Peroxide lens care effective for GP lens wearers
With their outstanding disinfection efficacy, preservative-free composition, and features supporting lens care compliance, H2O2 lens care systems can be an excellent option for GP lens wearers. Find out more about why
Figure 1. A scleral contact lens (with NaFl) on an eye with a corneal graft. Photo courtesy Clark Y. Chang, MSA, MSc, OD, FAAO


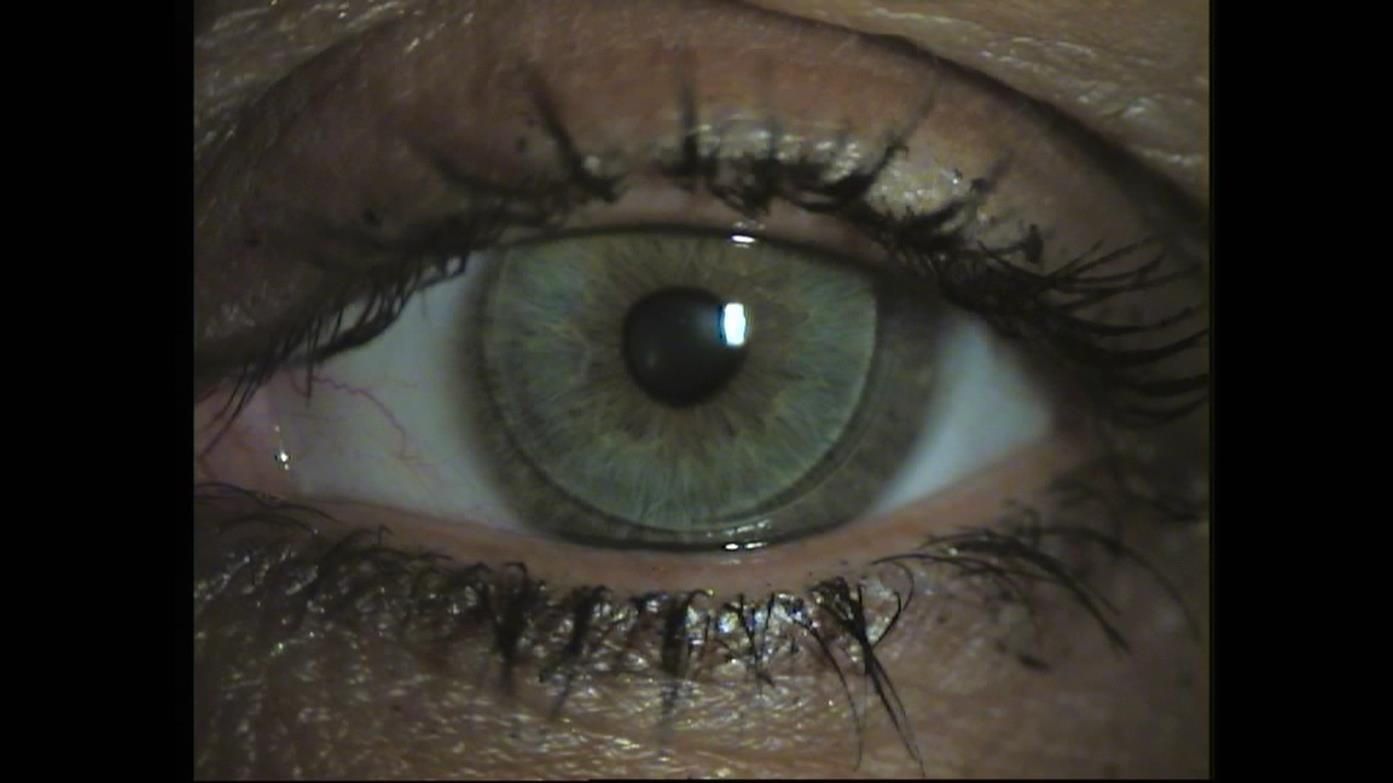
Figure 2. A healthy cornea fitted with an aspheric gas permeable contact lens. Photo courtesy Ardie van Goinga and Karin Teuben, Lens B.V.
Rigid gas permeable (GP) contact lenses continue to serve as essential optical and therapeutic treatment tools for many patients today. Besides providing exceptional optics, GP lenses offer durability, high oxygen transmissibility, and additional ocular surface health benefits, all of which can make them excellent options for patients with a wide range of visual and clinical needs.
Due to the availability of extensive lens designs and customization features, GP lenses provide an opportunity for advanced and individualized treatment applications.
