Retinal findings present in pediatric case
Trauma evaluation leads to diagnosis, treatment for commotio retinae

Not long ago, a 9-year-old Caucasian girl presented for a trauma evaluation. She was a healthy child who took no medications. One day prior, she had been playing tennis and received a ball in her right eye. Her mother brought her in because her eye was a little red and ached slightly, as per the patient. She reported no visual changes, specifi cally no fl ashes of light, floaters, spider webs, shadows, or curtains in her vision.
Examination
Entering visual acuities unaided were 20/20 in each eye. Her pupils were normal and reactive to light. Extraocular muscle testing showed a full range of motion for both eyes with no pain or diplopia. Confrontation visual fi eld testing showed full fields for each eye. IOP by means of rebound tonometry was 13 mmHg in the right eye and 15 mmHg in the left eye. An anterior segment examination showed moderate injection of the right eye’s bulbar conjunctiva, more so nasally. Otherwise, the lids and corneas were clear, angles were open, irises were intact, and anterior chambers were clear, quiet, and well formed. Similarly, a gonioscopy showed no evidence of angle recession or bleeding.
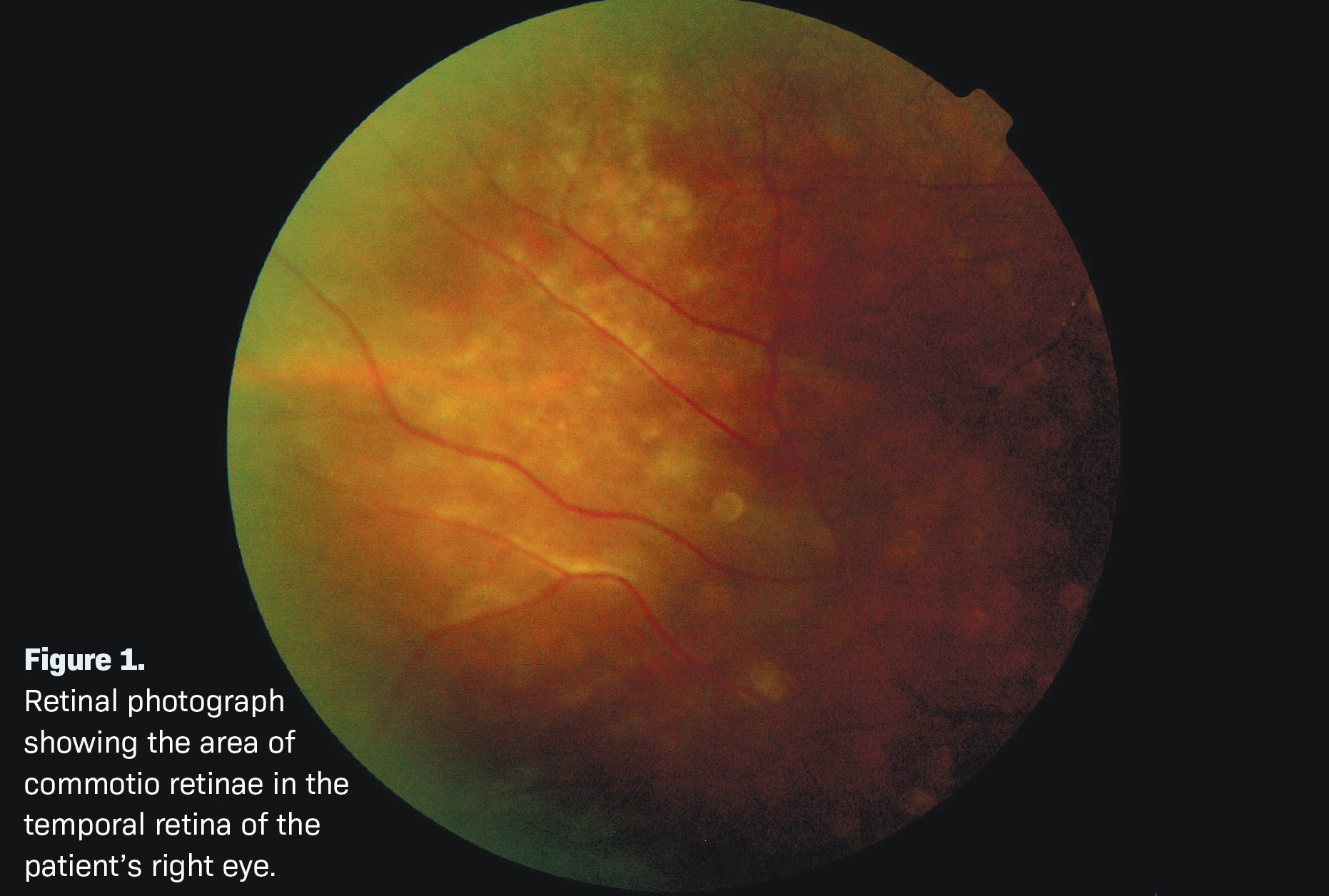
The patient was dilated with tropicamide 1% in each eye because there was a history of trauma. The optic nerves were distinct and well perfused and the maculas were flat with healthy foveal light reflexes. The vasculature was normal, and there was no evidence of a retinal tear or detachment. However, the patient’s temporal midperipheral retina had an area of whitish sheen which changed as I changed the angle of Figure 1.
