Best practices for comanaging crosslinking patients
We practice a few blocks from each other in a tertiary-care surgical practice and a primary-care optometry practice, respectively. Although we comanage different types of surgical cases, one of the most rewarding recent developments has been the opportunity to jointly care for patients with keratoconus.
New technology has disrupted the way we approach these patients. In the past, optometrists have mostly watched and waited, trying to keep keratoconus patients seeing well for as long as possible in contact lenses.
Historically, as many as 1 in 5 patients with progressive keratoconus have required a corneal transplant, with more than half of those needing multiple transplants within 20 years.1,2
Related: Collagen corneal cross-linking for keratoconus
Corneal crosslinking
With the approval in 2016 of corneal collagen cross-linking (CXL) using the Avedro cross-linking suite (Photrexa Viscous, Photrexa, and the KXL System), the paradigm has shifted to one of intervening as early as possible with keratoconus patients. Multiple studies have shown that CXL may slow or halt the progression of keratoconus, providing better visual acuity and decreased corneal bulging up to 10 years post-treatment.3-6
The procedure uses Photrexa Viscous (Riboflavin-5’-phosphate) drops applied to the corneal stroma; the drops are activated by ultraviolet A (UVA) light over the course of approximately 30 minutes, resulting in new chemical bonds that stiffen collagen strands in the cornea.7,8
The CXL procedure approved in the United States requires removal of the epithelium; a phase 3 clinical trial of an Avedro epi-on technique is underway.
Collaboration opportunity
In many ways, keratoconus is an ideal condition for collaboration among optometrists and ophthalmologists because it presents three distinct challenges that can best be addressed by multiple professionals working together.
The first challenge is detecting keratoconus early before the cornea is irreparably damaged. These patients typically don’t know they have keratoconus and are unlikely to present to a practice that performs CXL; rather, they will visit their primary-care optometrist in the hopes of improving their refractive corrections. That gives the optometrist the opportunity to diagnose and refer the patient for a full corneal evaluation.
Once keratoconus has been diagnosed, the second challenge is to prevent further corneal changes that may otherwise lead to a corneal transplant. We strongly believe that it is important to recommend CXL as soon as there is evidence of progression because it is the only therapy shown to be effective in slowing these changes.9
Related: Keratoconus: cracking the corneal code
Finally, the third challenge is helping patients to see better, wherever they are in the stages of keratoconus progression. More vision correction tools are available to us when keratoconus is stabilized earlier in the course of the disease.
A patient who is treated early may be able to continue to wear soft contact lenses or glasses for the rest of his life. Others may need rigid gas permeable (RGP), scleral, or hybrid contact lenses to obtain their best acuity. Their primary-care optometrists are best positioned to prescribe the vision correction that will work best for the patient.
Although patients may expeirence some improvement in visual acuity with CXL, improved visual acuity is not the goal of the procedure. It is important for patients to understand that stopping progression and improving vision are two different steps in their journeys.
Related: 7 strategies for fitting keratoconus patients
Early detection case
Optometrists who accept broad-based vision and/or medical insurance plans will be best positioned to attract a broad range of patients to their practices, including those in the demographic in which keratoconus first develops: teens and young adults.
A patient who recently returned for his two-year follow-up visit after CXL illustrates the benefits of early detection. This a 27-year-old male found his contact lens prescription was changing more rapidly in his right eye than his left. Uncorrected visual acuities were 20/40- OD and 20/20 OS. He demonstrated aggressive eye-rubbing in the exam chair.
While he did correct to 20/20- with +0.75-3.00 x 070 in the right eye, there was mild anterior bowing to his inferior cornea in the right eye and sub-clinical findings on his left eye. All other slit lamp exam findings were normal.
