Case study: Vascular abnormality diagnosed as arteriovenous malformations of the iris
Determining diagnosis, prognosis, and whether referral for more specialized care is needed.

This case study involves a diagnosis of arteriovenous (AV) malformations of the iris. Evaluation warranted dilation of the pupil, thorough retinal examination, and visualization of the posterior side of the iris. Because the abnormal iris vasculature may not be the primary site of the abnormality in question, careful examination of the conjunctival vasculature is also needed.
Vascular abnormalities of the iris and ciliary body can take on an impressive appearance, or they can be very subtle and easily missed. In addition, they can present a diagnostic quandary if they are difficult to visualize or extend or arise from the posterior segment side of the iris.
A patient presented recently with a vascular abnormality which caused me to pause and investigate further in order to sort out a diagnosis, prognosis, and the need (or lack thereof) for a referral for more specialized care.
Related: Update on iris melanoma
Case presentation
A 59-year-old Caucasian female was referred for a comprehensive eye examination as per a recent diagnosis of type 2 diabetes mellitus. She had no complaints and wore reading glasses as needed. Medical history was remarkable for systemic hypertension, type 2 diabetes mellitus, and high cholesterol. Her medications included hydrochlorothiazide and a generic statin.
She was newly diagnosed with diabetes; she was not yet prescribed anything for glucose control and was working on dietary changes. Family history was remarkable for diabetes, systemic hypertension, and cataracts. She also had an uncle who was blind in one eye, but she did not know why.
Entering unaided distance visual acuities were 20/25 in the right eye and 20/20-2 in the left eye. Pupil function was normal in each eye, and extraocular muscle function was unremarkable for each eye. Confrontation visual field assessment showed frankly full visual fields for each eye, and intraocular pressure (IOP) assessment by means of rebound tonometry was 17 mm Hg in the right eye and 19 mm Hg in the left eye. The patient was found to have a low amount of astigmatism in each eye with best-corrected visual acuities of 20/20 in each eye.
Related: 10 new treatments in eye care
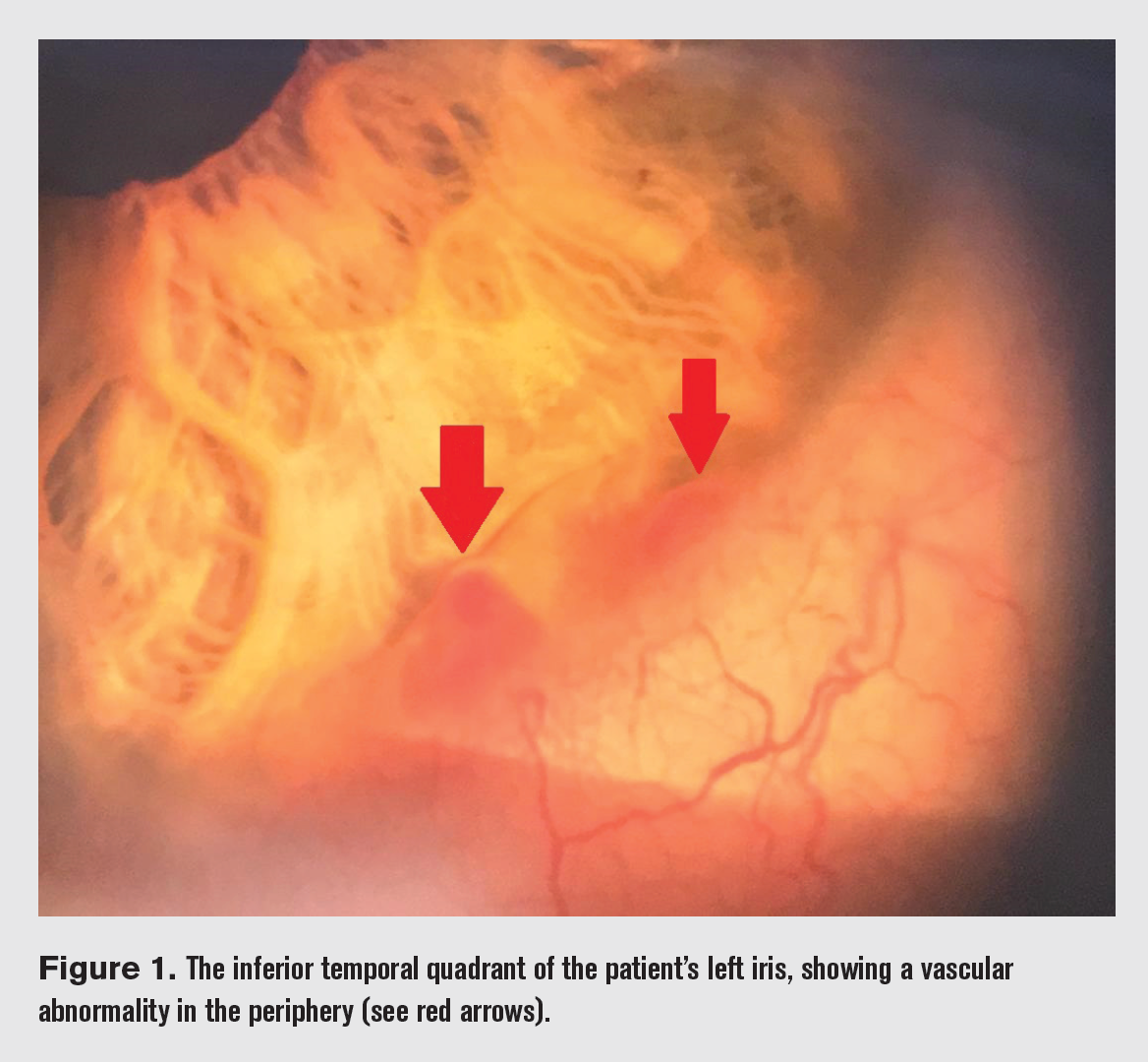
Anterior segment examination of the right eye showed unremarkable lids and lashes, open anterior chamber angles, a clear cornea, quiet conjunctivae, and a quiet anterior chamber with an iris of normal architecture. Examination of the left anterior chamber was essentially the same except for a prominent vascular abnormality of the iris at the inferior temporal aspect of the limbus (Figure 1).
The examination of this abnormality under high magnification via slit lamp yielded no additional information. I also viewed the patient’s anterior chamber angles by means of gonioscopy, and no other abnormalities were noted. The abnormal blood vessel did not appear to extend further into the angle when viewed in this fashion. There were no signs of vascular compromise, such as hemorrhaging.
