Introduction to biosimilars for AMD
Advances in drug creation would reduce cost burden of treatment for patients.

As a low-vision specialist, I see hundreds of patients with age-related macular degeneration (AMD) each year. Patients with advanced AMD frequently experience the greatest difficulty with daily activities and have the most limited ability to interact with loved ones. As a result of its increasing prevalence, it is the most common diagnosis seen in low-vision clinics.
AMD is one of the leading causes of visual impairment in the US, with nearly 20 million individuals with early-stage AMD and 1.5 million individuals with late-stage AMD.1 Not only is the prevalence high, but the cost of treatment is also very high.
The main treatment drugs for exudative age-related macular degeneration are Eylea, Lucentis, and Avastin alongside some novel drugs such as Vabysmo and Beovu. While the exact price may differ for each case, the high price tag is irrefutable. Eylea and Lucentis cost about $1800 per dose whereas Vabysmo costs $2,190 per treatment.2,3
According to Genentech, patients can be treated with Vabysmo every 1 to 4 months, following 4 initial monthly doses based on evaluation of the patient’s anatomy and vision outcomes. Thus, the overall cost of treatment is expected to go down after the first year given the ability for less frequent dosing over time, as shown by recent 2-year data from two large-scale clinical trials. In these studies, nearly 80% of people receiving Vabysmo for wet AMD could be treated every 3 months or longer, while more than 60% could be treated every four months.
Considering the vast population of Americans who receive a diagnosis of visually impairing stages of AMD, it comes as no surprise that the market for treatment options is lucrative and vast. By 2030, it is predicted that the global market for age-related macular degeneration treatments will be around $18 billion.
It is anticipated that between 2022 and 2030, growth will increase at a 6.9% compound annual rate.4 This rate of growth is largely attributable to increased life span; many patients receive injections for well over a decade. The tremendous amount of research and development (R&D) funds dedicated to launching new pharmaceuticals for treatment also contributes to the cost.
A biosimilar drug is a medication that, both structurally and functionally, is remarkably similar, but not identical, to its innovator biologic (also known as the reference medicine). A biosimilar drug functions similarly to its original biologic, displaying no substantial differences between them. To prove equal status, the biosimilar must demonstrate comparable safety, efficacy, and pharmacokinetics. This indicates that the biosimilar is regarded as being as secure and efficient as the biologic.5
Drug manufacturers around the world are vying to get their foot in the market as fast as possible. Pharmaceutical companies are driven by lower costs of development, yielding higher profitability margins. A biosimilar can be created more quickly for substantially less money compared with an original biologic.
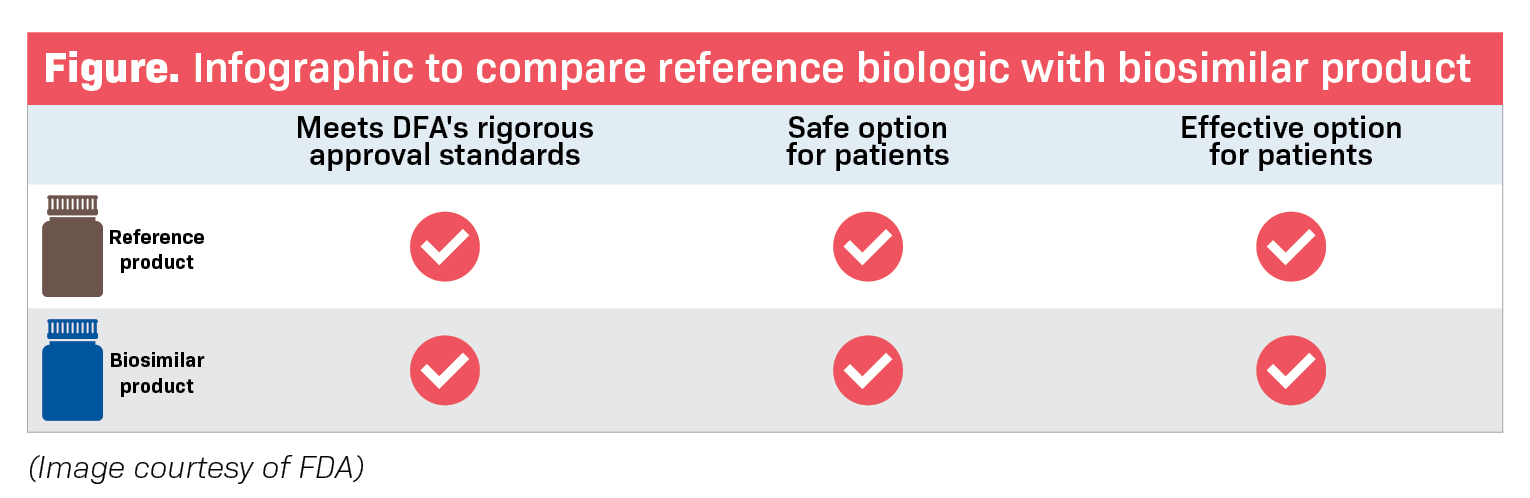
Biologics production can typically take 10 to 15 years on average and cost well over $2 billion USD. Biosimilars, however, can be created in 8 to 10 years for roughly a tenth of the cost around $100 million to $200 million.6,7 Biosimilars can cut costs and time because the requirements for FDA approval rely more heavily on strong bioequivalence than extensive clinical trials that biologics are required to participate in.
