When to refer patients with diabetic retinopathy
The time to refer patients with diabetic retinopathy (DR) or diabetic macular edema (DME) depends on disease staging and location, especially now that ODs have new treatment options for lessening disease severity.
Guidelines
Patients with DR or DME need to be referred when eye-specific treatment is indicated, necessary, or should be considered by a retinal specialist.
The referral should be based on standards of care and/or clinical practice guidelines for the management and treatment of diabetes-related eye disease.
Related: How diabetes affects your patients
Multiple clinical practice guidelines exist, including those from ophthalmology, optometry, and organizations representing diabetes providers.1-4
In general, these guidelines focus on referral and treatment of vision-threatening diabetic retinopathy; that is, proliferative diabetic retinopathy (PDR, defined as neovascularization of the optic nerve or retina) and center-involved DME (CI-DME, defined as central subfield thickening on optical coherence tomography examination [OCT]).
Study results
Additionally, the Early Treatment Diabetic Retinopathy Study (ETDRS) suggested benefits of pan-retinal photocoagulation (PRP) not only in patients with PDR, but also for patients having type 2 diabetes and severe non-proliferative diabetic retinopathy (NPDR), as well as macular laser for those with clinically significant macular edema (CSME) per specific ETDRS criteria.5
Related: Using imaging to manage diabetic retinopathy
Intravitreal injection of anti-VEGF therapy (AVT) for CI-DME has become the gold standard because it results in visual and anatomical outcomes superior to laser based on multiple clinical trials. However, it has not yet become the standard for treatment of either NPDR or PDR.6
More recently, large prospective trials have shown that earlier intervention with AVT in non-proliferative DR (NPDR) can not only stabilize, but also results in disease regression for a significant percentage of patients with less severe disease, as well as lower the risk of developing PDR or CI-DME.7
Moreover, anti-VEGF has been shown to be non-inferior to PRP for treating PDR (DRCR.net Protocol S).8
FDA approval
In 2017, ranibizumab (Lucentis, Genentech) received FDA approval for the treatment of any level of DR with or without the presence of DME, and aflibercept (Eylea, Regeneron) is expected to receive such approval in the near future.
The data for both ranibizumab and aflibercept show that significantly more patients with moderately severe or worse NPDR have at least a two-step improvement in Diabetic Retinopathy Severity Scale (DRSS) when given AVT, such as a patient with severe NPDR improving to either mild or (more commonly) moderate NPDR, and that these patients are far less likely to develop a sight-threatening disease.
Of course, all this begs the question: When should an OD refer any specific patient to a retinal specialist for consideration of treatment?
The answer is not always straightforward, given several important factors with which ODs must contend.
Diabetes duration and metabolic control-especially duration/stability/variability of blood sugar and pressure control-modulate individualized risk and may prompt an earlier referral for some patients than others.
Evidence shows that some patients are more likely to be lost to follow-up based on specific characteristics-socioeconomic class, level of education, and age-and, as such, referring optometrists might want to transfer care earlier rather than later.9
Different retinal specialists have different criteria for treatment based on their own clinical experience and may or may not use AVT in the absence of DME.
Some important retinal findings can be hard to visualize based on patient cooperation, optometrists’ instrumentation, and clarity of the ocular media. The complexity of ETDRS severity grading can make even seasoned practitioners’ eyes glaze over.
Additionally, retinal specialists have said they can’t find grading scales for DR that are helpful in comparison to widefield fluorescein angiography when deciding who does and doesn’t need treatment.
When to refer
Optometrists should refer patients when they are no longer comfortable managing specific cases of diabetes and/or diabetic retinopathy. We all have our strengths and weaknesses and should remember that we have colleagues in both optometry and ophthalmology who are on our side as well as on our patients’ sides.
Given this, it makes increasing sense to refer patients who have moderately severe or worse non-proliferative diabetic retinopathy-in the “vicinity” of ETDRS severity level 47 or worse: multiple intra-retinal hemorrhages in two or more quadrants, any definite vein beading, any prominent IRMA- especially if a disease progression via serial fundus photography is detected.
A local retina specialist should be consulted to ascertain their referral and treatment preferences as well as to facilitate informed conversation with patients based on reasonable expectations.
