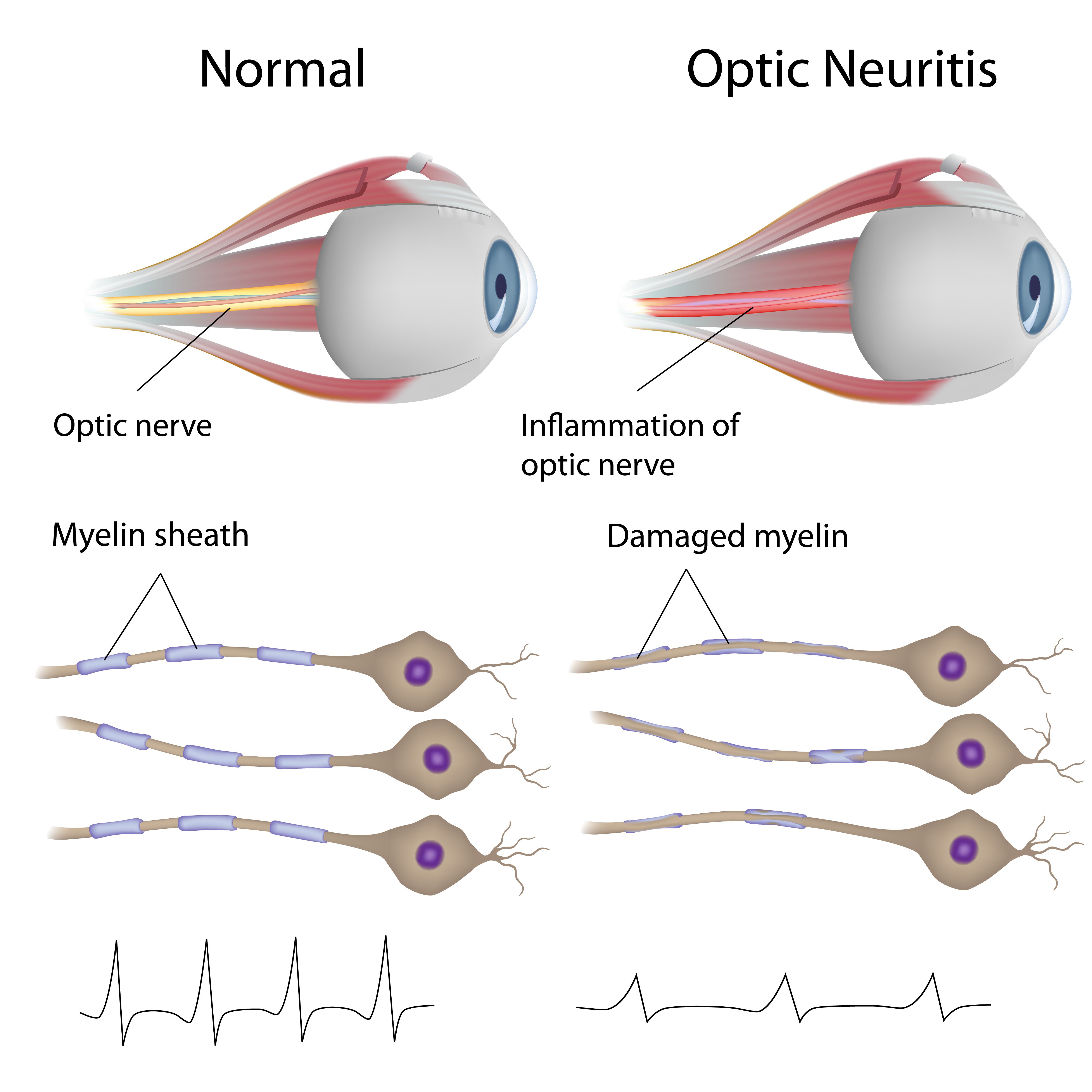
Optic Neuritis and COVID-19 vaccine connection?
At this stage, most people have decided whether they will get a COVID-19 vaccine. I am happy that the number of people in the United States—specifically my home state of Georgia—who are fully vaccinated continues to go up. So I suppose people are still being persuaded.
After-hours phone call
I received a phone call a couple weeks ago around 9:30 PM . When you own a 2-lane practice with 5 employees, the after-hours line is straightforward: Someone calls, and my left pocket vibrates. This call came from a woman in her 20s who was complaining of odd visual disturbances and a feeling of pressure around her left eye, which started 3 days after receiving her second COVID-19 vaccine.
I met her at my office around 9:45 PM that night. Her medical history was unremarkable. She had a history of diabetes on 1 side of the family and wore glasses at times. She stated these symptoms were gradually worsening over the past 24 hours and that she was becoming concerned.
Entering visual acuities unaided were 20/25 in the right eye and 20/30 in the left. IOPs were in the teens in each eye. Confrontation visual fi elds were full in each eye, and extraocular muscle function was normal. Amsler grid testing revealed a splotchy relative scotoma in the left eye’s central vision.
Dilated fundus examination showed an unremarkable right eye and a very swollen optic nerve in the left eye. Then came the questions in light of an optic neuritis diagnosis. I asked whether she was sure this started after her COVID-19 vaccine. She was certain. I asked whether she felt numbness or tingling or experienced heat intolerance. That is when we hit the nail on the head.
She reported feeling numbness in her legs for years, which was exacerbated by too much time on her feet. She was referred to a neurologist for a multiple sclerosis workup several years ago but did not keep the appointment.
I informed the patient that multiple sclerosis was high on the list of differential diagnoses, and I was able to get her into the hospital the next morning for treatment and a subsequent work-up. She wanted my opinion on whether this had anything to do with the vaccine. My response was straightforward and honest. The short answer was that I, frankly, did not know but was intrigued by the timing. However, my most educated guess was that the cause of this inflammation to her optic nerves had likely been brewing since before the vaccine existed. I look forward to hearing stories you may have regarding COVID-19 and patients’ eyes. Drop us an email or find us on social media.

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.