Available GP lens designs include scleral GP lenses that offer optical rehabilitation in those with corneal irregularities or therapeutic protection in patients suffering from dry eyes.1,2
Corneal GP lenses can be utilized for myopia control in the form of overnight wear of orthokeratology lenses.3
GP lenses are typically the preferred clinical treatment tool for patients requiring vision correction after corneal and keratorefractive surgeries.4
While generally less widely prescribed than soft contact lenses at the present, global data suggest increasing clinical utilization of GP lenses, including scleral and orthokeratology lenses specifically.5-7
H2O2 advantages
An important part of prescribing any non–single-use contact lens is making the right lens care recommendation. Hydrogen peroxide (H2O2) lens care systems have a long history of safe, effective use, and have features that differentiate them from other lens care systems often used for GP lenses (Figure 1).
First, H2O2 has a mechanism of disinfection that differs from that of the biocides in the formulations of other lens care systems. In addition to meeting International Organization for Standardization (ISO) disinfection efficacy standards against free-floating bacteria and fungi,8-10 H2O2’s mechanism of action allows it to effectively remove Acanthamoeba cysts and trophozoites,11 as well as bacterial and fungal biofilms.9,12
Biofilms can form on the lens surface or inside lens cases.13 While they are typically more resistant to disinfectants than planktonic microorganisms,14 studies suggest that H2O2 can more effectively remove biofilms than multipurpose solutions (MPS).9,12
Second, H2O2 lens care systems are preservative-free, which enhances their biocompatibility with the ocular surface. Preservatives contained in MPS and other GP lens care systems can be transferred onto the eyes at lens application and during lens wear.
The introduced preservatives can act as irritants, capable of altering corneal epithelial barrier integrity, which may be observed as diffuse punctate corneal staining and may negatively affect lens-wearing comfort.15 Due to the lack of added preservatives, corneal staining is essentially absent with H2O2 lens care use.15-19
Available systems safely neutralize H2O2 to concentrations that are well below human detection thresholds and are rapidly metabolized at the surface of the eye.20-22
Finally, today’s one-step H2O2 lens care systems support ease of use, which promotes better lens care compliance.23
H2O2 benefits GP lenses
Many specialized features of H2O2 lens care systems can have clear benefits for GP lens wearers, as well as wearers of hybrid lenses (which combine a central GP zone with a peripheral skirt made of a soft contact lens (SCL) material).
Lenses composed of GP materials are replaced less frequently than SCL disposable modalities. The clinical implication of this is that GP lenses can be exposed to higher cumulative levels of external irritants and microbial flora. Hence, the disinfection potency and biocompatibility of the recommended lens care system is crucial, and the disinfection efficacy of H2O2 lens care systems8-12 can help support proper lens hygiene over the prescribed life span of each lens.
Today’s one-step H2O2 systems can support effective disinfection by simplifying the lens care process. These systems combine disinfection and neutralization into a single step and do not require that lenses be rubbed prior to disinfection and neutralization, therefore making compliant lens care easier for patients. (Note that some patients will still benefit from being instructed to incorporate digital rubbing into their daily cleaning regimen.)
Lens case design allows patients to visualize the disinfection and neutralization process, which has the dual benefits of preventing patients from wearing their lenses before neutralization is complete and helping to promote timely case replacement.
Benefits to GP wearers
The preservative-free nature of H2O2 lens care offers important benefits to GP lens wearers.
Like with any patient, the eyes of wearers of GP and hybrid lenses may be sensitive to potential effects of added preservatives, so efforts to avoid preservative exposure, when possible, can be beneficial. This can be particularly pertinent for wearers of specific specialty GP lens designs.
Wearing scleral GP lenses, which cover a large proportion of the ocular surface, or orthokeratology lenses, which are worn overnight, can limit tear exchange. If using a non-H2O2 lens care system with these types of lenses, the reduced replenishment of tears between the contact lens and the surface of the eye24 can potentially prolong the exposure time of ocular tissues to irritating preservatives.
In these and other clinical scenarios, practitioners can help limit patients’ preservative-related ocular burden and support a successful lens-wearing experience by recommending H2O2 lens care. It is encouraging that a recent survey of eyecare practitioners found that H2O2 was the most commonly prescribed type of lens care system for scleral lens disinfection.25
References:
1. Barnett M, Mannis MJ. Contact lenses in the management of keratoconus. Cornea. 2011 Dec;30(12):1510-1516.
2. Bavinger JC, DeLoss K, Mian SI. Scleral lens use in dry eye syndrome. Curr Opin Ophthalmol. 2015 Jul;26(4):319-324.
3. Gifford P, GIfford KL. The future of myopia control contact lenses. Optom Vis Sci. 2016 Apr;93(4):336-343.
4. Bromley JG, Randleman B. Treatment strategies for corneal ectasia. Curr Opin Ophthalmol. 2010 Jul;21(14):255-258.
5. Morgan PB, Woods CA, Tranoudis I, et al. International contact lens prescribing in 2016. Contact Lens Spectrum. 2017;32:30-35.
