Artificial tear ingredients that mimic the real thing
The ones you should seek out—and avoid.
Artificial tears are artificial, with ingredients that aren’t produced by the human body. How can we ensure that patients who need these products get the hydration and protection they need? (Adobe Stock Images/Марина Демешко)

Optimally, artificial tears should be just like natural tears, with aqueous, mucin, and lipid layers functioning together to keep the ocular surface healthy and hydrated. But artificial tears are artificial, with ingredients that aren’t produced by the human body. How can we ensure that patients who need these products get the hydration and protection they need? By looking for ingredients that mimic nature and avoiding the ones that work against it.
Filling the roles of 3 natural tear layers
The aqueous, mucin, and lipid layers of natural tears contain many
substances, including over 2000 nutrients and growth factors not found in artificial tears. However, advanced artificial tears incorporate ingredients that mimic some of the functions of these substances.
Hydrated, protected, and nourished epithelial cells
The aqueous layer provides the hydration that the ocular surface needs. Many artificial tears contain hyaluronic acid (HA), which binds to water to help retainfluid on the surface of the eye. Because HA plays an important role in inflammatory regulation, wound healing, and cellular regeneration,1 it promotes epithelial cell health. A relatively new ingredient in lubricating eye drops is trehalose, available in iVIZIA (Théa) and TheraTears EXTRA (TheraTears). Trehalose acts as a bioprotectant for the cornea’s epithelial cells.2
Figure.Superficial punctate keratitis due to dry eye disease (Image courtesy of Cecelia Koetting, OD, FAAO, Dipl ABO)
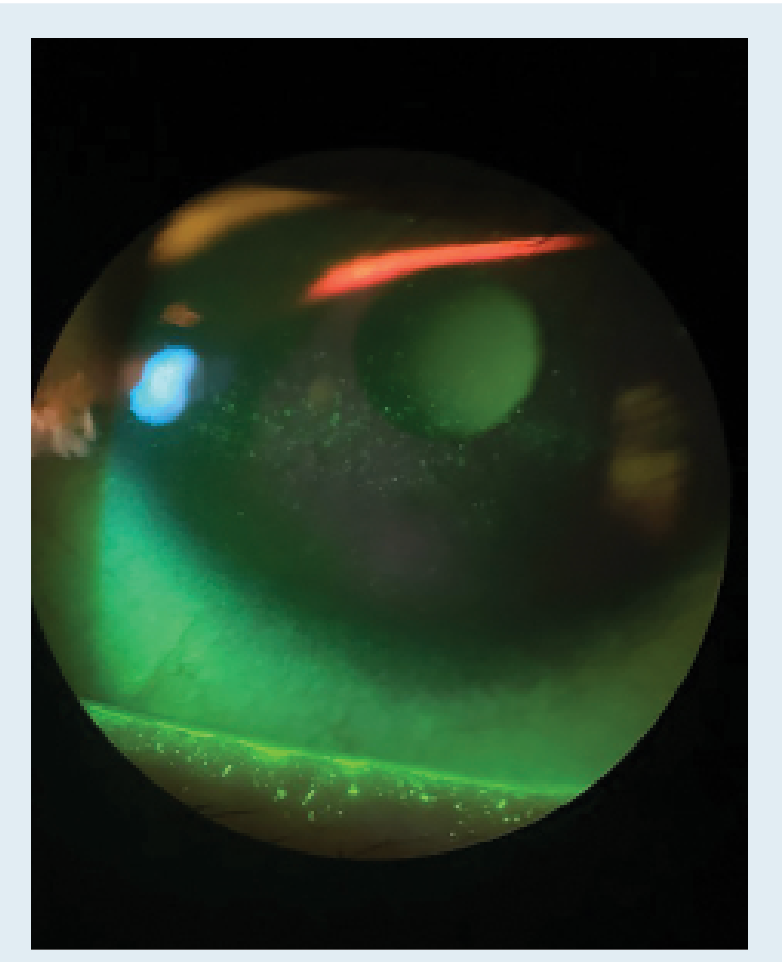
In a hyperosmotic situation, epithelial cells desiccate, atrophy, and die, resulting in superficial punctate keratopathy (SPK) and staining. Trehalose, a disaccharide produced by some plants in response to environmental stress, preserves cells so they can recover when conditions improve. For instance, the plant known as the rose of Jericho, which produces trehalose, can remain dry for years during droughts and recover when water becomes available again. The idea of adding trehalose to artificial tears is to potentially convey the same kind of stabilizing protection to epithelial cells. Studies have shown that compared to HA alone, HA and trehalose together boost tear film thickness leading to an increase in tear break up time and leads to a lower self reported symptom score on the OSDI questionnaire.3,4
Tear retention on the eye
The mucinlayer in natural tears performs many functions, including making tears “sticky” so they remain on the eye.The HA in artificial tears helps them do the same thing by binding to water. Other components found in artificial tears such aswater-soluble polymers like carboxymethylcellulose and povidone form a protective matrix over the eye. This helps with shielding and lubricating the mucus membrane while reducing viscosity and increasing stickiness, all of which increases the drop’s longevity on the ocular surface.
A healthy rate of evaporation
The lipid layer of natural tears slows evaporation of the aqueous layer but is often of poor quality in patients with ocular surface disease. Some artificial tears contain emollients to replace natural lipids. Early lipid-containing formulations caused blurriness and separated in the bottle. Today, the
technology is much better; nanoparticles of oil are distributed throughout
the drop, causing less blurring and visual fluctuation.
Ingredients to avoid
In the search for ocular homeostasis, it is equally important to avoid chemicals that damage the ocular surface and worsen dry eye. Unfortunately, the eye drop aisles of supermarkets and pharmacies are filled with an overwhelming amount of options, many containing these harmful additives. By recommending a specific drop rather than allowing patients to shop around, we can help them avoid some of these ingredients.
Vasoconstrictors
Ingredients like naphazoline and tetrahydrozoline provide temporary reduction in redness by constricting blood vessels on the ocular surface. When the drops wear off, rebound redness occurs and the drop must be reapplied. Prolonged use of vasoconstrictors is problematic because ocular surface cells rely on blood circulation for health and healing.
BAK preservative
Most artificial tears contain a preservative. The most common one is benzalkonium chloride (BAK), which can weaken epithelial cells and cause ocular surface toxicity, worsening the very problem we’re trying to treat.5 In small doses, BAK may not cause problems, but chronic use can lead to complications, and some patients are sensitive to any amount of BAK. Other preservatives such as polyquaternium-1 have less potential for harm, but I recommend unpreserved tears for patients who use them every day.
Detrimental “natural” ingredients
In my experience, certain natural ingredients are added to artificial tears with little thought to their effects. A few homeopathic formulations contain belladonna, a toxic plant that dilates the pupil, affecting vision. Another brand touts that it produces a cooling effect, which it achieves with menthol. When the goal is comfort and homeostasis, it’s best to stick to formulations without unproven or irritating ingredients, even if they’re described as being natural.
Case study: Fewer flares with HA/trehalose drops
A 52-year-old office manager who works constantly on the computer came to me for a second opinion about her dry eye disease, which she could not control with over-the-counter artificial tears and eyelid cleansing wipes. She described constant tearing and foreign body sensation with some itching, noting worsening of symptoms with seasonal changes that were likely related to her systemic allergies. On exam, she had blepharitis debris on her lids, grade 1 Meibomian gland dysfunction with turbid expression, no current papillae, and grade 1 corneal SPK staining.
A the time, iVIZIA HA/trehalose artificial tears had just become available in the US. I recommended that she use both the drops and the cleansing wipes twice a day. She also began taking omega 3 supplements and using a heat mask at night for 10 minutes followed by a lid massage prior to bed.

