Orthokeratology is key to managing pediatric myopia
Enhanced treatments, tools, and resources make a difference.
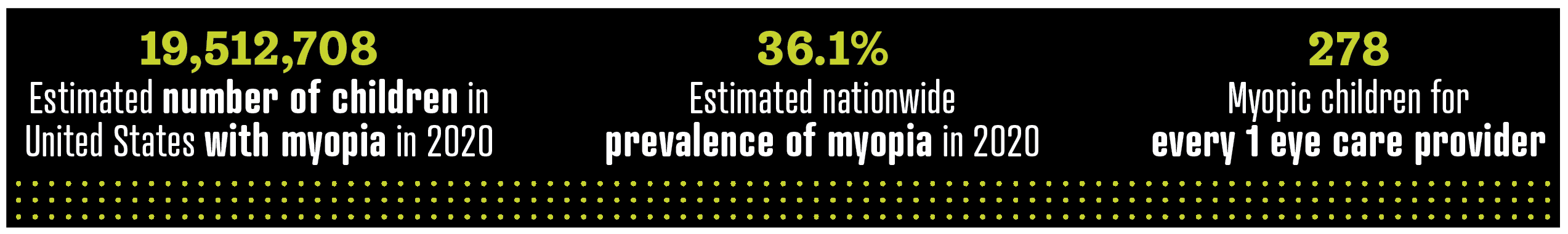
With the global rise of myopia in recent years, there is no shortage of patients in need of management. Estimation of myopia prevalence using the 2020 US Census revealed that 39,025,416 eye examinations are required annually across the nation for each child with myopia to be evaluated twice per year.1
Of the approximately 70,000 optometrists and ophthalmologists nationwide, each eye care professional (ECP) would need to provide care to 278 children biannually to meet the current eye care requirements of children with myopia in the United States.1 That averages to examining and managing more than 1 pediatric myope a day. How does your practice compare?
Benefits beyond management
As ECPs, we aim to reduce the burden of progressive myopia and help prevent long-term visual impairment for all myopes. But what are our patients saying about their own correction modalities and outcomes?
When it comes to orthokeratology (ortho-k), patient feedback is resoundingly about their vision-related quality of life.
A study by Lipson et al using the National Eye Institute Refractive Error Quality of Life questionnaire compared adults wearing single vision, soft contact lenses to adults wearing ortho-k lenses. They concluded that overall satisfaction and vision were comparable; however, about 68% of the participants preferred ortho-k and chose to continue its use at the end of the study.2 Subjects reported they enjoyed daytime correction-free vision.
Although adults may prefer ortho-k, what about pediatric myopes? Zhao et al evaluated pediatric subjects before and after 3 months of ortho-k wear.
Source: Fortin P, Kwan J. The Myopia Management Opportunity in the United States Using the 2020 Census.
Poster presented at: Association for Research in Vision and Ophthalmology 2022 Annual Meeting; May 1-5, 2022; Denver, CO.
Children using ortho-k showed improved quality of life and benefits during daily activities, were more willing to try something new, and were more self-confident, active, and likely to participate in sports—ultimately resulting in an increased total time spent outdoors.3
Perhaps a holistic approach to myopia management may help continue to engage patients and assist in the long-term adherence required to adequately help manage myopia.
Innovations in lens design
Since the first FDA approval for ortho-k contact lenses in the United States in 2002, ortho-k has seen dramatic enhancements in lens designs and materials. Two topics that stand out in clinical practice today are ortho-k lenses with meridional depth differences and the ability to customize back optic zone diameters.
Meridional depth difference
Although meridional ortho-k lens designs tend to be prescribed for myopic patients with astigmatism, their fitting capabilities far exceed myopic and astigmatic correction.
For example, a patient with 0.50 diopters (D) of corneal toricity may be empirically prescribed a single return zone depth difference based on manufacturers’ guidelines.
However, the small amount of toricity on the cornea paired with an ortho-k lens, which incorporates a meridional depth difference, will allow for proper tear exchange underneath the lens and optimal centration. Therefore, several patients could benefit from the stabilization and superior fit provided by this design.
