Use aesthetics to treat lid and periorbital conditions

Technology and innovation has improved many aspects of health care and eye care, including ocular aesthetics. The options at optometrists’ disposal to treat periorbital skin changes are increasingly more effective, more affordable, and more available than ever before.
Let’s take a look at these physiologic changes, what causes them, and how they can be managed.
Related: Embracing aesthetics in optometry Causes of eyelid and periorbital skin damage
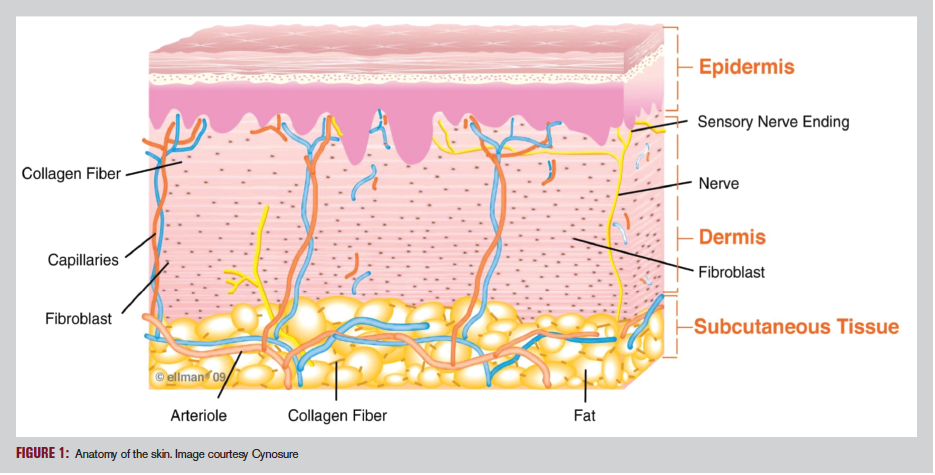
Time, sun, and other environmental factors, including gravity itself, are the mortal enemies of youthful, tight skin. The anatomy of the skin can be simplistically compared to the cornea (see Figure 1).
The epidermis is the relatively thin, superficial skin layer most directly exposed to the environment, similar to the corneal epithelium. The middle skin layer, the dermis, comprises the bulk of the skin’s thickness just as the stroma does in the cornea, while the skin’s subcutaneous tissue (i.e., hypodermis) loosely correlates with the cornea’s endothelium.
Collagen, the main component of connective tissue, comprises about one-third of the total protein content of the body. In the skin, Type I collagen, and to a lesser degree Type III, are present in the dermis and subcutaneous tissue and are responsible skin tautness.1,2
Elastin, on the other hand, is another connective tissue protein present in the body that has rubber-like in consistency. Elastin fibrils slide over one another and recoil, providing elasticity.
Related: Preparing the periocular region for surgery
The aging process reduces collagen production and changes the composition of the collagen that remains, yielding a loss of skin tightness.1,2
As a result:2
• The dermis thins to reveal blood vessels, and melanin levels may increase (which appear as dark circles around the eyes when those vessels dilate)
• The skin sags, and pockets of edema can form, producing “bags” under the eyes (i.e., malar edema)
• Fine lines (e.g. crow’s feet) develop
Damage from the sun’s ultraviolet rays reduces elastin synthesis, which when combined with other environmental and gravitational changes yields loss of skin elasticity (e.g., dermatochalasis) and the formation of deep wrinkles (i.e., rhytids).1,2
What, if anything, can be done?
Related: Blue light: Why it matters Preventive advice for patients
As the old saying goes, “An ounce of prevention is worth a pound of cure.”
Yet sometimes the preventive advice ODs could offer is so obvious that it is easy to overlook. To minimize damage to the periorbital tissue, including the risk of malignancy, ODs should proactively recommend our patients use:
• Sunscreen and other skincare products with sun protection factor (SPF) protection (even on the eyelids) to slow the development of rhytids and dermatochalasis
• Ultraviolet coatings on all clear and sunglass spectacle lenses
• Sunglasses with large eye sizes and/or wraparound designs to maximize protective coverage whenever outdoors
• Polarized sun lenses to reduce squinting and the development of “crows’ feet”
Obviously, even if patients follow these recommendations, clinical signs of damage to the lids and periorbital skin tissue will eventually still develop.
What then?
Related: Vision therapy: A top 10 must-have list Therapeutic options
Numerous in-office therapies and procedures can now be offered to improve the function of the lids and periorbital skin tissue as well as to enhance their aesthetic appearance.
Recommendations, especially for reducing dark circles and bags around the eyes, include:3,4
• Applying cold compresses in the morning
• Suggesting patients ingest caffeine (a vasoconstrictor) in the morning (in moderation because excess caffeine can dehydrate tissue)
• Staying well-rested (seven to nine hours of sleep per night)
• Maintaining proper hydration
• Limiting salt intake
• Avoiding excess alcohol consumption, especially late in the evening
• Treating underlying allergies which can contribute to malar edema
Potentially using over-the-counter creams and lotions containing retinol and/or other appropriate ingredients to remove makeup and to reduce fine lines, rhytids, and malar edema
Related: How to build an eye spa
(Note: There are a multitude of options, but do your research and recommend only those products you are confident have a clinically proven effect; several product lines, such as We Love Eyes and Ocusoft’s Zoria products, can be made available for direct in-office sale)
Several therapeutic procedures are also available for patients.
Related: Top 10 vision therapy books Radiofrequency therapy
Radiofrequency therapy (RF) has been in use in medicine for nearly a century. This technology uses radio waves to selectively warm tissue. Radio waves have an affinity for intracellular water molecules, causing them to vibrate, which produces heat within the cell itself.5
One key consideration is that the tip of the RF probe never gets hot. It is simply a transmitter that emits radio waves into tissue, causing cells to heat from the inside out.
At high frequencies, RF can be used to vaporize the water molecules, causing the cell to lyse and allowing tissue to be incised with a simultaneous hemostatic effect (e.g., essentially bloodless lid lesion removal with an Ellman unit or similar RF device).
Related: How digital devices are affecting vision
In recent years, it was discovered that at lower frequencies RF selectively delivered to the epidermis and dermis to achieve temperatures of approximately 42°C can:5
• Induce collagen denaturation (i.e., contraction)
• Stimulate new collagen synthesis (neocollagenesis)
• Significantly increase the uniformity of elastin
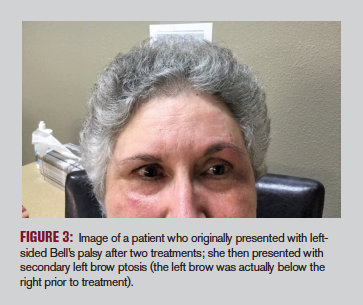
This elective procedure consists of applying an ultrasound gel to the area receiving treatment, activating the RF probe, gently applying the probe to the skin, activating the RF generator, and moving the probe in a corkscrew pattern over the skin while subjectively and objectively monitoring tissue temperature until it reaches ~42°C (Fig. 3).
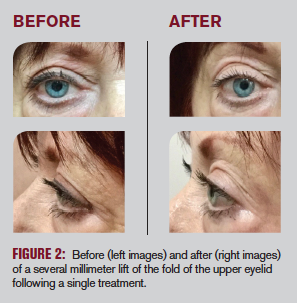
Over the course of the next four weeks post-treatment, rearrangement and reformation of collagen and elastin occurs, resulting in tightening of the skin, reduction of rhytids and malar edema, and even mild-to-moderate elevation (2 to 3 mm) of the upper lids in dermatochalasis.
Usually three to four treatments in total are necessary over a four-to six month period for maximum therapeutic effect, followed by an annual maintenance session. Note that RF is not a replacement for blepharoplasty in moderate-to-severe cases.
Related: The role of lid hygiene in ocular surface disease Intense pulsed light therapy
Intense pulsed light (IPL) therapy (photorejuvenation) has been available for many years as a U.S. Food & Drug Association (FDA)-approved treatment for acne and rosacea. A handpiece emits brief, powerful bursts of light in the 500 to 800 nm range to thermally coagulate cells and produce vascular thrombosis, resulting in decreased hyperemia and reduction of problematic skin flora.
Rolando Toyos, MD, reported that in addition to reducing telangiectasia and enhancing skin appearance, many patients with dry eye syndrome (DES) reported a significant reduction in their symptoms post-IPL.6 Thus IPL is now being used to treat meibomian gland dysfunction (MGD) and DES, in addition to the aesthetic benefits it provides.7,8Related: Understanding intense pulsed light
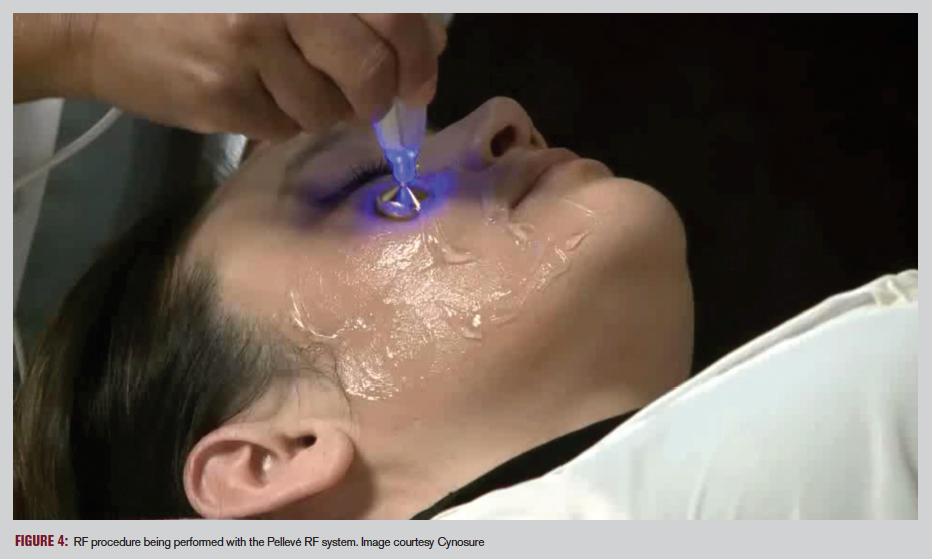
Additionally, as with RF, research using IPL as a therapy for MGD and DES has shown significant efficacy when treatments are applied to the eyelids because the combination of heat and massage is known to help evacuate the meibomian glands. One study found Pellevé RF therapy was equivalent to LipiFlow (Johnson & Johnson Vision) in objective and subjective measures.9Other therapies
For states with broad optometric scopes of practice, aesthetic laser therapies are available, collectively known as laser skin resurfacing, which employ various fragmentation lasers.
