Peripupillary prognosticators of glaucoma
Examine the anterior segment for risk factor identification and early diagnosis.
As primary eye care practitioners, we acutely know how essential early detection, treatment, and management of glaucoma can be for best maintenance of vision in our patients.
We also know that, as of summer 2021, 3 million Americans older than 40 years were living with glaucoma—and that counts only those who were already diagnosed.1
We also know that not every patient’s diagnosis is caught early on. This translates to innumerable opportunities for us to drive timely diagnosis and save vision.

Typically, our go-to routine for ruling glaucoma in or out is a combination of an intraocular pressure (IOP) check and visualization of the nerve.
Related: Glaucoma: More pressures than meet the eye
Both are helpful and can reveal a great deal about patients’ glaucoma status. However, we can also get a peek into their risk factors from their anterior segment—specifically, the peripupillary findings.
Peripupillary viewing
Examination of the peripupillary area is unique because it is one of the only structures (to use that term loosely) that can be visualized both by direct viewing outside and using the slit lamp as well as by retroillumination.
Both can reveal unique preglaucomatous findings that might steer us toward more careful examination.
Direct viewing of the peripupillary area can be done externally from the slit lamp, using a penlight, indirect light, or any similar bright light source. Beginning with the basics, not only are we looking for afferent pupillary defects comparatively between the eyes, but we are also analyzing each individual pupil for shape and size.
Irregular shape on a still motile pupil can alert a practitioner to the potential for posterior synechiae—or a partial adhesion—between either the iris and the lens or the iris and the intraocular (IOL) implant.
This is sometimes indicative of a previous inflammatory event, traumatic or otherwise. The incidence of glaucoma after an inflammatory event (uveitis)—regardless of which type of uveitis—is 7% to 11%, and that risk increases with time.2
If the pupil appears quite small and entirely nonmotile, it could be an indication of a posterior synechiae around the entire pupil (360) or iris bombé, which could show that it is aqueous and has been prevented from flowing to the anterior chamber, with a secondary glaucoma invariably following.3
Related: Pearls on diagnosing and managing glaucoma for optometrists
