How to address face mask–associated dry eye
Face coverings are causing individuals to experience ocular irritation and dryness
THE USE OF FACE MASKS has exponentially increased during the COVID-19 pandemic. Face masks are worn to reduce disease transmission and prevent infection. Because mask use is expected to continue for the foreseeable future, ODs need to be aware of the impact on the ocular surface. A recent study found a corresponding increase in ocular irritation and dry eyes among regular mask users.1
Face mask history
Just over 100 years ago, Doust and Lyon reported the results of a study on the effect of face masks on respiratory tract infections.2 A volunteer was instructed to gargle with a suspension of an opportunistic pathogen, the bacterium Bacillus prodigiosus (now called Serratia marcescens). Agar plates were placed at various distances from 1 to 10 ft from the volunteer, who was instructed to speak in an ordinary conversational tone, a loud tone, or to cough as much as possible. After the volunteer left the room, plates were exposed for 10 minutes, then incubated for 72 hours.
The results demonstrated a “4-ft danger zone about the patient” during normal or loud speech, which lengthened to “a minimum radius of 10 ft” during coughing. This led to the well-recognized concept of social distancing at approximately 6 ft or 2 m. Presently, laser light scattering and high-speed cameras are used to study particulate emissions.3-5
Early face masks were made of coarse or medium gauze from 2 to 10 layers that did not prevent the projection of inhaled material during coughing. Conversely, “3-layer butter cloth masks were effective” preventing respiratory diseases. This was the genesis of the use of face masks to prevent infective droplet transmission at the time of the Spanish flu pandemic.1
In October 1919, Hurley suggested that if everyone were required to wear a face mask during an influenza epidemic, “the transmission of the infection from those in the incubation period, sick, convalescent, or from well carriers to the healthy noninfected population would be greatly minimized.” This was the first recommendation for both the universal use of face masks and face masks for well, or asymptomatic, carriers.6
N95
Current N95 “respirator” masks have been made to effectively block particle inhalation via a complex microstructure. These masks are termed 95 because they block 95% of the entry of 0.3-μm particles. Thus, 5% of particles are not trapped, which could lead to infection.
A solution is wearing a surgical mask over an N95 mask to prevent infection and keep the surface of the N95 mask clean. However, this may encumber breathing.
