Misdiagnosis when clinical findings don’t make sense
Case exhibits challenge of “atypical” disease presentation and potential for unneeded surgery.
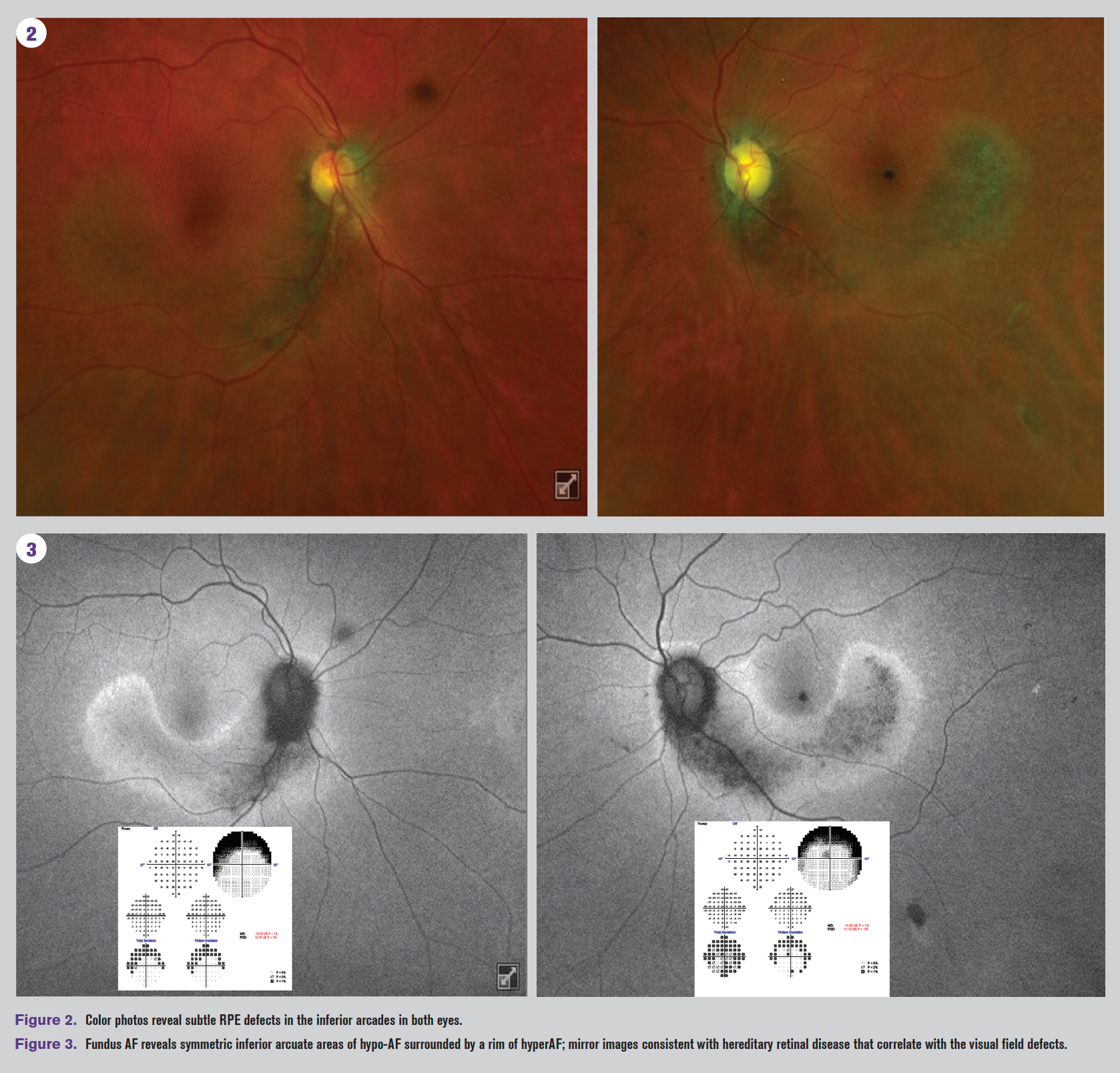
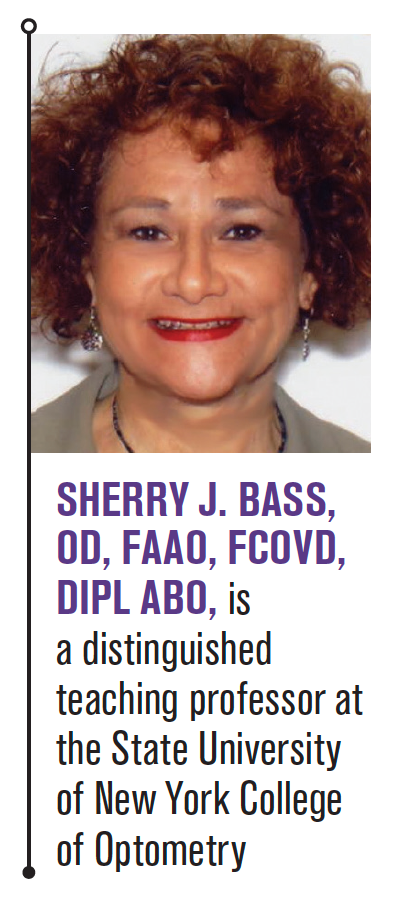
Figure 1
In this case example, a patient was originally misdiagnosed with progressive glaucoma based on progressing superior field loss. However, subsequent testing showed that structural findings did not match functional findings. Fundus autofluorescence imaging prompted a new diagnosis of sector retinitis pigmentosa. The patient had already undergone trabeculectomy OS and was almost scheduled for a trabeculectomy OD.