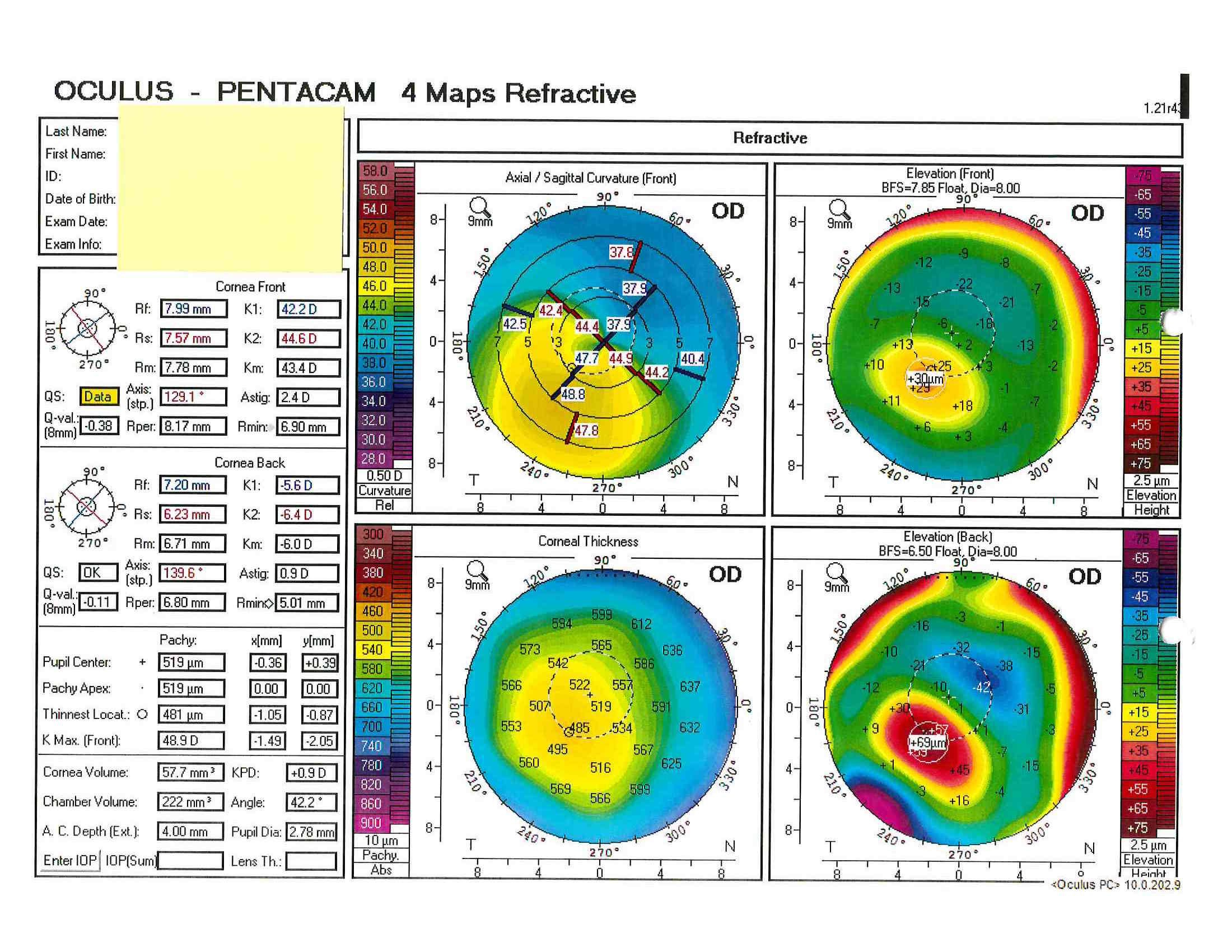
Baseline Pentacam (Oculus) tomographies contributed to the diagnosis of progressive keratoconus OD (Figure 1) and forme fruste keratoconus OS (Figure 2).
CXL was performed in the right eye, with planned close monitoring of the left eye. We saw improvements in the cornea and best-corrected visual acuity to 20/20- at six months (Figure 3).
Now, at two years post-CXL OD, the patient continues to be correctible to 20/20 OD and OS with greatly improved corneal tomography (Figure 4). He is able to wear glasses and soft contact lenses and has ceased eye rubbing. The patient’s corneal scans in the left eye have continued to be stable.
Related: Top 10 questions about cross-linking
Diagnosing keratoconus
In working to identify early keratoconic changes and risk factors for keratoconus, we have learned is that simply raising the index of suspicion is important, independent of any specific diagnostic tools.
Watch for these red flags:
• Inability to correct an otherwise healthy young eye to 20/20
• A large change in refraction over the course of a year
- 0.50 D myopic change
- 1.00 D cylinder change
• Habitual eye rubbing, particularly in combination with any of the above
Traditional diagnostic tools such as manual keratometry, autorefractor autokeratometry, slit-lamp exam, and retinoscopy are important first steps. However, accurately tracking changes in corneal curvature over time requires access to advanced topography/tomography technologies such as Pentacam or Orbscan (Bausch + Lomb) that aren’t available to all primary-care optometrists.
We recommend that primary-care optometrists seek out and partner with ophthalmic practices that do have these devices.