Between 2014 and 2024, it is predicted that biosimilars in the US will result in nearly a $44 billion reduction on biological drug spending. Though it is impossible to forecast the precise cost of ophthalmological medications, in general, biosimilars result in a 10% to 50% decrease in price per unit compared with the market price for original biologics.6
It is key to understand the difference between biosimilars and generic products. Generic pharmaceuticals are identical to the branded drugs on which they are based in that they have the same active ingredients and chemical compositions.
Generic medications are also created through far less complicated pharmacologic chemical processes, whereas biosimilar medicines must be reverse-engineered using much more complex systems and are not entirely comparable to the original biologic. They are structurally comparable but different from the original biologics, yet there are no clinically significant differences in their safety or effectiveness.6
The ophthalmology field for biosimilars is rapidly growing as major pharmaceutical companies are losing their patents. Lucentis and Eylea are both subject to losing their US and European patent between 2021 and 2025.6 As a result, the race to produce biosimilars has ensued. A 2020 study identified 25 different ophthalmic biosimilars in various stages of development: 8 for bevacizumab (Avastin), 4 for aflibercept (Eylea), and 6 for ranibizumab (Lucentis).8
There are more than a handful of biosimilars for Lucentis in various stages of R&D globally. Some major ones that are further along the research phases include Razumab (Intas Pharmaceuticals Ltd), FYB 201 (Formycon AG and Bioeq AG), and SB11 (Samsung Biosimilars). Biosimilars for Eylea, FYB203 (Formycon) and ALT-L9 (Alteogen Inc), are further along, and M710 (Momenta Pharmaceuticals and Mylan NV) appears to be promising as well. Avastin is not currently FDA approved for ophthalmic usage and though there are biosimilars on the market, their usage is currently geared toward oncology treatments.8

What does this entail for optometrists? Optometrists frequently make the initial diagnosis of patients with early AMD. As we track the course of the disease, we can provide patients with a stronger assurance that they will have options that may be more affordable and even more effective in preserving their vision. At our low-vision clinic, patients frequently inquire about the future of AMD treatment. As more biosimilars receive FDA approval, we are hoping we will be able to provide our patients with a bigger array of better options.
Conclusion
It is imperative for optometrists to be knowledgeable and up to date with novel therapies and current research. Biosimilars will create an abundance of alternatives for treating not only age-related macular degeneration but also other ocular conditions. Topical eye drops can be very costly for patients with conditions such as glaucoma or ocular surface disease. With great anticipation, the future holds a place for biosimilars in the realm of many more ocular diseases.
Editor's note: This story has been updated to reflect the correct price of Vabysmo from "more than $2300" to "$2,190 per treatment." Dosing frequency information provided by Genentech was also added. This information was incorrect in print.
References
1. Rein DB, Wittenborn JS, Burke-Conte Z, et al. Prevalence of age-related macular degeneration in the US in 2019. JAMA Ophthalmol. 2022;140(12):1202-1208. doi:10.1001/jamaophthalmol.2022.4401
2. Eylea prices, coupons, copay and patient assistance. Drugs.com. Updated January 11, 2023. Accessed December 20, 2022. https://www.drugs.com/price-guide/eylea
3. Vabysmo prices, coupons, copay and patient assistance programs. Drugs.com. Updated January 11, 2023. Accessed December 20, 2022. https://www.drugs.com/price-guide/vabysmo
4. Mulcahy AW, Predmore Z, Mattke S. The cost savings potential of biosimilar drugs in the United States. Rand Corporation. 2014. Accessed December 20, 2022. https://www.rand.org/content/dam/rand/pubs/perspectives/PE100/PE127/RAND_PE127.pdf
5. What are biosimilar drugs? American Cancer Society. Revised April 27, 2022. Accessed December 20, 2022. https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/biosimilar-drugs/what-are-biosimilars.html
6. Sharma A, Reddy P, Kuppermann BD, Bandello F, Lowenstein A. Biosimilars in ophthalmology: “is there a big change on the horizon?” Clin Ophthalmol. 2018;12:2137-2143. doi:10.2147/opth.s180393
7. Taylor R. Biosimilars in ophthalmology. American Academy of Ophthalmology. January 2021. Published January 2021. Accessed December 20, 2022. https://www.aao.org/eyenet/article/biosimilars-in-ophthalmology
8. Sharma A, Kumar N, Kuppermann BD, et al. Understanding biosimilars and its regulatory aspects across the globe: an ophthalmology perspective. Br J Ophthalmol. 2020;104(1):2-7. doi:10.1136/bjophthalmol-2019-314443
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.