If a patient has glycosylated hemoglobin > 8 percent, and especially if they have an initial and/or long-term history of poor glycemic control, consider earlier referral.
This should also be done if patients aren’t getting regular diabetes and eye care, are monocular/have amblyopia, have anxiety or depression, or display apparent risk factors for more severe DR10 (ask patients explicitly; you’ll be surprised how many patients will answer in the affirmative when a caring provider asks).
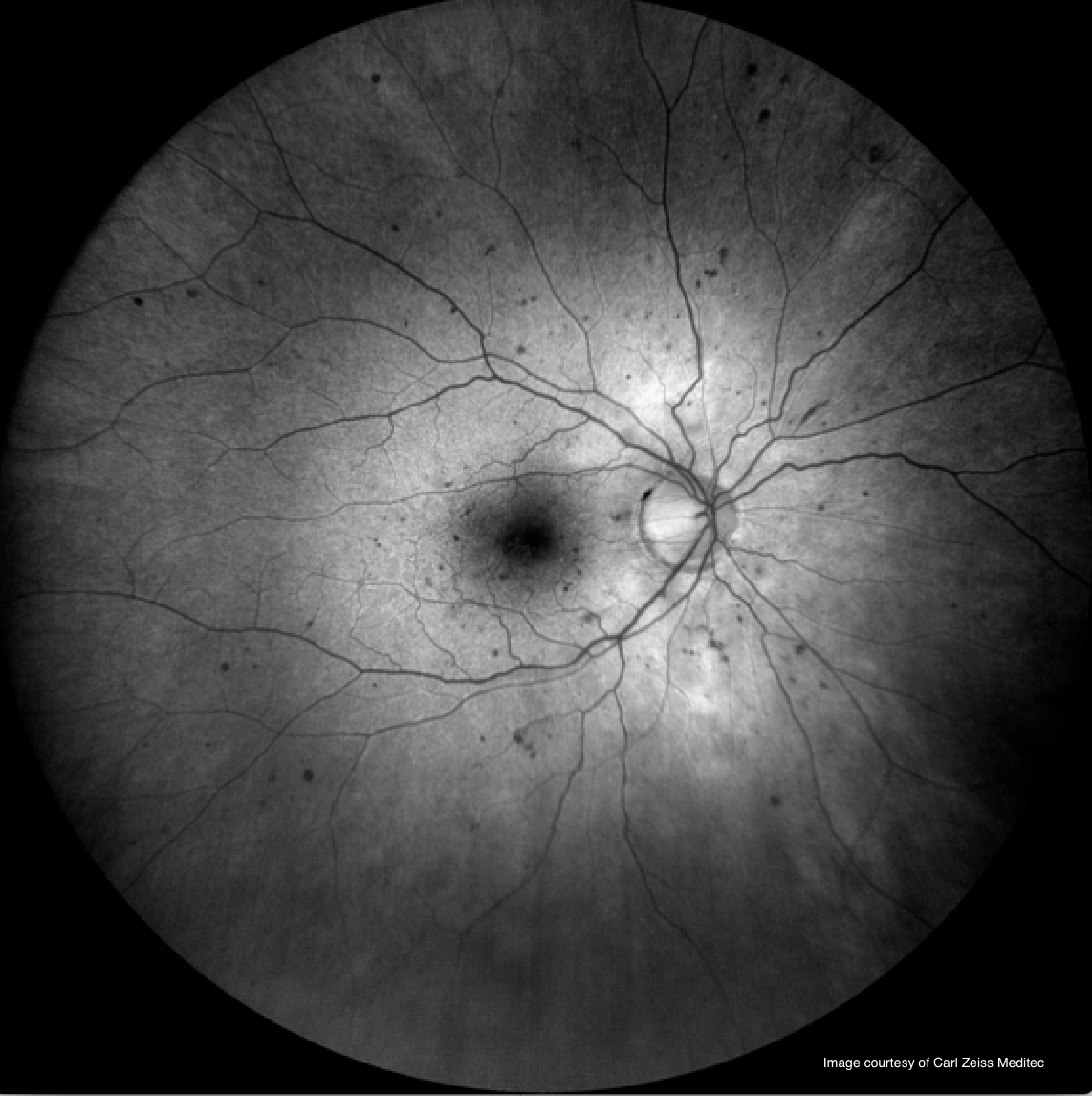
Dilate patients with diabetes and use technology to detect abnormalities that might be missed with conventional fundus examination techniques: serial fundus imaging and ultra-widefield imaging using red-free and, even better, fundus autofluorescence (see Figure 1).