A mentor once taught me that 95 percent of treatment is making the right diagnosis. Once the proper diagnosis is made, the treatment can easily be obtained by referring to a vast wealth of publications and internet sources or referring the patient to the proper specialist.
An “atypical” case of misdiagnosis is presented here. The patient, now middle-aged, had a misdiagnosed eye disease that almost resulted in unnecessary surgery.
Related: Unconventional clinical options for lowering IOP
Case presentation
A 67-year-old black female with a history of uncontrolled primary open-angle glaucoma (POAG), greater in the left eye, presented for a follow-up examination. She was on maximum medications and had undergone selective laser trabeculoplasty in both eyes and a trabeculectomy in the left eye. She was urged at multiple visits over the past year to undergo trabeculectomy in the right eye as well. The concern was that the patient’s glaucoma was progressing based on the visual field loss despite medical and surgical interventions and despite the fact that intraocular pressures (IOP) were maintained in the mid-teens.
The patient had severe (dense) arcuate superior field loss OU (Figure 1 left and middle). At her last follow-up visit, it was noted that the optical coherence tomography (OCT) of the retinal nerve fiber layer (RNFL) findings did not correlate with the visual field findings (Figure 1 far right). Regardless, the patient was referred for a trabeculectomy consult in the right eye.
Related: New guidelines out for diabetes patient care
The patient returned two months later for the trabeculectomy consult with the glaucoma specialist who agreed that the visual fields did not fully correlate to the OCT or to the optic nerve head appearance. It was thought that the dense superior arcuate visual field loss in both eyes may have been due to extensive peripapillary atrophy. No additional treatment was advised, and the patient was referred for a retinal evaluation to determine possible retinal etiology of the progressing arcuate superior field defects in both eyes.
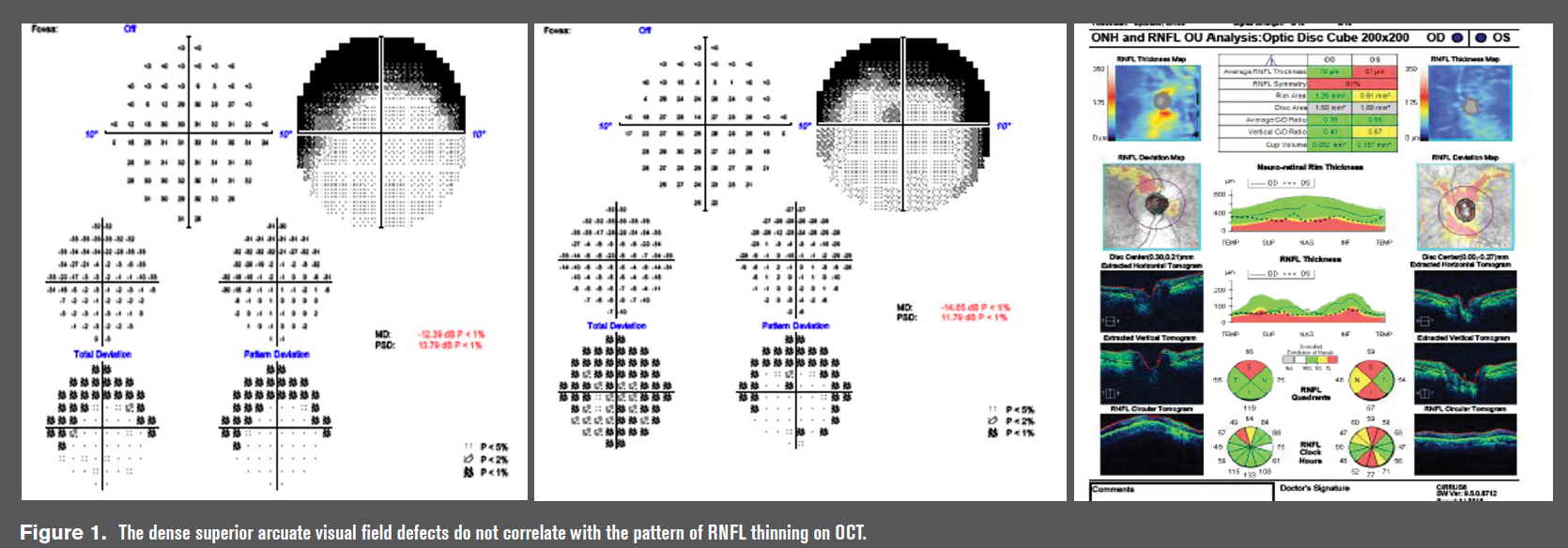
Examination of the retina revealed subtle retinal pigmentary changes in the inferior arcuate region in both eyes (Figure 2). Fundus autofluorescence (AF), on the other hand, revealed more obvious bilateral, symmetric inferior arcuate areas of hypo-AF in both eyes surrounded by hyper-AF abnormalities (Figure 3).
Related: Spiking IOP not what I thought
Diagnosis
Based on the AF appearance, the patient was diagnosed with sector retinitis pigmentosa (RP), a type of regional retinal degeneration in which the patient is asymptomatic because a small portion of the retinas are affected and the visual field loss is superior. Superior field loss is often unnoticed by patients compared to inferior field loss.
