbilical cord tissue with dehydrated amniotic membrane/chorion tissue. J Wound Care. 2014 Oct;23(10):465-74.
12 U.S Food & Drug Administration. Prokera 510(k) approval documents. Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf3/k032104.pdf. Accessed 2/25/19.
13. McDonald MB, Sheha H, Tighe S, Janik SB, Bowden FW, Chokshi AR, Singer MA, Nanda S, Qazi MA, Dierker D, Shupe AT, McMurren BJ. Treatment outcomes in the DRy Eye Amniotic Membrane (DREAM) study. Clin Ophthalmol. 2018 Apr 9;12:677-681.
14. Asbell PA, Maguire MG, Peskin E, Bunya VY, Kuklinski EJ; Dry Eye Assessment and Management (DREAM) Study Research Group. Dry Eye Assessment and Management (DREAM) Study: Study design and baseline characteristics. Contemp Clin Trials. 2018 Aug;71:70-79.
15. Cheng AM, Zhao D, Chen R, Yin HY, Tighe S, Sheha H, Casas V, Tseng SC. Accelerated restoration of ocular surface health in dry eye disease by self-retained cryopreserved amniotic membrane. Ocul Surf. 2016 Jan;14(1):56-63.
16. John T, Tighe S, Sheha H, Hamrah P, Salem ZM, Cheng AMS, Wang MX, Rock ND. Corneal nerve regeneration after self-retained cryopreserved amniotic membrane in dry eye disease. J Ophthalmol. 2017;2017:6404918.
17. Chua L, Cooke M, Mandrycky C, Tan EK, O'Connell J, Tseng S, McDevitt T. Biological differences between cryopreserved and dehydrated amniotic membrane tissue grafts. Invest Ophthalmol Vis Sci. 2013 June;54(15):3894.
18. Morkin M, Hamrah P. Efficacy of self-retained cryopreserved amniotic membrane for treatment of neuropathic corneal pain. Ocul Surf. 2018 Jan;16(1):132-138.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.