The iris bombé malformation can be better appreciated on slit lamp, with an anterior bowing of the middle of the iris. Taking those extra few milliseconds to examine the shape and motility can be vital.
Analysis
After examining the pupils from afar, slit-lamp analysis will give more information. The integrity of the pupillary ruff presents a vital peek into potentially glaucomatous eyes. It has been found that pupillary ruff changes; its absence, mostly, and irregularity between the eyes are predictive of IOP.4
To clarify: The eye with more pupillary ruff loss is more likely to have a larger cup-to-disc ratio and higher IOP.
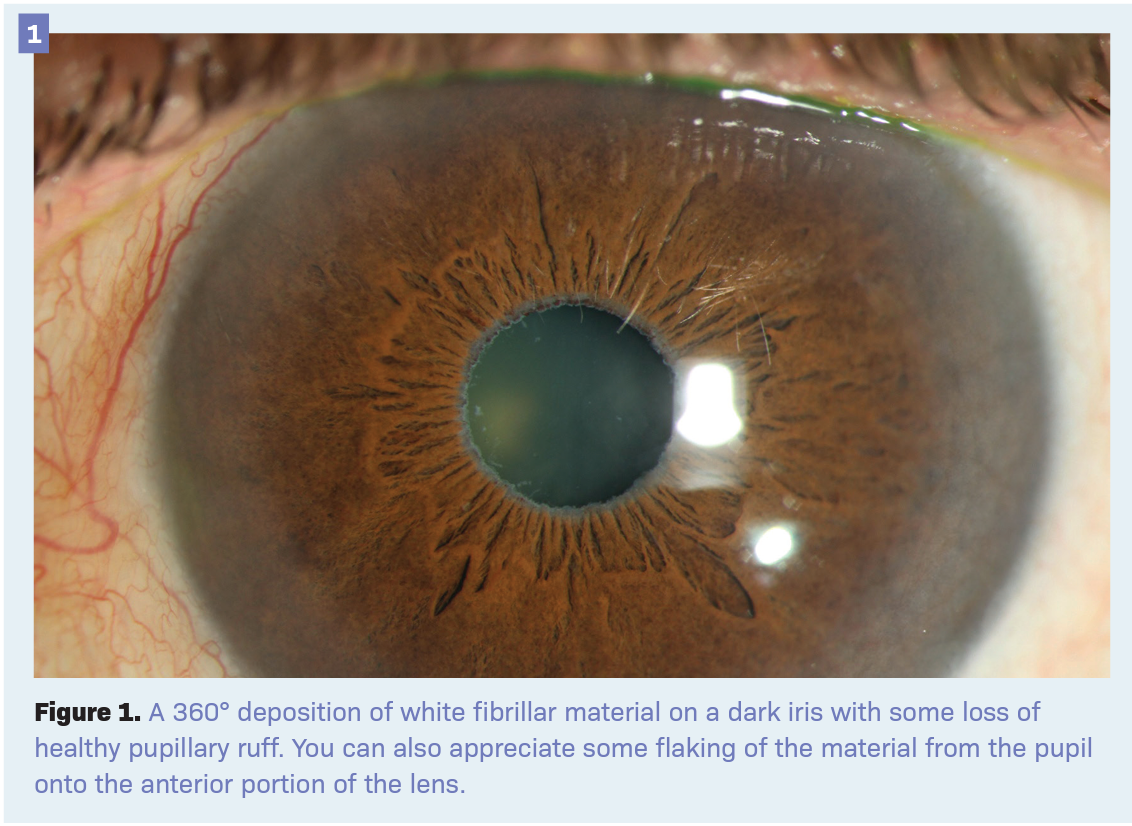
Pseudoexfoliative material around the pupillary border is well known—but not always easy to spot. Often appearing white and believed to be amyloid and/or fibrillarlike material, it can be more challenging over a light-colored iris and more obvious on a dark.5
See Figure 1 for a 360° deposition of white fibrillar material on a dark iris with some loss of healthy pupillary ruff. You can also appreciate some flaking of the material from the pupil onto the anterior portion of the lens.
Approximately 20% of patients with newly diagnosed pseudoexfoliative syndrome have either glaucoma or increased IOP.6
Overall, 50% of patients with pseudoexfoliation syndrome are ultimately diagnosed with glaucoma.6 Taking an extra few moments during the exam to scan the peripupillary ruff can be of paramount importance.
Retroillumination
After completing the slit-lamp examination of the anterior segment, it is tempting to instantly lift the fundoscopy lens and push through to view the posterior pole.
Although this is an important step, first take a pause: A direct slit-lamp beam shone through the pupil, gifting us a retroilluminated view, can provide a great deal of information.
Related: Preserving the ocular surface in glaucoma patients
The red reflex and reflection from the retina can be used to highlight opacities and defects in both the iris and the lens.
The most well-known retroilluminated view is the classic radial pattern of pigmentary dispersion ring changes in the iris midline via transillumination defects, the presence of which indicates approximately a 15% chance of conversion to glaucoma.7
That same iris from Figure 1, with pseudoexfoliative changes, just may have a peripupillary transillumination from the atrophy of the pupillary ruff. You might also be able to see the flaked fibrillar material on the natural lens retroilluminated as an opacity, which can sometimes be difficult to appreciate from a direct view.