Related: Use dark adaptation to screen before multifocal IOL implantation
The patient did not recall being told of any iris abnormalities in the past, and her last eye exam was reportedly about 5 or 6 years prior.
The patient was dilated with 1% tropicamide and 2.5% phenylephrine. While the patient was dilating, I researched this finding by consulting my Atlas of Eye Disease and performing a search of the world’s peer-reviewed literature.
Posterior segment examination showed healthy and dry retinas with healthy and perfused optic nerves. The patient was phakic with a trace amount of nuclear sclerosis in each eye. A three-mirror contact lens was used to better visualize the peripheral retina to the ora serrata in the left eye, and no abnormalities were seen. By this method, the posterior aspect of the iris was unremarkable to the extent to which it was seen.
Spectral domain optical coherence tomography (OCT) studies of the left iris and angle showed no other corresponding abnormalities. As it approached the angle, the iris was flat on each side.
In addition, B-scan ultrasound was unremarkable. Anterior segment photography of the abnormality was saved in the patient’s record, and this will be repeated at a follow-up visit.
Related: Retinal detachment seals itself
Diagnosis
Based on the clinical presentation and lack of associated abnormal findings, the patient was diagnosed with an arteriovenous (AV) malformation of the left iris. The exact origin of this malformation was frankly unclear, but the iris was the only tissue with which it was in overt correspondence. AV malformations of the iris appear to be relatively benign findings, with the affected blood vessels exhibiting essentially normal function.1 There are also no apparent systemic associations.1
The patient was advised to call immediately if she experienced a sudden loss of vision and/or eye pain, which could be a sign of a hemorrhage into the anterior chamber-although the risk for such is likely very low. She was invited to return in 4 to 6 months for a follow-up examination and will be examined annually after that if all findings are stable.
Conclusion
Evaluation of such an abnormality of the iris warrants dilation of the pupil, thorough retinal examination, and visualization of the posterior side of the iris to check for related findings to include a malignancy of the iris or adjacent tissue.
A careful examination of the conjunctival vasculature is also warranted, in keeping with the notion that the abnormal iris vasculature may not be the primary site of the abnormality in question.
More by Dr. Casella: Coats’ disease: A case study of a 4-year old boy
References:
1. Shields JA, Streicher TF, Spirkova JH, Stubna M, Shields CL. Arteriovenous malformation of the iris in 14 cases. Arch Ophthalmol. 2006 Mar;124(3):370-5.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.