Cataract surgery comanagement from the other side

As director of optometry at a surgical center where almost all of our patients are referred by their ODs, high-level comanagement is part of what I do every day. My colleagues and I think this is the future of health care: ophthalmologists focus their skills and experience in the operating room while optometrists fulfill the full scope of their abilities to comanage diseases as patients’ primary eyecare practitioners. When these two specialists work together, each doing what they're best trained to do, patients benefit.
One of the most common surgeries we comanage with referring ODs is cataract surgery. We work with referring ODs so they are aware of the latest options for this ever-evolving procedure, which helps them refer patients at the right time, having educated patients about their options.
At that point, our office takes over preoperative care, education, decision-making, and finally surgery. Postoperatively, patients return to their optometrists for follow-up care. In comanaging patient care after cataract surgery, we all help ensure that patients have the best possible outcomes.
Related: Understand the basics of cataract surery measurements
Transfers after surgery
In our practice model, referring optometrists are in the loop every step of the way of their patients’ journeys-from patient referral and our practice’s initial evaluation, to preoperative care such as treatment in our dry eye clinic, to surgical decisions and the procedure itself, we continually inform and confer with each other. Referring ODs’ ongoing involvement with their patients makes the postoperative transition quite smooth.
The handoff point depends on the optometrist’s comfort level and surgical success; however, many referring ODs immediately assume care by seeing patients for the one-day visit after cataract surgery. Primary care ODs continue to see patients for one-week and one-month examinations to ensure that patients are achieving the desired visual outcomes on schedule without complications or discomfort.
Modern cataract surgery has become so advanced that it is very routine and reliable with low risk for complications. Our surgeons feel confident in sending patients back to their optometrists, knowing that ODs excel at identifying and managing potential complications.
In addition, referring ODs continue the open communication among their offices and ours, sending a mutually agreed-upon report on every patient. Anytime a patient experiences a minor complication, a patients feels dissatisfied about any aspect of the experience, or something unusual happens, our surgeons want to know about it and the referring ODs keep our office updated.
Related: How to help the unhappy patient after successful surgery
Postoperative medications
Evaluating patients for complications is an essential part of the referring ODs’ responsibility, and one of the most effective ways to prevent complications is to ensure patients are compliant with postoperative medications.
Traditionally, post-cataract patients are placed on a corticosteroid like prednisolone (Pred Forte, Allergan) or loteprednol (Lotemax, Bausch + Lomb), a non-steroidal anti-inflammatory drug (NSAID) such as bromfenac (Prolensa, Bausch + Lomb) or nepafenac (Ilevro, Novartis), and antibiotics such as moxifloxacin (Vigamox, Alcon) and besifloaxin (Besivance, Bausch + Lomb).
The antibiotic is prescribed for about one week, while the corticosteroid and the NSAID are used for one month. If a patient is considered high risk for cystoid macular edema (CME), we might prescribe the NSAID for two months.
In our experience, we have found that it is best not to allow generic substitutions for any of these drugs. We understand that cost is always a concern, but the small savings is not worth the risk. We find that generics are not as reliable and are more likely to induce ocular surface problems or CME.
When we explain these risks, patients rarely choose generics. If they do, we have them sign a waiver attesting that they were warned of the additional risk and accept responsibility. If the patient cannot truly afford medicine, we will utilize other treatment options.
With the same goals in mind of efficacy and compliance, we follow new medications for cataract patients. Finding anti-inflammatory therapies that require a lower dosage is one of our primary interests. Patients get frustrated with the number of drops they need to use after surgery, and we have found that when we are able to decrease the dosing frequency of a medication, we increase compliance.
For post-cataract pain and inflammation, we are excited about loteprednol etabonate suspension 1% (Inveltys , Kala Pharmaceuticals). The drug penetrates the tear film mucins, delivering more than 3.75 times of loteprednol etabonate to target ocular tissues compared to traditional suspension formulations in a preclinical study.1 It is the first corticosteroid approved for twice-a-day (bid) dosing following ocular surgery.1
The best patient experience
How does this process play out from the patient’s perspective? The patient’s optometrist refers him for cataract surgery, then the patient has multiple visits to our practice and, potentially, several weeks of treatment for ocular surface disease. He has the surgery, then returns to his optometrist for a month of follow-up care.
We work hard to ensure that throughout this process, the patient’s practitioners are on the same page and each doctor or staff member delivers the same message to patients at every step. That consistency is an important part of education within our center and with our referring ODs.
Of course, no patient has a good experience if the visual results are poor, and we do everything we can to ensure that measurements are accurate and surgery is a success. Another potential reason for dissatisfaction is discomfort during the healing process.