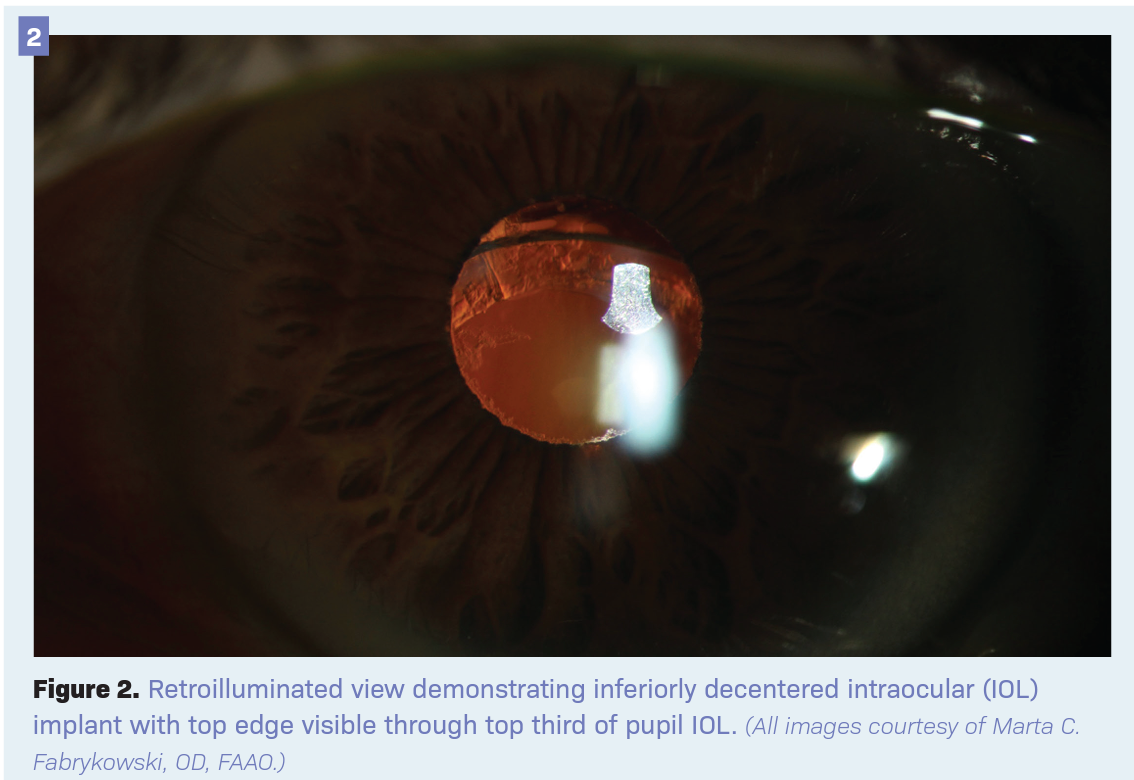
A peripupillary retroilluminated view can also divulge great information on the integrity of the lens, natural or implant.
With a direct view, we can sometimes assume that the lens, a fairly clear structure, is in place; however, it can be bowed so posteriorly or inferiorly that we are not able to see it.
In Figure 2, a retroilluminated view demonstrates an inferiorly decentered IOL implant, with the top edge visible through the top third of the pupil.
The center of the pupil houses a clear portion of the IOL, which would give a fairly decent quality view through the pupil and might not flag that the patient has a decentered lens in direct light.
Related: Case report: 16-year-old presents with asymptomatic glaucoma
It is unknown what the true probability is of lens decentration—and subsequent risk of glaucoma—but in some sulcus-placed IOLs, decentration was as high as 14% and glaucoma as high as 6%.8
Although they paint an incomplete picture, these statistics highlight the need to examine the positioning of the IOL via various methods, as it may reveal the need for more careful investigation.
Screening
Effective glaucoma screening is paramount for the detection, treatment, and management of the disease. This is especially important because the nature of glaucoma is asymptomatic, particularly early in the disease and even in later stages—particularly if it is asymmetrical.9
This places greater gravity on early discovery and management. Mainstays of evaluation such as the IOP and optic nerve appearance are vital and here to stay, but many other tools are also at our disposal.
The pupil—our passageway to the posterior segment—can be indispensable in providing clues. From direct views of pupillary deposition and atrophy to retroilluminated clues on the lenticular integrity, this viewing is rapid and can be a richly revealing peek at glaucomatous risk factors.
References
1. Glaucoma: facts & figures. BrightFocus Foundation. July 14, 2021. Accessed April 5, 2022. https://www.brightfocus.org/glaucoma/article/glaucoma-facts-figures#:~:text=Glaucoma%20is%20a%20leading%20cause,Americans%20age%2040%20and%20over
2. Neri P, Azuara-Blanco A, Forrester JV. Incidence of glaucoma in patients with uveitis. J Glaucoma. 2004;13(6):461-465. doi:10.1097/01.ijg.0000146391.77618.d0
3. Yanoff M, Sassani J. Ocular Pathology. 7th ed. Elsevier Inc; 2015:93-145.
4. Ang GS, Wong T, