As seen on TV: Doing harm, not help, to the ocular surface

An interesting ophthalmologic emergency room (ER) study found that 40.5 percent of the patients who reported to the ER for an eye-related condition used a self-prescribed therapy to solve their eye problems.1
Remedies for the eye concern include:1
– “Homemade” eye solutions
–Folk remedies
–Herbal infusions
– Breast milk
– Lemon juice
– Holy water
– Boric acid mixtures
– Urine,
– Commercially available or pharmacist-recommended products
Amazingly, use of these therapies went beyond treating the common red eye and were used to manage acute, vision-threating injury.
This information begs the question as to what your patients may be using to soothe, treat, or “beautify” the components of the ocular surface system.
Related: What's your red eye protocol? Balanced functional unit
Consider that dry eye disease is a multifactorial disease that affects one or more elements of the ocular surface functional unit. The ocular surface functional unit includes:
– Tear film
– Cornea
– Limbus
– Conjunctiva
– Lid margin
– Muco-epidermal junction
– Lacrimal gland tubulo-acinar epithelia
– Lacrimal drainage system
– Eyelids
Added to this are considerations of blink rate and completeness, tear spreading abnormalities related to conjunctival degenerations or compromised eyelid position and/or function.
Are your patients manipulating this delicately balanced environment in any way?
Since the first television commercials, television broadcast has marketed products to viewers, including those that are “eye related.”
Now, there are a myriad of information suppliers and marketing platforms that include Instagram and Twitter as well as online suppliers, most notably Amazon, that can advertise and supply items from around the globe.
Remember that many of these are products that are unregulated or monitored by any governing agency.
Related: How digital device usage is affecting youth Digital device usage
In the setting of ocular surface disease, a patient’s blink rate and blink excursion is of significant concern. Any ergonomic, positional, dysfunctional, surgical, or other component that can negatively impact the proper mechanism of the natural, complete blink may tax the tear film’s efficacy and hence, ocular surface homeostasis.
Digital device use has been associated with dry eye syndrome, in part related to compromising the quality of the blink.2,3 Reductions in blink rate may be substantial.
For example, Patel et al4 reported a mean rate of 18.4 blinks per minute before computer use, decreasing to 3.6 blinks per minute during operation. Tsubota and Nakamori5 observed a mean rate of 22 blinks per minute among office workers under relaxed conditions, reducing to seven blinks per minute when viewing an electronic display.
Related: How to guide patients in the use of digital devices

Across all age groups in developed nations, engagement with digital devices has increased substantially in recent years, particularly in the field of mobile media.6
A European study reported that by 3 years of age, 68 percent of children regularly use a computer, and 54 percent undertake online activities.7
In older age groups, use of technology is growing rapidly. Between 2011 and 2017, the proportion of the population classed as “recent Internet users” (within the last three months) more than doubled in the 75 years and over age group, and increased from 52 percent to 77.5 percent in those aged 65 to 74 years.8
U.S. data indicates that 37 percent of adults aged 60 years and over spend five or more hours per day using digital devices.9
Marketed to parents of infants and children, teenagers, working adults, and seniors, are a multitude of gizmos and gadgets, gimmicks and hacks to make digital devices “easier” for extended viewing in inappropriate, visually-sound postures.
Additionally, electronic games and toys, educational products, and entertainment are produced and distributed to younger and younger demographics.
In fact, the ubiquity of technology in modern society has led to the American Academy of Pediatrics adapting its screen-viewing recommendations for children. The guidelines encourage families to identify an appropriate balance between screen viewing and other activities.10Related: How to recognize and manage digital eye strain Cosmetics and the ocular surface
Ubiquitously available and with worldwide self-proclaimed “expert” bloggers, Internet and other informational content, of significant concern to the ocular surface and eyelid margins is the use of cosmetics.
