IOP-lowering medication review
Stay up-to-date on available glaucoma therapies

Medical therapy for the treatment of glaucoma has come a long way in recent decades, yielding several classes of medications and combinations from which to choose. This will serve as a review of available topical medications in the United States for the treatment of glaucoma. It will also update the clinician on the newer therapeutics that have recently become available.
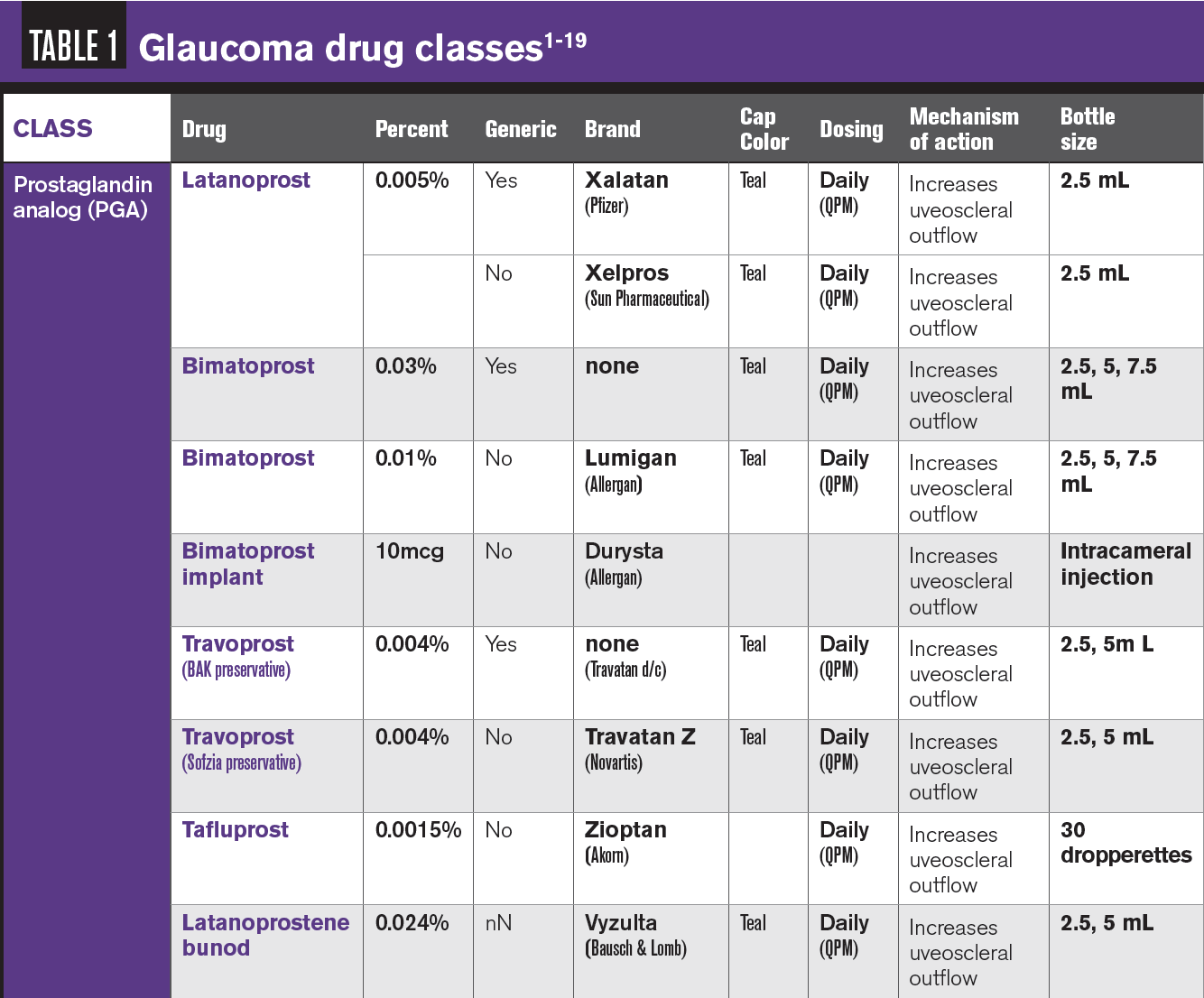
Prostaglandin analogues
Example: Latanoprost (Xalatan; Pfizer)
Prostaglandin analogues (PGAs) are the primary first-line intraocular pressure (IOP)-lowering drug class due to their 25-year history of excellent efficacy, safety, and tolerability. They increase aqueous outflow through the uveoscleral pathway by increasing extracellular matrix turnover in the ciliary body.1 A 25% to 35% decrease in IOP is seen with PGA use, and the maximum effect takes up to 2 weeks to be reached. PGAs are dosed once a day (usually at bedtime, but adherence is more important than time of day used) and show a paradoxical increase in IOP when dosed more than that.2,3
This medication type should be used with caution in patients with ocular inflammatory conditions (ie, uveitis, herpes, macular edema) and in pregnant patients.1,4,5 No significant systemic adverse events (AEs) exist. Main local AEs of PGAs include stinging, hyperemia, darkening of the iris (affecting green-brown eyes the most), eyelid redness, and increased