Back optic zone diameters
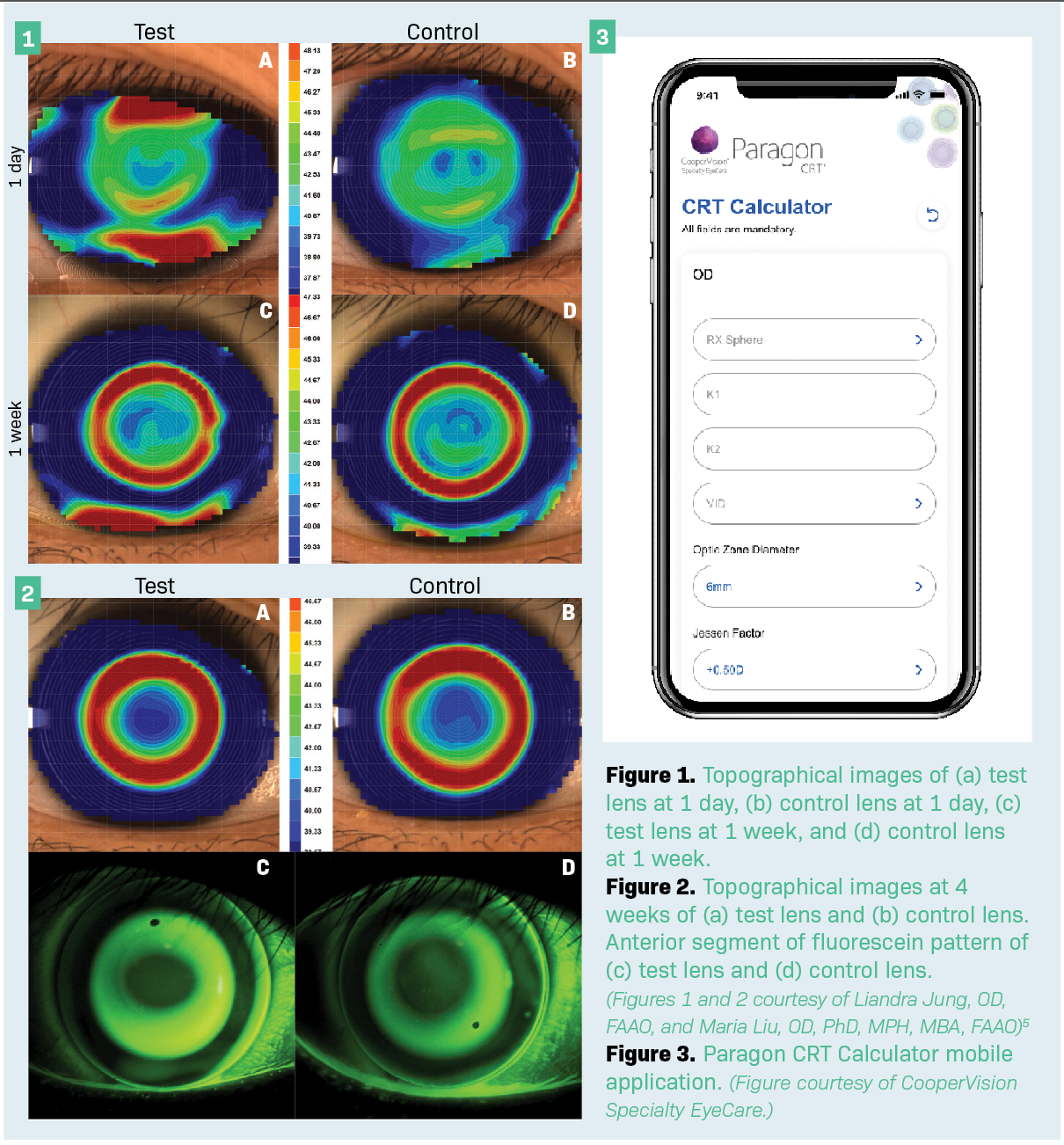
In a recent clinical trial, 5-mm back optic zone diameter (BOZD) ortho-k lenses offered many benefits to patients with myopia. Results showed a 5-mm BOZD had 0.43 D more myopia correction at the 1-day visit compared with the 6-mm BOZD (control lens) design, offering rapid onset of correction and improved visual acuity (Figures 1 and 2).4,5
Jung et al also found a proven, statistically significant reduction in topographic treatment zone diameter with a 5-mm BOZD ortho-k lens design. Thus, for ECPs aiming to achieve a smaller treatment zone size for their patients, a 5-mm BOZD has proven advantageous.
Fitting for the future
Although many ECPs are familiar with fitting contact lens patients diagnostically or empirically, innovative ways are now available to increase accessibility and streamline the fitting process in clinic.
Launched in October 2021, the Paragon CRT Calculator mobile application (Figure 3) enables ECPs to determine Paragon CRT and CRT Dual Axis (CooperVision Specialty Eye Care) ortho-k lens patient parameters and place lens orders with a few clicks. A quickaccess troubleshooting guide offers a useful clinical tool on the go.
In 2022, myopia prevalence is undoubtedly increasing. However, the eye care profession is armed with enhanced management options and the tools and resources to help make a difference in the lives of pediatric patients with myopia.
References
1. Fortin P, Kwan J. The myopia management opportunity in the United States using the 2020 Census. Poster presented at: Association for Research in Vision and Ophthalmology 2022 Annual Meeting; May 1-5 2022; Denver, CO.
2. Lipson MJ, Sugar A, Musch DC. Overnight corneal reshaping versus soft disposable contact lenses: vision-related quality-of-life differences from a randomized clinical trial. Optom Vis Sci. 2005;82(10):886-891. doi:10.1097/01.opx.0000180818.40127.dc
3. Lipson MJ, Boland B, McAlinden C. Vision-related quality of life with myopia management: a review. Cont Lens Anterior Eye. 2022;45(3):101538. doi:10.1016/j.clae.2021.101538
4. Zhao F, Zhao G, Zhao Z. Investigation of the effect of orthokeratology lenses on quality of life and behaviors of children. Eye Contact Lens. 2018;44(5):335-338. doi:10.1097/ICL.0000000000000529
5. Jung L, Liu M. Comparing 5mm and 6mm back optic zone diameter (BOZD) in orthokeratology lens design. Poster presented at: Global Specialty Lens Symposium 2022; January 19-22, 2022; Las Vegas, NV.

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.