At her 6-week follow up, the patient said that her symptoms had calmed down and she had improved. The iVIZIA wipes were the first she had found that had not caused further irritation, and the tears were more soothing than others she had tried. Clinically, she had improved as well: no debris on the lids, clear Meibomian gland expression, and no corneal staining. Those minor changes made a huge difference to her quality of life and made working all day on the computer significantly less difficult. The combination of iVIZIA
products and other therapies tipped back the scale for this patient, and has done so for many others in my clinic.
In cases like this, recommending good-quality artificial tear drops containing the right ingredients can make a bigger difference than we might think. When a patient experiences worsening symptoms or is not quite controlled on medication, I add a quality HA/trehalose tear to improve results, and I get a great response.
References
1. Litwiniuk M, Krejner A, Grzela T, et al. Hyaluronic acid in inflammation and tissue regeneration. Wounds. 2016;28(3):78-88.
2. Ozek D, Kemer OE. Effect of the bioprotectant agent trehalose on corneal epithelial healing after corneal cross-linking for keratoconus. Arq Bras Oftalmol. 2018;81(6):505-509. doi:10.5935/0004-2749.20180100
3. Schmidl D, Schmetterer L, Witkowska KJ, et al. Tear film thickness after treatment with artificial tears in patients with moderate dry eye disease. Cornea. 2015 Apr;34(4):421-426. doi:10.1097/ICO.0000000000000358
4. Fondi K, Wozniak PA, Schmidl D, et al. Effect of hyaluronic acid/trehalose in two different formulations on signs and symptoms in patients with moderate to severe dry eye disease. J Ophthalmol. 2018:4691417. doi:10.1155/2018/4691417
5. Datta S, Baudouin C, Brignole-Baudouin F, et al. The eye drop preservative benzalkonium chloride potently induces mitochondrial dysfunction and preferentially affects LHON mutant cells. Invest Ophthalmol Vis Sci. 2017;58(4):2406-2412. doi:10.1167/iovs.16-20903

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.