Broadly, the impact of eye cosmetics on the adnexa and ocular surface includes:11
– Increased risk of eye infection
– Toxicity
– Allergy
– Changes in the tear film lipid layer
– Changes to tear stability
– Changes in ocular comfort
– Changes to contact lens wear
– Changes in pigmentation of the conjunctiva and periocular skin
– Masses in the lacrimal system
Note that the law does not require cosmetic products and ingredients-other than color additives-to have FDA approval before they go on the market.
Related: Cosmetic dangers: Part 1-Popular cosmetics patients use
Cosmetic products contain preservatives that include but are not limited to preservatives that include benzalkonium chloride (BAK) and formaldehyde (FA)-releasing preservatives. BAK and FA exert toxic effects on cells of the ocular surface and adnexa.12
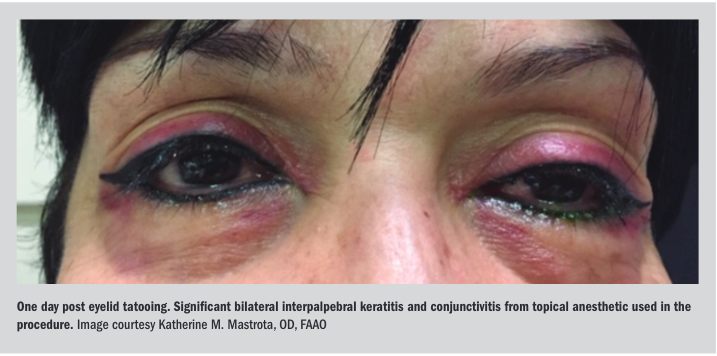
In a similar category is the practice of eyelid tattooing-or cosmetic blepharopigmentation. Tattooing instruments, inks, shields, and guides are deliverable with one click to anyone with an online store account.
Cases of inadvertent corneal pigmentation, limbal and conjunctival pigmentation, full-thickness eyelid penetration during/after the tattooing process have been documented. Lid margin tattooing has been associated with a shortened tear break-up time, increased ocular surface staining, and meibomian gland loss. Post-procedure keratitis related to the tattooing process have been described anecdotally.13-16
Furthermore, tattoo inks may contain heavy metal ingredients that can create artifacts on magnetic resonance imaging (MRI) and/or discomfort, burning sensation, or redness during MRI testing at the lid area of tattoo.17Related: Cosmetic dangers: Part 2-Products banned by the FDA, worsen ocular surface disease
Other tattoo-like procedures include microblading (semi-permanent tattoo using a small blade made up of tiny needles to deposit pigment under the skin) or long-lasting cosmetics designed to pigment the eyelid/eyelid margin area.
Not to be forgotten are eyelash heater curlers, chemical perms (akin to hair permanent curling), and dyes that are documented by the manufacture as toxic or poisonous.
In the quest for eyelash enhancement, eyelash extensions/false eyelashes are posted on multiple information channels including YouTube and beauty blogging sites. Eyelash extensions involve the gluing of fibers (natural or synthetic) to the natural lashes.
Ocular disorders secondary to the eyelash extension process include keratoconjuctivitis from invasion of eyelash glues or removing agents onto the ocular surface, allergic blepharitis due to glues, conjunctival erosions from procedural eye-lid fixing tapes, allergic blepharitis to the eyelid-fixing tape, subconjunctival hemorrhage as well as possible irritation from the formaldehydes and other sensitizing glue ingredients, and bacterial conjunctivitis.18Related: How to educate patients on risks of eyelash enhancements In the air
Finally, challenges to the skin, nasal passages, and ocular surface include those carried in the ambient air.
Allergens; fragrances and chemicals in air sprays and room fresheners/deodorants; and formaldehydes released from personal and homecare products, clothing, building materials, fertilizers, and pesticides can be hidden, potential offenders of the ocular surface.
Dry eye hero
As seen on TV and other information platforms, many of these seemingly harmless products can impact sensitive or at-risk individuals and compound disease management.
Think outside the box. Ask your patients lifestyle, hobby and occupation questions. Be an ocular surface sleuth and a dry eye hero.