Another solution is wearing an N100 respirator mask to block 100% of inhaled particles (virus, bacterial droplet, aerosol). N100 respirators are manufactured by the 3M Company and are designed to block 99.97% of particulate inhalation.7 These masks are beneficial to reduce particle transmission from approximately 5% (N95) to approximately 0.03% (N100), an improvement of approximately 170x to block particle transmission via the nose and mouth.1 These numbers are significantly improved compared to a surgical mask with variable particle penetration of approximately 30% on average.8
N100 respirator masks are not generally discussed because they are even more difficult to obtain than N95 masks, which remain in short supply.1 The downside to N95 or N100 respirator masks is that breathing through them is more difficult compared with breathing through a surgical face mask, necessitating a medical fitting and evaluation prior to use. A valved respirator is not as effective blocking exhaled viral or bacterial infectious droplets because they can pass straight through the valve. Of interest, valved respirators have been prohibited as acceptable “face coverings” for the public in San Francisco, California.9
Mask wear and dry eye
A recent review in Ophthalmology Therapy described a marked increase in dry eye symptoms among regular mask users.10 Dry eye symptoms may become problematic for a significant percentage of the population. Even individuals who have not previously had dry eyes are exhibiting dry eye symptoms with mask usage. Those who wear masks regularly for extended hours each day or full time exhibit more symptoms.10
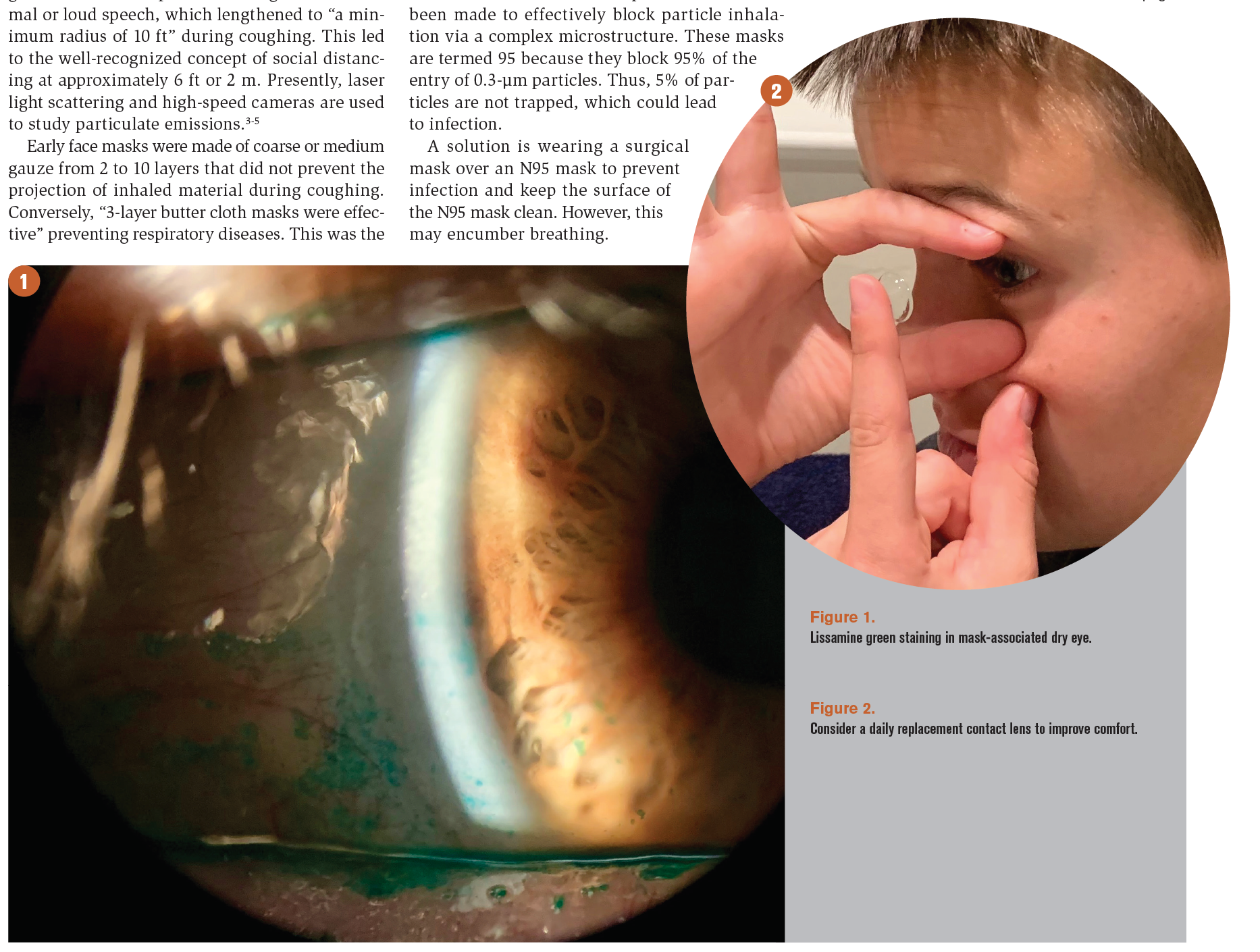
All face mask wearers are susceptible to dry eye symptoms; however, people at greater risk of dry eye symptoms are those who are immunosuppressed, have other preexisting ocular surface conditions such as Sjögren’s syndrome, are elderly with reduced tear film quality, contact lens wearers, and those who wear masks for extended periods. A worsening of subjective dry eye symptoms assessed by the Ocular Surface Disease Index was noted in staff and patients. An objective increase in corneal staining was found in patients who wore face masks (Figure 1).10
Most individuals described an awareness of air blowing upward from the mask into their eyes. Exhaled air from breathing out is channeled up, out of the top of the face mask, and over the ocular surface. The increased airflow likely accelerates tear film evaporation, causing ocular surface irritation or inflammation. Dry eye symptoms include a feeling of dryness; eyes feeling gritty, sandy, irritated, itchy, or watery; or redness.10
The tear film is an essential barrier against the invasion of pathogens and may be compromised if face mask use causes increased evaporation of this barrier.11 Discomfort from dry eyes may increase eye rubbing or touching, which may cause increased viral transmission when unwashed hands are brought close to the face.12 This increases the likelihood of coronavirus infection through mucous membranes such as the mouth, nose, and to a smaller extent, the eye.