length, thickness, pigmentation, and number of eyelashes and eyelid vellus hairs. All AEs are reversible with discontinuation except iris color changes.1,3,5 An interesting AE of long-term use is prostaglandin-associated periorbitopathy and includes the following changes6:
– Upper lid ptosis
– Deepening of the upper lid sulcus
– Shrinkage of dermatochalasis
– Periorbital fat atrophy
– Mild enophthalmos
– Inferior scleral show
– Increased prominence of eyelid vessels
– Tightening of the eyelids
Upon discontinuation, partial to full reversal of these changes is seen.6
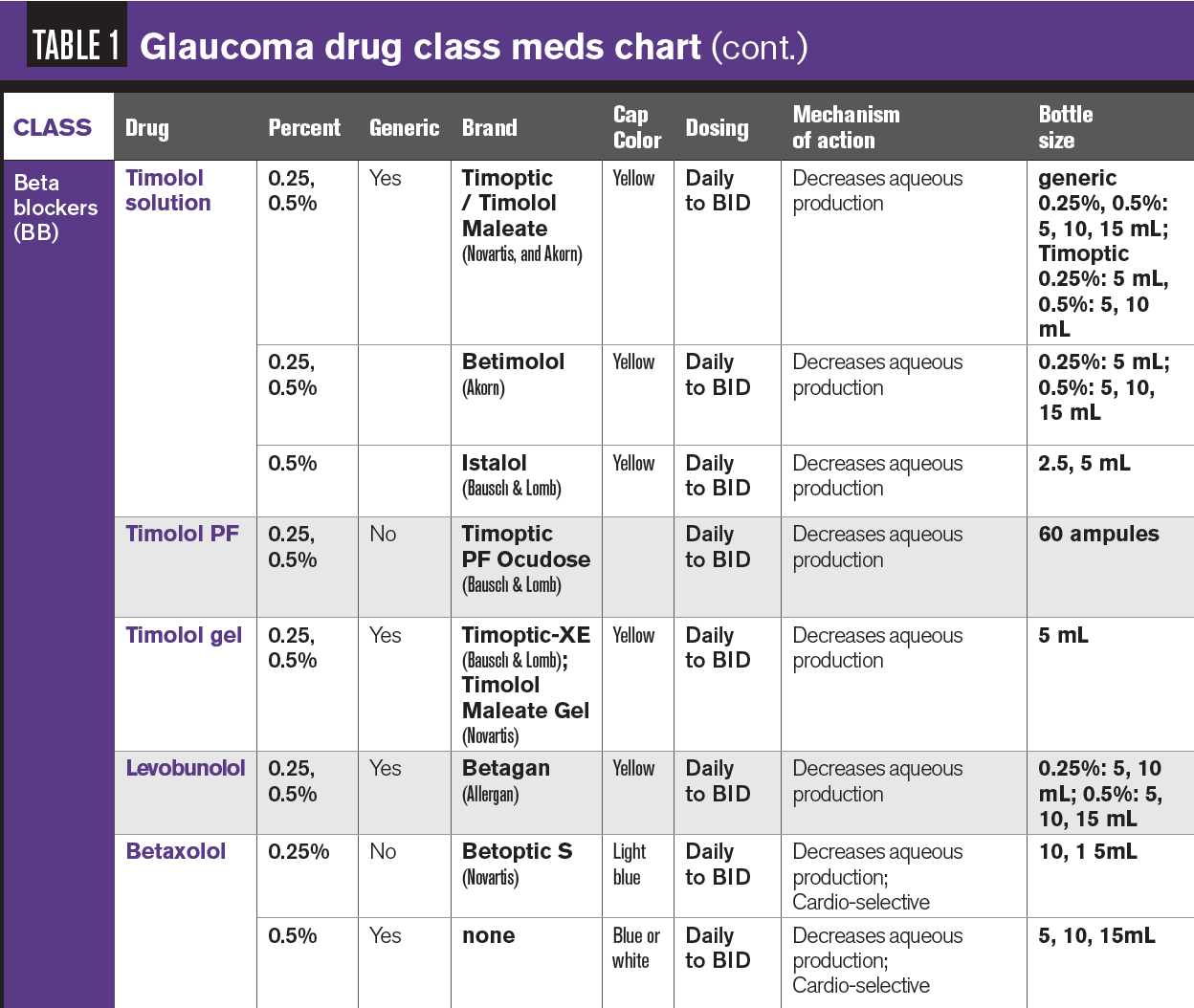
Beta blockers (beta adrenergic antagonists)
Example: Timolol (Timoptic)
Beta blocker (BB) eye drops work by blocking the beta receptors in the ciliary body, reducing aqueous production.7 Nocturnal aqueous production is about half of diurnal, which is why BBs do not control overnight IOP as well as other options.4,5 Expected IOP decrease with a topical BB is 20% to 30%, but efficacy may decrease over time in approximately 10% of patients. BBs are dosed once or twice a day: often twice a day if monotherapy, every morning if using the gel formulation or when used as adjunctive therapy.2,5 Patients already on a systemic BB will not achieve the maximum effect of the topical BB since the systemic beta blocker slightly lowers the baseline IOP by about 2 mm Hg.2
