Digital health care in optometry
Embracing this new model of care can allow optometric practices to flourish—and may enable earlier detection of conversion from intermediate dry to wet AMD.
Optometry has been skeptical of digital eye care models that have burst onto the scene during the past decade. This skepticism, rooted in the reality that online spectacle and contact lens sellers ate into the retail revenues of optometric practices, may indeed be justified for technology services offering digital eye care such as online refractions.
And it may be reinforced by concerns that such eye care services are fundamentally unable to match the quality of in-person interaction, examination, and evaluation.
However, digital health care models present an opportunity to increase the reach and services of a practice in a way that some digital eye care models have not.
By viewing digital health care as a series of adjunctive tools that supplement—rather than replace—a clinician’s expertise, optometrists might reframe their thinking of digital health care as a structure to be embraced instead of a threat to be mitigated.
Further, by adopting digital health care models as part of a practice paradigm, optometrists can increase their reputation in their local market, differentiate themselves from the competition, and provide a uniquely high level of care—all without relying on heavy capital investments that could take years to recoup.
Embracing digital health care may be especially effective in caring for patients with potentially vision-threatening retinal disease.
Related: Top digital resources for prescribing
Given that retinal disease requires treatment that may only be administered in an ophthalmic practice, optometrists (ODs) are left with little opportunity to engage with these patients upon referral.
The use of home-based digital health care platforms such as the ForeseeHome AMD Monitoring Program (Notal Vision) could be key to expanding an optometric clinic’s offerings in the retina space.
By empowering ODs to catch the conversion of dry to wet age-related macular degeneration (AMD) early, a monitoring platform allows ODs—commonly called the gatekeepers of eye care—to be instrumental in timely intervention.
Digital health care in optometry
A number of digital health care platforms have been shown to be effective at monitoring ocular diseases while being user friendly, resulting in high degrees of patient satisfaction.
For example, iCare Home (iCare Inc), a home tonometer used by patients with glaucoma to track diurnal intraocular pressure (IOP), was shown to “reliably [detect] therapy-related IOP changes in patients with glaucoma and ocular hypertension” in a pivotal study.1
Additional research has shown that patients find the device intuitive, real-world patients are able to accurately gather IOP data with the device, and 89% of patients would recommend the device to other patients with glaucoma.2
Related: Addressing the need for greater access in vision care
iCare Home highlights a home-based hardware solution. For a software solution, consider the various platforms that exercise artificial intelligence (AI) and machine learning for the detection of diabetic retinopathy.
Patients with diabetes who submit to fundus photography may have their imaging results reviewed by AI, which then identifies any evidence of diabetic retinopathy and, if found, classifies its severity.
This AI-based interpretation of images has been shown to be an effective method for screening patients with diabetes, especially among large populations.3
Although this software-based system requires that patients visit a clinic, removing the convenience of home monitoring via a device like iCare Home, it clearly illustrates the value of AI-based monitoring systems for detecting ocular pathology.
The ForeseeHome AMD Monitoring Program includes a physical device patients use at home, which utilizes AI, and results are automatically transmitted to the Notal Vision Monitoring Center.
Thus, it is a marriage of home-based hardware and AI innovations. By enrolling patients in home monitoring, earlier detection of conversion from intermediate dry to wet AMD may be achieved.
Patients actively engaged in home-based monitoring remain in the orbit of an optometry clinic, allowing a brick-and-mortar practice’s reach to expand beyond the borders of its physical location.
Related: Adopting new technology without sacrificing practice space
If routine testing indicates that a patient may have converted to wet AMD, the prescribing practice is alerted that an in-person examination may be warranted, thereby strengthening the patient-clinician relationship rather than replacing it.
Home-based AMD monitoring
Patients with intermediate dry AMD and best-corrected visual acuity (VA) of 20/60 or better are eligible for referral to the ForeseeHome AMD Monitoring Program, with the majority of patients’ costs covered by Medicare because the device is FDA approved.
The Notal Vision Monitoring Center assists the patient in setting up the platform and walks the patient through the steps of routine testing, taking any burden for patient support off the referring optometric practice.
Moreover, the center monitors patient compliance (contacting the patient if compliance has dropped off and troubleshooting technology issues in real time) and analyzes patient testing results via an AI algorithm.
If AI concludes that an aberration from baseline (and a possible conversion from intermediate dry to wet AMD) has occurred, the software’s determination is checked by in-house medical professionals before the patient’s clinic is contacted.
If the in-house clinician agrees with the AI’s interpretation, Notal Vision Monitoring Center contacts the prescribing provider, who then determines whether and how to contact the patient for a clinical examination.