Retinal photograph showing the area of commotio retinae in the temporal retina of the patient’s right eye. my 20-D condensing lens (see Figure 1).
I asked the patient and her mother again if there had been any visual changes, and they again reported none. Then I performed some high-definition raster scans by means of spectral domain optical coherence tomography (OCT) of the area, to ensure that I wasn’t missing a subtle detachment (see Figure 2).
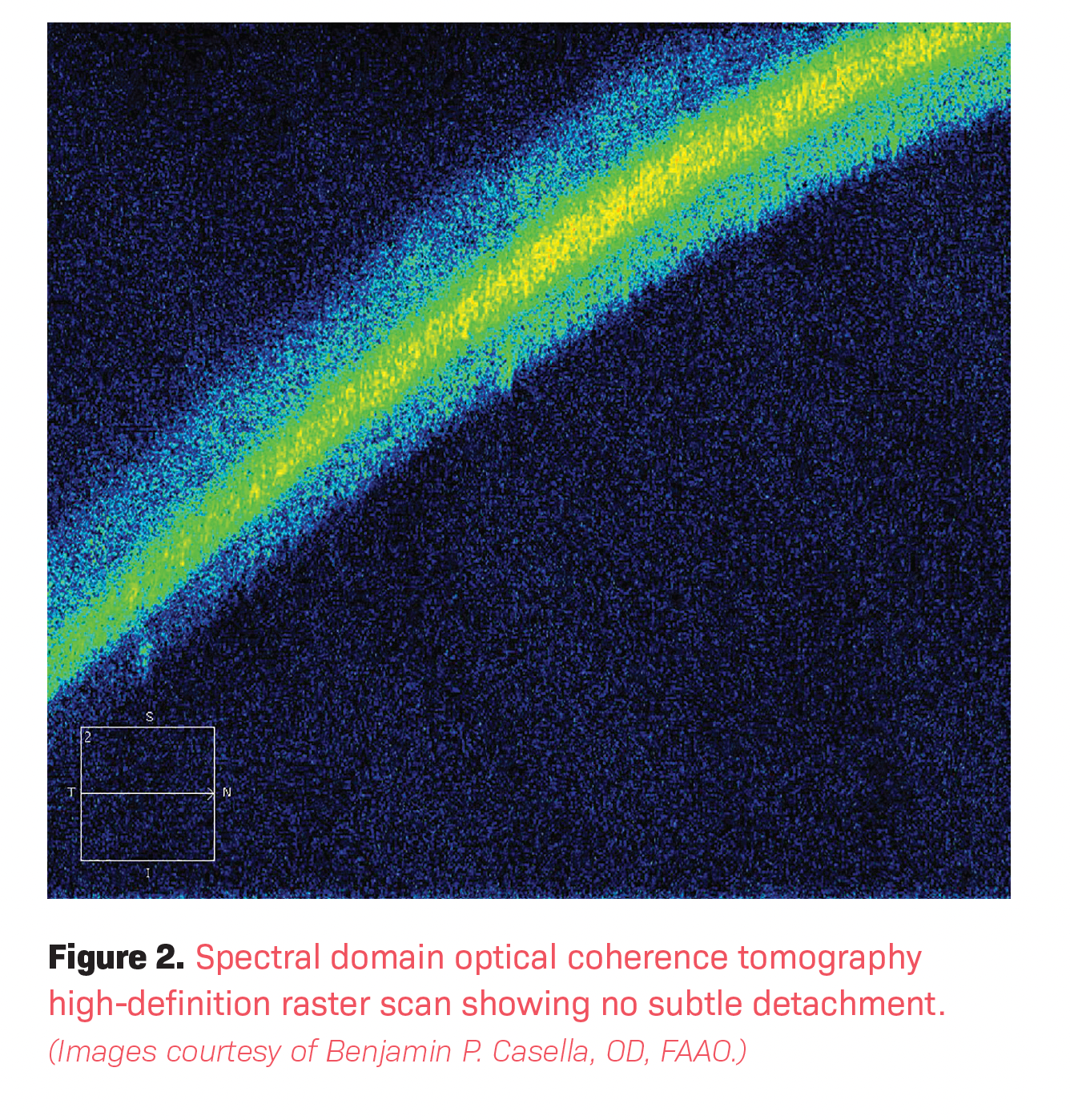
Admittedly, and due to the relative peripheral location of the area, the images were not of the highest quality. However, they did rule out any subtle retinal detachments. I made a diagnosis of mild conjunctival inflammation following trauma to the right eye and commotio retinae of the right eye. I prescribed prednisolone acetate 1% ophthalmic suspension to be used 4 times a day in the right eye and invited the patient back in 2 to 3 days for a follow-up and to be dilated again. I also educated them on signs and symptoms of retinal detachment or tear.
Follow-up
At that visit, 3 days later, the patient’s mother reported that her eye had cleared up after a couple of doses of the prednisolone acetate drops. She reported no visual changes at all and felt completely fine. Unaided visual acuities were again 20/20 in each eye. Pupils were normal and reactive to light, and the patient’s right bulbar conjunctiva was white and quiet. IOPs by means of rebound tonometry were 15 mmHg in the right eye and 17 mmHg in the left eye. A dilated fundoscopy showed complete resolution of the area of commotio retinae in the right eye’s temporal midperiphery.