Related: 5 steps to manage cataract patient expectations
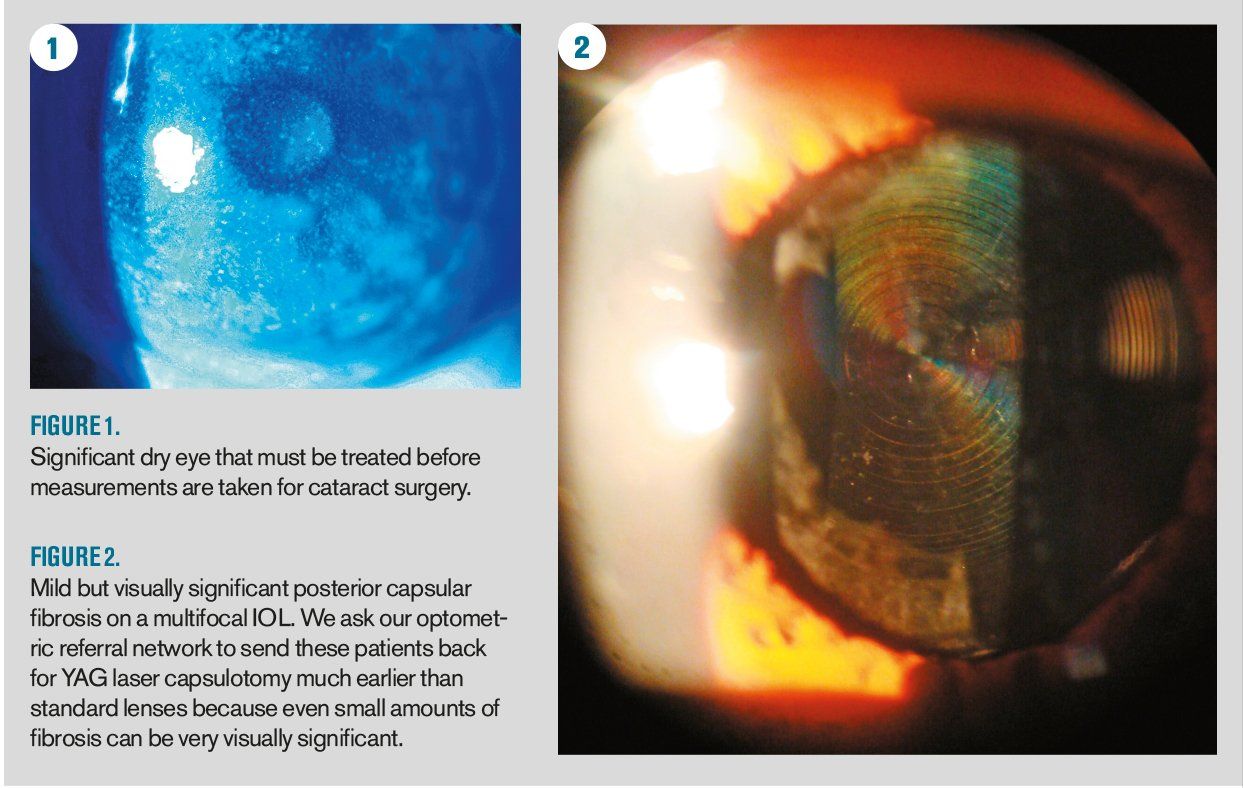
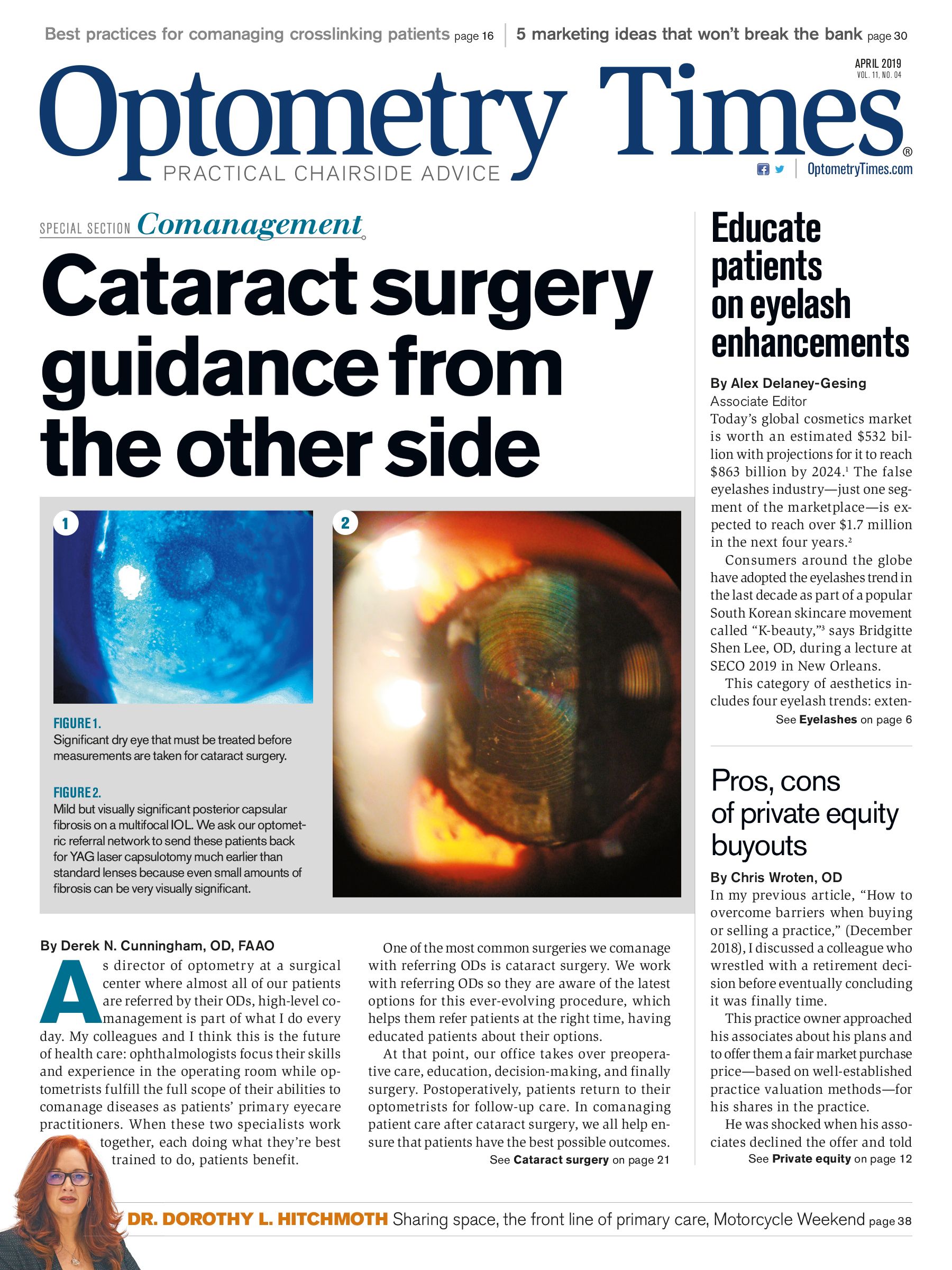
One way we prevent poor visual results and healing discomfort is aggressively treating dry eye before surgery with prescription medications like cyclosporine (Restasis, Allergan) or lifitegrast (Xiidra, Takeda) and possibly thermal pulsation therapy (LipiFlow, Johnson & Johnson Vision). This ensures accurate biometry and reduces ocular surface discomfort after surgery. Almost 80 percent of our patients opt for premium intraocular lenses (IOLs) such as Tecnis Symfony extended depth-of-focus lens, Tecnis Multifocal (Johnson & Johnson Vision), and Bausch + Lomb Crystalens-even minor amounts of ocular surface disease during biometry can skew visual results.
In addition, we need to make sure to prescribe medications that adequately control pain and inflammation after surgery, and then, of course, make sure patients are complying with the drops.
Our patients tell us that they have received an exceptional level of care. They appreciate that we make group decisions with their optometrists, and they like that we take more time before surgery to take multiple measurements and discuss their needs to produce better results.
We have learned that when patients see referring and comanagaing doctors taking their roles in cataract care seriously, they put more effort into their own role, complying with pre- and postoperative care. Their help and their satisfaction help the comanagement process succeed.
Related: Choose your words carefully with surgery patients
About the author
Dr. Cunningham is director of the Dell Eye Institute for Dry Eye Research. He has a special interest in sports vision and performance and provides vision training services to several college and professional sports teams. He is the co-founder of SportsVisionPros.com and spends some of his free time in the broadcast booth helping announce for the University of Texas Longhorns football games. Dr. Cunningham serves a consultant to Kala Pharmaceuticals, Valeant, Alcon, Shire, and Eyevance Pharmaceutical Companies. He is also a consultant to Johnson & Johnson Vision, TearLab, BVI, and Nike.
derek.n.cunningham@gmail.com
References:
1. Schopf L, Enlow E, Popov A, Bourassa J, Chen H. Ocular pharmacokinetics of a novel loteprednol etabonate 0.4% ophthalmic formulation. Ophthalmol Ther. 2014 Dec;3(1-2):63-72.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.