This patient was originally misdiagnosed with progressive glaucoma based on the progressing superior field loss. The patient already underwent trabeculectomy in the left eye and was almost scheduled for a trabeculectomy in the right eye.
Discussion
This case underlines the importance of ascertaining that the structural findings (in this case RNFL thinning) match the functional findings (visual field loss). Closer examination of the RNFL thinning pattern reveals superior thinning OU and inferior thinning only OS. Yet the visual field defects are symmetric and dense. The superior arcuate visual field defects can be explained on the basis of the inferior arcuate retinal defects caused by the sectoral RP.
The combination of two diseases which can both cause visual field loss makes the glaucoma more challenging to treat. In another reported case, a patient was misdiagnosed as having POAG on the basis of the arcuate field loss when in fact the patient had RP.1
Related: How to manage the angle closure spectrum
One must determine, if possible, which disease is responsible for the progressing field loss. There are two ways of differentiating the etiology of the progressive field loss.
First, visual field loss in photoreceptor degenerative diseases like RP is symmetric and very dense because early retinal thinning affects the outer retina. Glaucomatous field loss, on the other hand, is usually relative in the early and moderate stages of the disease and asymmetric.
Second, the RNFL in RP is usually thicker than normal and is not affected until the end stage of the disease. On the other hand, glaucoma affects the RNFL early in the disease.
Also important to note: The ganglion cell analysis (GCA) will be abnormal in retinal degenerative diseases. The reason for this is not well understood, but if one is following glaucoma in a patient with a hereditary retinal degeneration like RP, it is important to know that the GCA will be abnormal in both diseases and cannot be used to differentiate the two.
In summary, misdiagnosis can delay treatment or can result in inappropriate treatment. In our haste to diagnose patients, errors can be made that have the potential to result in further harm to the patient. Clinicians need to be alert when diagnosing “atypical” presentations of disease without further investigation or when results from various tests don’t make sense.
Acknowledgement: The author would like to thank Kim Poirier-Schmidt, OD, for sharing this case.
Related: Know what common glaucoma mistakes to avoid
References:
1. Lin J, Vander JF, Martin M, Katz LJ. Atypical retinitis pigmentosa masquerading as primary open angle glaucoma. J Glaucoma. 2007 Mar;16(2):268-70.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.