Beta blockers are indicated for all types of glaucoma—the state of the angle does not impact their effect).5 The most common AEs from topical BB are shortness of breath, reduced blood pressure and heart rate, and fatigue. Less common AEs include decreased libido, depression, and decreased sensitivity to symptoms of hypoglycemia in insulin-dependent diabetics.7,8
These drops are contraindicated in patients with asthma, severe chronic obstructive pulmonary disease, sinus bradycardia, heart/atrioventricular block, congestive heart failure, and myasthenia gravis.2,7 Consider taking a pretreatment pulse on patients being prescribed a topical BB and reevaluate pulse at follow-up visits.5
Most BB nonselectively block both beta-1 (cardio) and beta-2 (lung) receptors. Betaxolol (Betoptic-S; Alcon) is the only selective topical BB because it has an affinity for beta-1 receptors. Because of this, it is an option for patients without cardiovascular risk factors but with significant pulmonary risk factors to safely use a topical BB. Unfortunately, more beta-2 receptors exist in the eyes, so this drop does not have as significant an effect on IOP as nonselective BB.2,5
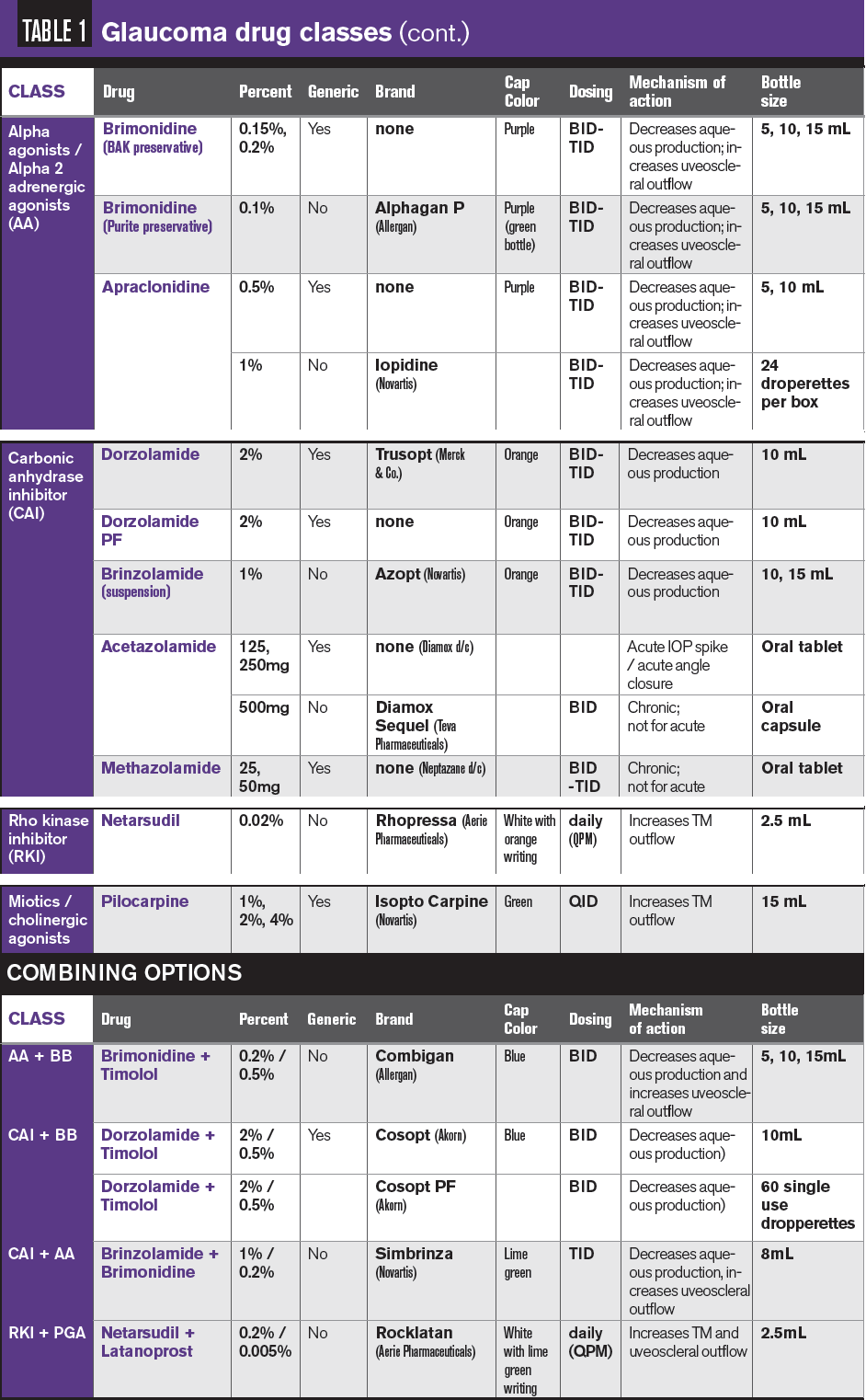
Alpha agonists (selective alpha-2 adrenergic receptor agonist)
Example: Brimonidine (Alphagan)
Alpha agonists activate the alpha-2 receptors in the ciliary body, inhibiting aqueous secretion.7 The main short-term effect is reduced aqueous production, and chronic treatment leads to increased aqueous outflow through the uveoscleral pathway.9 The reduction in IOP is 4 mm Hg to 6 mm Hg with this class.10
Up to 20% of users experience an allergy to this medication, which can appear soon after initiating treatment or be delayed up to 8 months and is concentration and dose dependent. Other than an allergy to the medication or preservative, other common AEs include irritation; burning; headache; dry mouth, nose, and eyes; hypotension and lethargy, fatigue, and drowsiness.2,9 This medication is contraindicated in children under age 2 years and in patients taking a monoamine oxidase inhibitor.4,7
Carbonic anhydrase inhibitors (CAI)
Example: Dorzolamide (Trusopt; Merck)
Inhibiting the carbonic anhydrase (CA) enzyme reduces aqueous production in the ciliary body, decreasing IOP by 4 mm Hg to 6 mm Hg with this class.7,10 AEs include a bitter taste, instillation discomfort, diuresis, fatigue, and stomach upset.7,8 This class is contraindicated in patients with a sulfa allergy, severe liver or kidney disease, or corneal compromise because the CA enzyme is present in the corneal endothelium and is involved in fluid transport within the cornea.7,11
The oral CAIs—acetazolamide, Diamox Sequels (acetazolamide XR; Teva Pharmaceuticals), and methazolamide—can be an option for chronic glaucoma treatment, especially to lower IOP while awaiting surgery or for a patient on maximum topical treatment not at target IOP who is not a candidate for surgery. Acetazolamide, however, is usually used in the treatment of short-term IOP control in acute angle closure glaucoma. Because of its reduced strength, methazolamide has fewer AEs but is not as effective as acetazolamide.