Technicians at the surgical practice can provide imaging services at the request of the primary-care optometrist.
This allows the referring optometrist to make a more informed decision about whether a CXL consult is needed, which can often be done quickly and with less hassle for the patient.
We also recommend erring on the side of caution and making a referral for further diagnostic evaluation whenever there is a reasonable suspicion of keratoconus.
Related: Why keratometry is important
Sharing the care
Once a referral for evaluation has been made, there are a number of steps in the process (see “Logistics of collaborative care for keratoconus”). Patients need to be educated about keratoconus, crosslinking, and the ongoing need for refractive correction.
More than 90 percent of commercially insured patients now have coverage for CXL, but practices often need to seek pre-authorization and review coverage, co-insurance amounts, and financing with patients.
Comanagement partners can’t overcommunicate in caring for keratoconus patients. It is very important for the surgical practice to understand the areas of concern and the reason for the referral. Surgical partners should, in turn, communicate their diagnosis and treatment plan, as well as the desired postoperative care regimen.
Optometrists should visit the cross-linking practice, seek out more information about the procedure, and be confident in their relationships with the doctors who will perform the crosslinking (see “Comanagement partnership qualities”).
Related: 5 features of successful comanagement
Most surgical practices will send the patient back to the referring optometrist for the first (~ one week) or second (one month) postop visit. They may want to see the patient back at six or 12 months to repeat imaging and confirm stability.
It is important to know that doctors can be reimbursed by insurance for these follow-up visits. Unlike cataract surgery, there is currently no global period for crosslinking, so follow-up appointments should be billed as office visits.
The bottom line is that collaborating to provide care for patients with keratoconus is very rewarding for all involved. Not only are there interesting clinical challenges in managing patients undergoing corneal collagen crosslinking, but CXL offers a fantastic opportunity for ODs to improve patients’ long-term visual acuity and corneal health outcomes.
Read more comanagement articles here
About the authorsDr. Ibach is a cornea, glaucoma, cataract, and refractive surgery specialist. His practice was a clinical trial site for the FDA trial leading to approval of epi-off CXL and ongoing studies of epi-on CXL. He is a consultant for Avedro. Dr. Ibach enjoys spending as many days as possible at the lake with his family.
mitch.ibach@vancethompsonvision.com
Dr. Sayler is an avid golfer and enjoys spending time on his hobby farm. He does not have any relevant financial interests to disclose.
jsayler@siouxfallsfamilyvision.com
References:
1. Maharana PK, Agarwal K, Jhanji V, Vajpayee RB. Deep anterior lamellar keratoplasty for keratoconus: a review. Eye Contact Lens. 2014 Nov;40(6):382-9.
2. Pramanik S, Musch DC, Sutphin JE, Farjo AA. Extended long-term outcomes of penetrating keratoplasty for keratoconus. Ophthalmology. 2006 Sep;113(9):1633-8.
3. Hersh PS, Stulting RD, Muller D, Durrie DS, Rajpal RK; U.S. Crosslinking Study Group. United States multicenter clinical trial of corneal collagen crosslinking for keratoconus treatment. Ophthalmology. 2017 Oct;124(9):1475-1484.
4. O'Brart, DP, Patel P, Lascaratos G, Wagh VK, Tam C, Lee J, O'Brart NA. Corneal cross-linking to halt the progression of keratoconus and corneal ectasia: Seven-year follow-up. Am J Ophthalmol. 2015 Dec;160(6):1154-63.
5. Poli M, Lefevre A, Auxenfans C, Burillon C. Corneal collagen cross-linking for the treatment of progressive corneal ectasia: 6-year prospective outcome in a French population. Am J Ophthalmol 2015 Oct;160(4):654-62.
6. Raiskup F, Theuring A, Pillunat LE, Spoerl E. Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressive keratoconus: ten-year results. J Cataract Refract Surg. 2015 Jan;41(1):41-6.
7. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol 2003;135(5):620-7.
8. Shetty R, Pahuja NK, Nuijts RM, Ajani A, Jayadev C, Sharma C, Nagaraja H. Current protocols of corneal collagen cross-linking: Visual, refractive, and tomographic outcomes. Am J Ophthalmol. 2015 Aug;160(2):243-9.
9. Hersh PS, Stulting RD, Muller D, Durrie DS, Rajpal RK; U.S. Crosslinking Study Group. United States Multicenter Clinical Trial of Corneal Collagen Crosslinking for Keratoconus Treatment. Ophthalmology. 2017 Sep;124(9):1259-1270.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.