Use OCT to detect sub-clinical DME and inner retinal thinning (retinal diabetic neuropathy) and OCTA to detect non-perfusion, sub-clinical microaneurysms and other capillary abnormalities.
Bottom line
ODs should refer patients who they believe would benefit from treatment now or in the near future in collaboration with a local retinal specialist.
The paradigm for treatment and management of diabetic retinopathy is changing. By all accounts, the new standard is shifting toward treatments that not only prevent severe vision loss late in the game but lessen disease severity early in the game.
References:
1. American Academy of Ophthalmology Retina/Vitreous Panel. Preferred Practice Guidelines. Diabetic Retinopathy. San Francisco, CA: American Academy of Ophthalmology; 2017. Available at: https://www.aao.org/preferred-practice-pattern/diabetic-retinopathy-ppp-updated-2017. Accessed 10/19/18.
2. International Council of Ophthalmology Guidelines for Diabetic Eye Care 2017. Available at: http://www.icoph.org/downloads/ICOGuidelinesforDiabeticEyeCare.pdf. Accessed 10/19/18.
3. American Optometric Association. Eye Care of the Patient with Diabetes Mellitus. Evidence-Based Clinical Practice Guideline 2014. Available at: https://www.aoa.org/Documents/EBO/EyeCareOfThePatientWithDiabetesMellitus%20CPG3.pdf. Accessed 10/20/18.
4. Soloman SD, Chew E, Duh EJ, Sobrin L, Sun JK, VanderBeek BL, Wykoff CC, Gardner TW. American Diabetes Association. Diabetic Retinopathy: A Position Statement by the American Diabetes Association. Diabetes Care. 2017 Mar; 40(3): 412-418.
5. El Rami H, Barham R, Sun JK, Silva PS. Evidence-Based Treatment of Diabetic Retinopathy. Semin Ophthalmol. 2017;32(1):67-74.
6. Virgili G, Parravano M, Evans JR, Gordon I, Lucenteforte E. Anti-vascular endothelial growth factor for diabetic macular oedema: a network meta-analysis. Cochrane Database Systematic Reviews. 2017 Jun 22;6:CD007419.
7. Bressler SB, Liu D, Glassman AR, Castellarin AA, Jampol LM, Kaufman PL, Melia M, Singh H, Wells JA. Change in Diabetic Retinopathy Through 2 Years: Secondary Analysis of a Randomized Clinical Trial Comparing Aflibercept, Bevacizumab, and Ranibizumab. JAMA Ophthalmology. 2017;135(6):558-568.
8. Gross JG, Glassman AR, Jampol LM, Inusah S, Aiello LP, Antoszyk AN, Baker, CW, Berger BB, Bressler NM, Browning D, Elman MJ, Ferris III FL, Friedman SM, Marcus DM, Melia M, Stockdale CR, Sun JK, Beck RW, Diabetic Retinopathy Clinical Research Network. Panretinal Photocoagulation vs Intravitreous Ranibizumab for Proliferative Diabetic Retinopathy: A Randomized Clinical Trial. JAMA Network. 2015;314(20):2137-2146.
9. Barsegian A, Kotlyar B, Lee J, Salifu MO, McFarlane SI. Diabetic Retinopathy: Focus on Minority Populations. International Journal of Clinical Endocrinology and Metabolism. 2017. Available at: https://www.peertechz.com/articles/diabetic-retinopathy-focus-on-minority-populations.pdf. Accessed 10/22/18.
10. Rees G, Xie J, Fenwick EK, Sturrock BA, Finger R, Rogers SL, Lim L, Lamoureux EL. Association Between Diabetes-Related Eye Complications and Symptoms of Anxiety and Depression. JAMA Ophthalmol. 2016 Sep 1;134(9):1007-14.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.