Oral CAIs have the same contraindications as topical CAIs, with additional contraindication if the patient is taking a thiazide diuretic or digitalis. Oral CAIs have a longer list of AEs because of systemic administration, including tingling hands and feet, memory problems, increased urination, kidney and liver effects, gastrointestinal problems, depression, impotence, Stevens-Johnson syndrome, and aplastic anemia.7,8,12
Miotics/cholinergic agonists
Example: Pilocarpine (Isopto Carpine; Alcon)
This rarely used class stimulates the muscarinic receptors, causing pupillary muscle constriction, which pulls on and opens the trabecular meshwork (TM) leading to increased aqueous outflow through the TM. Many ocular AEs are related to the pupillary constriction of this therapy, including dim vision, brow ache, myopia, and retinal tear and detachment.7,13
This medication is dosed 4 times a day, giving approximately a 20% decrease of IOP at that dosing. It is reserved for acute angle closure and should be used with caution in patients who are pregnant or breastfeeding.2,14
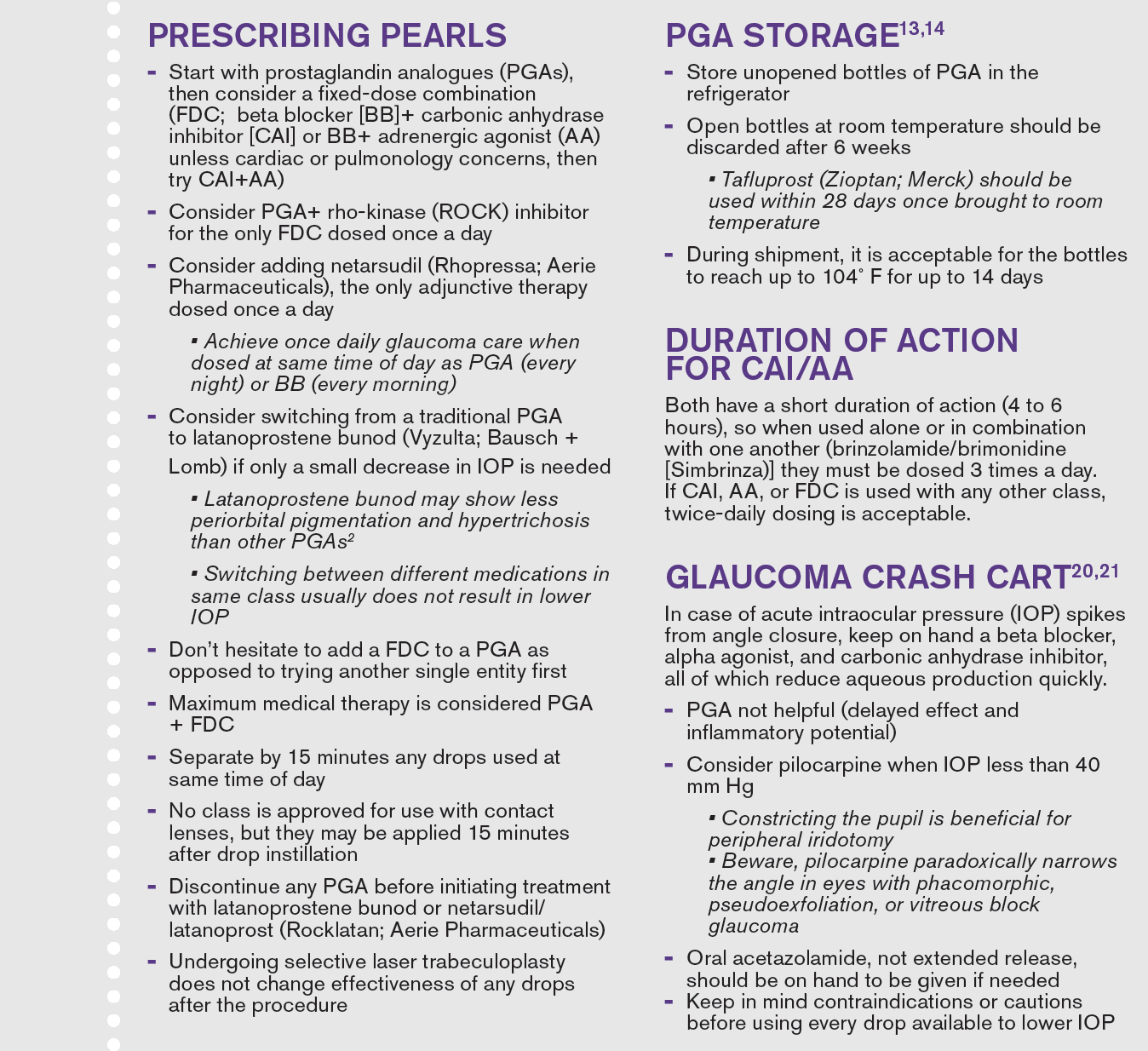
New options
Latanoprostene bunod (Vyzulta; Bausch + Lomb) is 1 of the 2 newest options and is part of the PGA class. The drug is metabolized into 2 active moieties; latanoprost acid, which increases uveoscleral outflow, and nitric oxide, which causes the TM to relax, leading to increased TM outflow. Research shows an additional IOP drop of about 1 mm Hg to 1.23 mm Hg compared to latanoprost.2,15