Read more dry eye content here
References:
1. Carvalho RS, Kara-José N, Temporini ER, Kara-Junior N, Noma-Campos R. Self-medication: initial treatments used by patients seen in an ophthalmologic emergency room. Clinics (Sao Paulo). 2009;64(8):735-41.
2. Sheppard AL, Wolffsohn JS. Digital eye strain: prevalence, measurement and amelioration. BMJ Open Ophthalmol. 2018 Apr 16;3(1):e000146.
3. Freudenthaler N, Neuf H, Kadner G, Schlote T. Characteristics of spontaneous eyeblink activity during video display terminal use in healthy volunteers. Graefes Arch Clin Exp Ophthalmol. 2003 Nov;241(11):914-20.
4. Patel S, Henderson R, Bradley L, Galloway B, Hunter L. Effect of visual display unit use on blink rate and tear stability. Optom Vis Sci. 1991 Nov;68(11):888-92.
5. Tsubota K, Nakamori K. Dry eyes and video display terminals. N Engl J Med. 1993 Feb 25;328(8):584.
6. eMarketer. Digital set to take majority share in UK time spent with media in 2016. 2016. Available at: https://www.emarketer.com/Article/Digital-Set-Take-Majority-Share-UK-Time-Spent-with-Media-2016/1013039. Accessed 8/29/19.
7. Palaiologou I. Children under five and digital technologies: implications for early years pedagogy. European Early Childhood Edu Res J. 2016;24(1):5-24.
8. Office for National Statistics. Internet users in the UK 2017. 2017. Available at: https://www.ons.gov.uk/businessindustryandtrade/itandinternetindustry/bulletins/internetusers/2017#quality-and-methodology. Accessed 8/29/19.
9. The Vision Council. Digital eye strain. Available at: https://www.thevisioncouncil.org/content/digital-eye-strain. Accessed 8/29/19.
10. Solomon-Moore E, Matthews J, Reid T, Toumpakari Z, Sebire SJ, Thompson JL, Lawlor DA, Jago R. Examining the challenges posed to parents by the contemporary screen environments of children: a qualitative investigation. BMC Pediatr. 2018 Apr 7;18(1):129.
11. Ng A, Evans K, North RV, Jones L, Purslow C. Impact of Eye Cosmetics on the Eye, Adnexa, and Ocular Surface. Eye Contact Lens. 2016 Jul;42(4):211-20.
12. Chen X, Sullivan DA, Sullivan AG, Kam WR, Liu Y. Toxicity of cosmetic preservatives on human ocular surface and adnexal cells. Exp Eye Res. 2018 May;170:188-197.
13. Goldberg H, Berger Y, Ben Bassat I, Barequet I. Inadvertent corneal pigmentation following cosmetic blepharopigmentation. Am J Ophthalmol Case Rep. 2018 Sep 5;12:52-54.
14. Moshirfar M, Espandar L, Kurz C, Mamalis N. Inadvertent pigmentation of the limbus during cosmetic blepharopigmentation. Cornea. 2009 Jul;28(6):712-3.
15. De M, Marshak H, Uzcategui N, Chang E. Full-thickness eyelid penetration during cosmetic blepharopigmentation causing eye injury. J Cosmet Dermatol. 2008 Mar;7(1):35-8.
16. Lee YB, Kim JJ, Hyon JY, Wee WR, Shin YJ. Eyelid Tattooing Induces Meibomian Gland Loss and Tear Film Instability. Cornea. 2015 Jul;34(7):750-5.
17. Tope WD, Shellock FG. Magnetic resonance imaging and permanent cosmetics (tattoos): survey of complications and adverse events. J Magn Reson Imaging. 2002 Feb;15(2):180-4.
18. Amano Y, Sugimoto Y, Sugita M. Ocular disorders due to eyelash extensions. Cornea. 2012 Feb;31(2):121-5.

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.