6. Morgan PB, Woods CA, Tranoudis I, et al. International contact lens prescribing in 2017. Contact Lens Spectrum. 2018;33:28-33.
7. Nichols JJ. Contact lenses 2017. Contact Lens Spectrum. 2018;33:20-25-42.
8. Rosenthal RA, Buck S, McAnally C, Abshire R, Schlech B. Antimicrobial comparison of a new multi-purpose disinfecting solution to a 3% hydrogen peroxide system. CLAO J. 1999 Oct;25(4):213-217.
9. Szczotka-Flynn LB, Imamura Y, Chandra J, Mukherjee PK, Pearlman E, Ghannoum MA. Increased resistance of contact lens-related bacterial biofilms to antimicrobial activity of soft contact lens care solutions. Cornea. 2009 Sept;28(8):918-926.
10. Hildebrandt C, Wagner D, Kohlmann T, Kramer A. In-vitro analysis of the microbial activity of 6 contact lens care solutions. BMC Infect Dis. 2012 Oct 3;12:241.
11. Kilvington S, Lam A. Development of standardized methods for assessing biocidal efficacy of contact lens care solutions against Acanthamoeba trophozoites and cysts. Invest Ophthalmol Vis Sci. 2013 Jul 5;54(7):4527-4537.
12. Retuerto MA, Szczotka-Flynn L, Ho D, et al. Efficacy of care solutions against contact lens-associated Fusarium biofilms. Optom Vis Sci. 2012 Apr;89(4):382-391.
13. Szczotka-Flynn LB, Pearlman E, Ghannoum M. Microbial contamination of contact lenses, lens care solutions, and their accessories: a literature review. Eye & Contact Lens. 2010 Mar;36(2):116-129.
14. Zegans ME, Shanks RMQ, O’Toole GA. Bacterial biofilms and ocular infections. Ocul Surf. 2005 Apr;3(2):73-80.
15. Andrasko G, Ryen K. Corneal staining and comfort observed with traditional and silicone hydrogel lenses and multipurpose solution combinations. Optometry. 2008 Aug;79(8):444-454.
16. Andrasko G, Ryen K. A series of evaluations of MPS and silicone hydrogel lens combinations. Rev Cornea and Contact Lenses. 2007;143:36-42.
17. Carnt N, Evans V, Holden B, et al. IER matrix update: adding another silicone hydrogel. Contact Lens Spectrum. 2008;23:28-35.
18. Carnt N, Willcox M, Evans V, et al. Corneal staining: The IER matrix study. Contact Lens Spectrum. 2007;22:38-43.
19. Lazon de la Jara P, Papas E, Diec J, Naduvilath T, Willcox MD, Holden BA. Effect of lens care systems on the clinical performance of a contact lens. Optom Vis Sci. 2013 Apr;90(4):344-350.
20. Chalmers RL, McNally J. Ocular detection threshold for hydrogen peroxide: drops vs. lenses. Int Contact Lens Clin. 1988;15:351-367.
21. Chalmers RL. Hydrogen peroxide in anterior segment physiology: a literature review. Optom Vis Sci. 1989 Nov;66(11):796-803.
22. Chalmers RL. A review of the metabolism of hydrogen peroxide by external ocular structures. Int Contact Lens Clin. 1995;22:143-147.
23. Guthrie S, Dumbleton K, Jones L. Contact lens compliance: Is there a relationship between care system and compliance? Contact Lens Spectrum. 2016;31:40-43.
24. Paugh JR, Chen E, Heinrich C, Miller H, Gates T, Nguyen AL, Edrington T, Weissman BA. Silicone hydrogel and rigid gas-permeable scleral lens tear exchange. Eye & Contact Lens. 2018 Mar;44(2):97-101.
25. Harthan J, Nau CB, Barr J, Nau A, Shorter E, Chimato NT, Hodge DO, Schornack MM. Scleral Lens Prescription and Management Practices: The SCOPE Study. Eye Contact Lens. 2017 Apr 6. doi: 10.1097/ICL.0000000000000387. [Epub ahead of print].
26. Lowe R, Brennan N. Hydrogen peroxide disinfection of hydrogel contact lenses: an overview. Clin Exp Optom. 1987;70(6):190-197.

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.