Another new glaucoma drug is netarsudil (Rhopressa; Aerie Pharmaceuticals), the first drug in the new class rho-kinase (ROCK) inhibitors. ROCK inhibition decreases TM cell contraction, leading to expansion and relaxation of the TM, causing increased aqueous outflow through the TM. Additionally, episcleral venous pressure decreases, which also increases outflow through the TM. ROCK inhibition also inhibits norepinephrine transport, leading to decreased blood flow to the ciliary body, which decreases aqueous production.
This medication is used only as adjunctive therapy and shows approximately 20% additional decrease in IOP when added to a PGA or combination drop. Local AEs include hyperemia (42%), stinging, corneal verticillate (11%), and subconjunctival hemorrhages (11%).2,8,16
Fixed-dose combination (FDC) drops
These are great options for increasing convenience and adherence, reducing the amount of preservative on the eye, and reducing cost.10 Most are dosed twice a day.2 Brinzolamide/brimonidine (Simbrinza; Novartis) is dosed 3 times a day. The newest combination, netarsudil/latanoprost (Rocklatan; Aerie Pharmaceuticals), is dosed once a day, typically at bedtime.17
Marijuana (tetrahydrocannabinol)
Finally, a few thoughts on a drug many patients assume is a treatment for glaucoma. Smoking marijuana has been shown to decrease IOP in individuals with or without glaucoma; however, the duration of action is short, only about 3 to 4 hours.
For this therapy to be an effective option, patients would need to smoke about every 3 hours, around the clock. Not only is this unrealistic, but the mood-altering effect would cause the user to be unable to drive or function at maximum mental capacity.