Addressing dry eye
A remedy for mask-associated dry eye is to ensure that the mask fits well with a pliable nose wire to fit the mask shape to prevent air from being directed toward the eyes. The top of the mask can be taped to impede upward airflow. However, careful attention is advised to ensure that lower lid excursion is not inhibited and that a mechanical ectropion is not induced. Frequent breaks on digital devices and employing the 20-20-20 rule (every 20 minutes, look at something 20 ft away for 20 seconds) may be beneficial. Taking breaks every few hours for mask removal and the application of lubricant eye drops is helpful. Encouraging good eyelid hygiene to maintain tear film integrity is imperative.
The application of localized heat to the meibomian glands improves meibum secretion, making warm compresses a commonly prescribed treatment.13-15 A recent publication demonstrated that moist heat compress could be an effective first-line treatment to improve comfort in contact lens wearers with contact lens-related dry eye.16 It is also important to limit direct air on the eyes such as with overhead fans and limit time in air-conditioned environments.
If parameters allow, consider prescribing a daily replacement contact lens to improve contact lens comfort,17 prevent contact lens discontinuation,18 and reduce corneal infiltrate events (CIEs; Figure 2). Chalmers reported that reusable contact lens wearers had a 12.5x increased risk of CIEs compared with daily disposable wearers.19
Such consideration is particularly important during the current pandemic, when there may be gaps between eye examinations.
Blinking is key to maintain a normal ocular surface. Most blinks have a cycle of secretion, dispersal, evaporation, and tear drainage.20 A reduced blink rate with computer use has been reported in multiple studies and may be associated with dry eye disease.21-23 One study described that a blink rate of 18.4 blinks/minute prior to computer use was reduced to 3.6 blinks/minute during computer use.21 Recommending and performing blinking exercises may be useful, especially with face mask wear.
Conclusion
During the current pandemic and beyond, it is important to ask patients about their face mask–wearing experiences and inquire about dry eye symptoms with mask wearing. Encourage breaks on digital devices, lubricant eyedrop use, good eyelid hygiene, and avoidance of touching the face and eyes (Figure 3).
References
1. Oldfield E, Malwal SR. COVID-19 and other pandemics: how might they be prevented? ACS Infect Dis. 2020;6(7):1563-1566. doi:10.1021/acsinfecdis.0c00291
2. Doust BC, Lyon AB. Face masks in infections of the respiratory tract. JAMA. 1918;71(15):1216-1219. doi:10.1001/ jama.1918.26020410011008c
3. Anfinrud P, Stadnytskyi V, Bax CE, Bax A. Visualizing speech-generated oral fluid droplets with laser light scattering. N Engl J Med. 2020;382(21):2061-2063. doi:10.1056/NEJMc2007800
4. Tang JW, Settles GS. Images in clinical medicine. Coughing and aerosols. N Engl J Med. 2008;359(15):e19. doi:10.1056/ NEJMicm072576
5. Bourouiba L, Dehandschoewercker E, Bush JWM. Violent expiratory events: on coughing and sneezing. J Fluid Mech. 2014;745:537-563. doi:10.1017/jfm.2014.88
