Contact lens overwear leads to short-term, long-term consequences
A patient presents with ocular issues from the overuse of contact lens for months
“When in doubt, take ‘em out.” That phrase should be put on at least three billboards in every county in America.
You can see where this is headed …
I was having somewhat of an interval in the middle of a busy afternoon when a patient — who was new to us — walked in with a red eye. She was a 47-year-old African American female who wore contact lenses and had been experiencing contact lens intolerance, redness, burning, and light sensitivity in her right eye for about three weeks.
Her medical history was remarkable for systemic hypertension of several years’ duration for which she was taking an angiotensin-converting enzyme (ACE) inhibitor. She reported no known medication allergies.
Related: How to drop a vision plan and replace revenue
She did report a history of “eye issues” in both eyes off and on for several years and that she wore her soft contact lenses continuously for a month or two before removing them. She had no idea how old her current contact lenses were.
Patient examination
Entering visual acuities (VA) through her habitual soft contact lenses was 20/25-1 in the right eye and 20/20-1 in the left. Pupil function was unremarkable for each eye. Examination of her left eye’s anterior segment was unremarkable except for seven old stromal scars. Two were near her visual axis. Her right eye’s anterior segment was remarkable for grade 1+ injection of her bulbar conjunctiva.
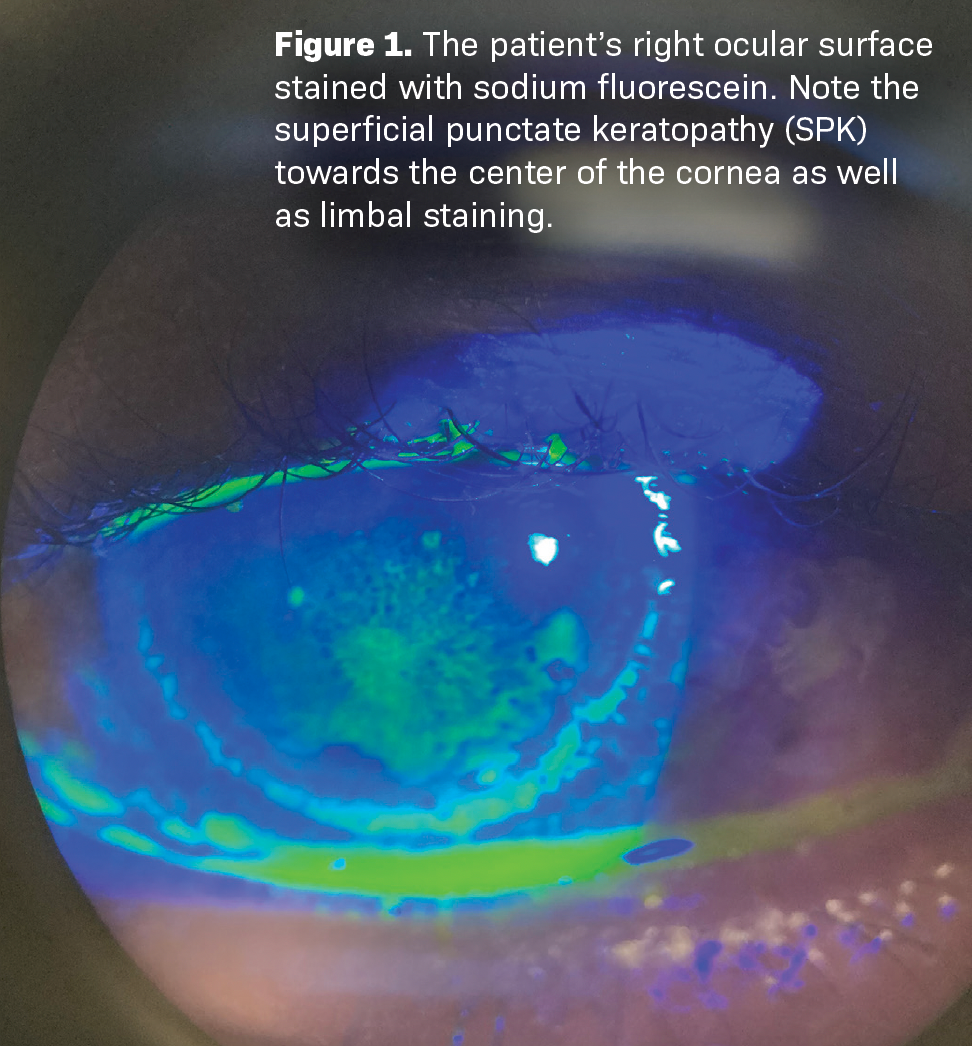
Her cornea was remarkable for diffuse superficial punctate keratopathy (SPK) affecting her central cornea and some fluorescein staining around her limbus (see Figure 1). There was no active ulceration. There were five old and inactive stromal scars. Intraocular pressure (IOP) by means of rebound tonometry was 19 mmHg in the right eye and 18 mmHg in the left.
Related: How implementing a hiring process netted a great staff
At that point, I explained to the patient that over-wearing her contact lenses was the cause of the inflammation and its ensuing signs and symptoms. I advised her to discard her current contact lenses and to wear spectacles only at least while I treated her.
She then informed me that she had no spectacles and had not had any for one or two years. I asked her if she could get by with a contact in just her left eye (the unaffected one). She said she had tried that before and that she could not handle it due to headaches.
I asked her what the powers of her contact lenses were, and she did not know. So, I placed her behind the phoropter, completed a quick dry retinoscopy, and refracted her to -3.50 DS in the right eye and -4.00 DS in the left.
I gave her a copy of her prescription and advised her to go to an optical in town that had same-day service on new spectacle prescriptions and to get some that day. I also gave her a sample of a topical fluoroquinolone to be used every two hours while awake and invited her to return the following day for me to recheck her eyes.
The following day, she did return. She had not purchased any spectacles and was not wearing any contact lenses.
Related: 5 marketing tips to grow a practice without breaking the bank
She stated that her eye felt much better since starting the drops. Entering VAs unaided were 20/200 in each eye. Behind the phoropter they were 20/20-1 in each eye. Pupil function was again unremarkable, and IOP was 16 mmHg in the right eye and 18 mmHg in the left. The bulbar conjunctival injection in her right eye was now trace. Her SPK in the central cornea was resolved, and her limbal staining was much improved.
At that point, I instructed her to continue her drops every two hours while awake in the right eye and invited her back in two days for another follow-up appointment. I have not seen nor heard from her since.
Conclusion
My tentative long-term plan for this patient would be to get her eyes back to baseline, and then explain to her that spectacles would be best moving forward.
If she insisted on contact lenses, I would implore her to wear nothing expect for daily disposables and to wear them as instructed.
Eyes can be relatively straightforward from time to time. The patients to whom they belong can be a different story.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.