Related: How IPL can help dry eye
Additionally, non-invasive, FDA-approved ultrasound technologies are able to eliminate wrinkles and stimulate collagen production.10
On the more invasive front, some states allow doctors of optometry to inject botulinum toxin to smooth and shape the periorbital region, treat essential blepharospasm, and employ commercially available injectable fillers to tighten skin.11
Care should especially be given to appropriately assess patient risk, follow approved protocols, and maximize safe, effective outcomes for all invasive procedures.
Conclusion
Many eyelid and periorbital skin concerns still require an oculoplastics referral, but patients now have more options than ever before at their disposal. More so than in any other area of eye care, dedicated staff and consistent marketing are a must to succeed in any aesthetic endeavor. Fortunately, RF, IPL, laser skin resurfacing, and ultrasound therapies can be performed by a trained technician (most manufacturers provide training and certification), freeing the doctor’s schedule to see other patients.
These therapies can allow a practice to differentiate itself while expanding services and meeting patients’ needs with these private-pay procedures. In states with a more limited scope of practice, check with the state optometry board to insure these arrangements comply with all state statutes and regulations.
As patients continue to seek solutions for these conditions, it is exciting to have these novel therapies available, so consider implementing them as they make sense within individual practices.
Read more by Dr. Wroten
References:
1. Howard D. Structural Changes Associated with Aging Skin. International Derman Institute. Available at: www.dermalinstitute.com/us/library/11_article_Structural_Changes_Associated_with_Aging_Skin.html. Accessed 9/3/19.
2. Cleveland Clinic. Skin. Available at: https://my.clevelandclinic.org/health/articles/10978-skin. Accessed 9/3/19.
3. Fries WC. Solutions for Dark Circles and Puffy Eyes. WebMD. Available at: https://www.webmd.com/beauty/features/eyes-puffy-circles#. Accessed 9/3/19.
4. Lyerly J. Your Eye Doctor’s Guide to Reducing Dark Under Eye Circles. Eyedolatry. Available at: https://www.eyedolatryblog.com/2015/02/your-eye-doctors-guide-to-getting-rid.html. Accessed 9/3/19.
5. Weiss RA. Noninvasive radio frequency for skin tightening and body contouring. Semin Cutan Med Surg. 2013 Mar;32(1):9-17.
6. Toyos R, McGill W, Briscoe D. Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction; a 3-year retrospective study. Photomed Laser Surg. 2015 Jan 1;33(1):41-46.
7. Albietz JM, Schmid KL. Intense pulsed light treatment and meibomian gland expression for moderate to advanced meibomian gland dysfunction. Clin Exp Optom. 2018 Jan;101(1):23-33.
8. Gupta PK, Vora GK, Matossian C, Kim M, Stinnett S. Outcomes of intense pulsed light therapy for treatment of evaporative dry eye disease. Can J Ophthalmol. 2016 Aug;51(4):249-253.
9. Jaccoma EH, Litherland C, Jaccoma A, Ahmed A. A pilot study comparing the efficacy of the Pellevé System to LipiFlow for the treatment of dry eye due to meibomian gland dysfunction. J Dry Eye Ocular Surf Dis. 2018 Mar;1(1): e11-e21.
10. Cleveland Clinic. How Ultrasound Skin Tightening Can Firm, Lift Your Face.Available at: www. https://health.clevelandclinic.org/how-ultrasound-skin-tightening-can-firm-lift-your-face/. Accessed 9/3/19.
11. Becker A. In the Eye of the Beholder: Aesthetic Procedures for the Periocular Area. Rev Optometry. Available at: https://www.reviewofoptometry.com/article/in-the-eye-of-the-beholder-aesthetic-procedures-for-the-periocular-area. Accessed 9/3/19.

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.