Additionally, hundreds of lung-damaging compounds in marijuana. Other routes (ie, oral, sublingual, drop) have been unsuccessful due to AEs or ineffective IOP control.18
Future research opportunities exist because receptors for the active component of marijuana are found in eye tissues, and this drug may even have neuroprotective potential. At this time, no form of this drug is recommended as an option for IOP-lowering therapy.18
References
1. Brooks AM, Gillies WER. Ocular beta-blockers in glaucoma management. Clinical pharmacological aspects. Drugs Aging. 1992;2(3):208-21. doi:10.2165/00002512-199202030-00005
2. Dorkowski M, Williamson J, Rixon A. A guide to applying IOP-lowering drugs. Review of Optometry. July 15, 2018. Accessed May 10, 2021. https://www. reviewofoptometry.com/article/a-guide-to-applying-ioplowering-drugs
3. Medication review: prostaglandin analogs for glaucoma. Pharmacy Times®. October 1, 2015. Accessed May 10, 2021. https://www.pharmacytimes. com/contributor/michelle-smith-pharmd-bcps/2015/10/medication-review-prostaglandin-analogs-for-glaucoma
4. Yee S. Glaucoma therapy: finding the right combination. Review of Optometry. April 15, 2027. Accessed May 10, 2021. https://www.reviewofoptometry.com/ article/glaucoma-therapy-finding-the-right-combination
5. Dexter A. Review of topical glaucoma medications. OptoPrep. February 29, 2016. Accessed May 10, 2021. https://blog.optoprep.com/review-of-topical-glaucoma-medications-prostaglandins-and-beta-blockers
6. Jayaram A. Prostaglandin associated periorbitopathy. American Academy of Ophthalmology. Updated April 26, 2021. Accessed May 10, 2021. https:// eyewiki.org/Prostaglandin_Associated_Periorbitopathy
7. Rhee DJ. Glaucoma: Color Atlas & Synopsis of Clinical Ophthalmology. McGraw-Hill, Medical Pub. Division. 2003:107-117.
8. Radhakrishnan S, Iwach A. Glaucoma medications and their side effects. Glaucoma Research Foundation. Updated July 23, 2018. Accessed May 10, 2021. https://www.glaucoma.org/gleams/glaucoma-medications-and-their-side-effects.php
9. Cantor LB. Brimonidine in the treatment of glaucoma and ocular hypertension. Ther Clin Risk Manag. 2006;2(4): 337-346. doi:10.2147/tcrm.2006.2.4.337
10. Collins LA, King BJ. Boost your glaucoma drug knowledge. Modern Optometry. April 2019. Accessed May 10, 2021. https://modernod.com/ articles/2019-apr/boost-your-glaucoma-drug-knowledge?c4src=article:infinite-scroll
11. Reynolds AC. Topical glaucoma treatment and the cornea. Glaucoma Today. November/December 2014. Accessed May 10, 2021. https://glaucomatoday. com/articles/2014-nov-dec/topical-glaucoma-treatment-and-the-cornea
12. Perkins TW. Oral CAIs: still an option worth using. Review of Ophthalmology. April 12, 2006. May 10, 2021. https://www.reviewofophthalmology.com/article/ oral-cais-still-an-option-worth-using
13. Medication guide. Glaucoma Research Foundation. Updated June 19, 2020. Accessed May 10, 2021. https://www.glaucoma.org/treatment/medication-guide.php
14. Epocrates. Version 21.1.1. Last updated February 5, 2021.
15 . Vyzulta. Package insert. Bausch + Lomb; Revised May 2019. Accessed May 24, 2021. https://www.bausch.com/Portals/69/-/m/BL/United%20States/USFiles/Package%20Inserts/Pharma/vyzulta-prescribing-information.pdf
16. Rhopressa. Package insert. Aerie Pharmaceuticals; Revised March 2019. Accessed May 24, 2021. https://rhopressa.com/hcp/assets/ pdf/RHOPRESSA-Prescribing-Information.pdf
17. Rocklatan. Package insert. Aerie Pharmaceuticals; Revised June 2020. Accessed May 24, 2021. https://rocklatan.com/hcp/assets/ pdf/Rocklatan_Prescribing_Information.pdf
18. Jampel H. American Glaucoma Society position statement: marijuana and the treatment of glaucoma. J Glaucoma. 2010;19(2):75-76. doi:10.1097/IJG.0b013e3181d12e39
19. Glaucoma Medication Manufacturers. Glaucoma Research Foundation. Updated June 24, 2020. Accessed May 10, 2021. www. glaucoma.org/treatment/glaucoma-medications-manufacturers.php
20. Cymbor M. Angle closure glaucoma: are you ready? Review of Optometry. October 15, 2016. Accessed May 10, 2021. https://www. reviewofoptometry.com/article/angleclosure-glaucoma-are-you-ready
21. Khondkaryan A, Francis BA. Angle closure glaucoma. American Academy of Ophthalmology. December 18, 2013. Accessed May 10, 2021. https://www.aao.org/current-insight/angleclosure-glaucoma-19
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.