6. Hurley JR. Influenza with special reference to the pandemic of 1918. Medical Record. 1919;96(16): 651-664.
7. 3M Particulate Respirator 8233, N100. 3M. Accessed May 5, 2021. https://www.3m.com/3M/en_US/p/d/v000057486/
8. Balazy A, Toivola M, Adhikari A, Sivasubramani SK, Reponen T, Grinshpun SA. Do N95 respirators provide 95% protection level against airborne viruses, and how adequate are surgical masks? Am J Infect Control. 2006;34(2):51-57. doi:10.1016/j. ajic.2005.08.018
9. Masks and face coverings for the coronavirus pandemic. City and County of San Francisco. Updated May 8, 2021. Accessed May 5, 2021. https://sf.gov/information/masks-and-face-coverings-coronavirus-pandemic
10. Moshirfar M, West WB Jr, Marx DP. Face mask-associated ocular irritation and dryness. Ophthalmol Ther. 2020;9(3):397- 400. doi:10.1007/s40123-020-00282-6
11. Sun CB, Wang YY, Liu GH, Liu Z. Role of the eye in transmitting human coronavirus: what we know and what we do not know. Front Public Health. 2020;8:155. doi:10.3389/ fpubh.202000155
12. Lazzarino AI, Steptoe A, Hamer M, Michie S. Covid-19: important potential side effects of wearing face masks that we should bear in mind. BMJ. 2020;369:m2003. doi:10.1136/bmj. m2003
13. Geerling G, Tauber J, Baudouin C, et al. The international workshop on meibomian gland dysfunction: report of the subcommittee on management and treatment of meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2011;52(4):2050- 2064. doi:10.1167/iovs.10-6997g
14. Goto E, Endo K, Suzuki A, Fujikura Y, Tsubota K. Improvement of tear stability following warm compression in patients with meibomian gland dysfunction. Adv Exp Med Biol. 2002;506(Pt B):1149-1152. doi:10.1007/978-1-4615-0717-8_161
15. Olson MC, Korb DR, Greiner JV. Increase in tear film lipid layer thickness following treatment with warm compresses in patients with meibomian gland dysfunction. Eye Contact Lens. 2003;29(2):96-99. doi:10.1097/01.ICL.0000060998.20142.8D
16. Tichenor AA, Cox SM, Ziemanski JF, et al. Effect of the Bruder moist heat eye compress on contact lens discomfort in contact lens wearers: an open-label randomized clinical trial. Cont Lens Anterior Eye. 2019;42(6):625-632. doi:10.1016/j. clae.2019.09.005
17. McConville P, Pope JM. Diffusion limited evaporation rates in hydrogel contact lenses. CLAO J. 2001;27(4):186-191.
18. Nichols JJ, Willcox MDP, Bron AJ, et al; members of the TFOS International Workshop on Contact Lens Discomfort. The TFOS International Workshop on Contact Lens Discomfort: executive summary. Invest Ophthalmol Vis Sci. 2013;54(11):TFOS7– TFOS13. doi:10.1167/iovs.13-13212
19. Chalmers RL, Keay L, McNally J, Kern J. Multicenter case-control study of the role of lens materials and care products on the development of corneal infiltrates. Optom Vis Sci. 2012;89(3):316-325. doi:10.1097/OPX.0b013e318240c7ff
20. Himebaugh NL, Begley CG, Bradley A, Wilkinson JA. Blinking and tear break-up during four visual tasks. Optom Vis Sci. 2009;86(2):E106-E114. doi:10.1097/ OPX.0b013e318194e962
21. Patel S, Henderson R, Bradley L, Galloway B, Hunter L. Effect of visual display unit use on blink rate and tear stability. Optom Vis Sci. 1991;68(11):888-892. doi:10.1097/00006324-199111000-00010
22. Freudenthaler N, Neuf H, Kadner G, Schlote T. Characteristics of spontaneous eyeblink activity during video display terminal use in healthy volunteers. Graefes Arch Clin Exp Ophthalmol. 2003;241(11):914-20. doi:10.1007/s00417- 003-0786-6
23. Tsubota K, Nakamori K. Dry eyes and video display terminals. N Engl J Med. 1993;328(8):584. doi:10.1056/ NEJM199302253280817
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.