Related: Viewpoints: Remote monitoring centers for dry AMD
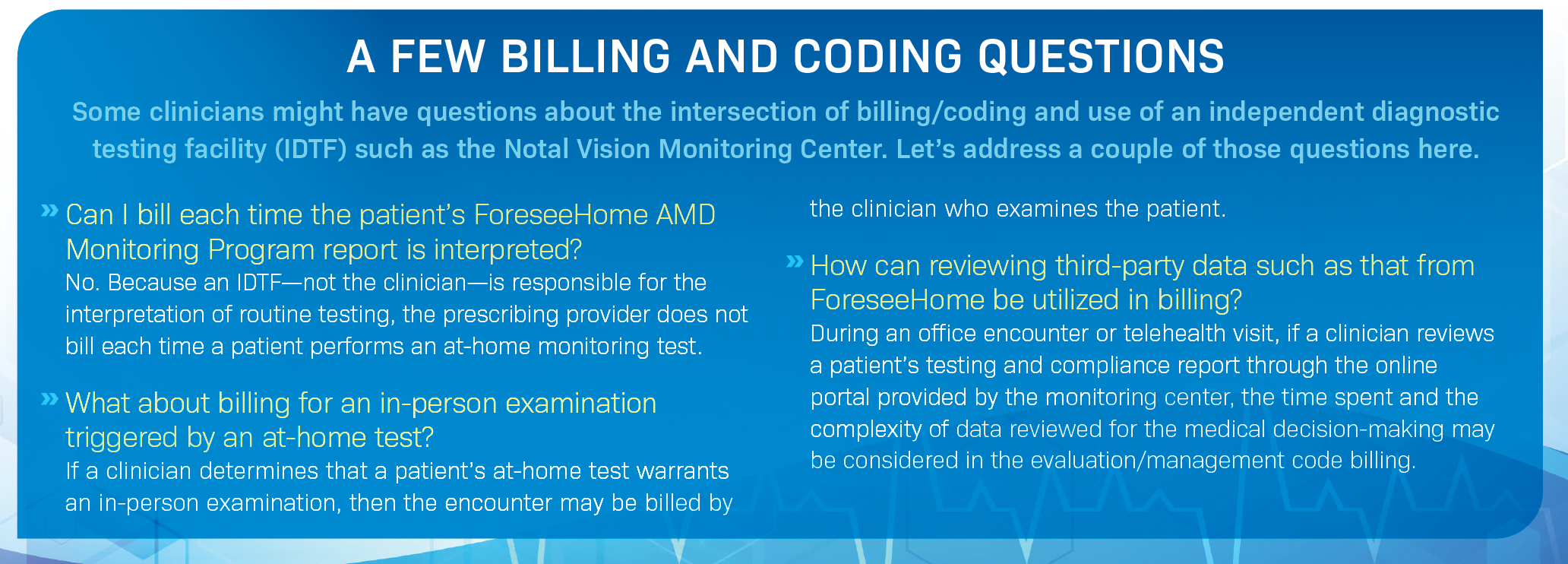
It should be emphasized that prescribing home-based monitoring for AMD conversion requires neither a cash investment by the prescribing physician nor a time investment to set up the device in the patient’s home, troubleshoot hardware issues, or review daily tests. For information on billing and coding, see the sidebar, “A few billing and coding questions.”
The value of early detection
Two recent contributions to the literature illustrate the importance of detecting and treating wet AMD early, which can be accomplished more effectively in patients who undergo at-home monitoring
A 2020 retrospective study that reviewed real-world patients diagnosed with wet AMD found that patients with at least 20/40 VA at baseline maintained a mean VA of 20/40 or better after year 1 and year 2 of treatment with anti-VEGF therapy.4
Among this same population, patients who presented with baseline VA worse than 20/40—approximately 66% of the real-world patients in the study—were not able to achieve mean VA of 20/40 or better at year 1 or year 2.
With these data in mind, it becomes clear that early detection of wet AMD conversion, which allows early intervention, is key to maintaining patients’ visual function.
Related: Case report: the “other” AMD
In 2021, researchers reviewed data from real-world patients enrolled in a regimen that included both in-person examination at a clinical practice and home-based monitoring via the ForeseeHome AMD Monitoring Program.5
All patients in the study had at least 20/60 VA at the time home monitoring was prescribed. In total, 306 patients in the study converted from intermediate dry to wet AMD, 69% of whom had their conversion detected by the Notal Vision Monitoring Center.
Note that patients in this 2021 study were not prescribed only home monitoring; rather, the hybrid regimen required in-person and at-home monitoring.
Use of the ForeseeHome AMD Monitoring Program allowed the clinic to provide constant monitoring services while still preserving (as opposed to replacing) the clinician-patient relationship through regular in-office encounters.
Retention of patients with dry AMD to the point of conversion to wet disease provides additional opportunities for diagnostic imaging with fundus cameras and optical coherence tomography devices.
Practice growth via technology
Although not all technologic advances will result in practice growth, select services will expand the reach of a practice and improve patient care while strengthening the relationship a clinic has with its patients.
By framing a platform as a digital health care service that practices can offer to patients, such technology can be viewed as an asset—rather than a threat—to the financial integrity of clinics and elevate optometry to a new level of care. Clinicians may wish to adopt these technologies as their practices evolve.
References
1. Scott AT, Kanaster K, Kaizer AM, et al. The utility of iCare Home tonometry for detection of therapy-related intraocular pressure changes in glaucoma and ocular hypertension. Ophthalmol Glaucoma. 2022;5(1):85-93. doi:10.1016/j.ogla.2021.05.007
2. Ogle JJ, Soo Hoo WC, Chua CH, Yip LWL. Accuracy and reliability of self-measured intraocular pressure in glaucoma patients using the iCare Home tonometer. J Glaucoma. 2021;30(12):1027-1032. doi:10.1097/IJG.0000000000001945
3. Pei X, Yao X, Yang Y, et al. Efficacy of artificial intelligence-based screening for diabetic retinopathy in type 2 diabetes mellitus patients. Diabetes Res Clin Pract. 2022;184:109190. doi:10.1016/j.diabres.2022.109190
4. Ho AC, Kleinman DM, Lum FC, et al. Baseline visual acuity at wet AMD diagnosis predicts long-term vision outcomes: an analysis of the IRIS registry. Ophthalmic Surg Lasers Imaging Retina. 2020;51(11):633-639. doi:10.3928/23258160-20201104-05
5. Ho AC, Heier JS, Holekamp NM, et al. Real-world performance of a self-operated home monitoring system for early detection of neovascular age-related macular degeneration. J Clin Med. 2021;10(7):1355. doi:10.3390/jcm10071355

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.