No other abnormalities were present. At this point, I educated the patient and her mother on a quick tapering schedule for the drops and again on signs and symptoms of retinal detachment or tear. I invited them back in 1 week for one more follow-up and to check again for any visual issues. At this visit, unaided visual acuities were 20/20 in each eye and the girl’s pupils were normal and reactive to light. IOP by means of rebound tonometry was 17 mmHg in each eye. I determined that the patient had +0.25 D hyperopia in each eye with good near acuity, good accommodation, and good binocular function. Examination showed no abnormalities in either eye, and the patient reported no visual changes. At that point, I invited her back in 1 year for a comprehensive eye examination and follow-up.
Conclusion
Commotio retinae was first described in 1873 by Rudolph Berlin.1 When it involves the macula, it is sometimes (albeit incorrectly) referred to as Berlin edema.1 Edema is not what creates the whitish sheen; disruption of the outer segment layer of the retina is mostly responsible for this appearance. Numerous retinal layers, from the inner retina to the retinal pigment epithelium, can be involved.1 Although visual damage can occur if the retinal sequelae of commotio is significant enough, this entity is typically self-limiting and resolves on its own.
Reference
1. Park JY, Nam WH, Kim SH, Jang SY, Ohn YH, Park TK. Evaluation of the central macula in commotio retinae not associated with other types of traumatic retinopathy. Korean J Ophthalmol. 2011 Aug;25(4):262-267. doi:10.3341/kjo.2011.25.4.262
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.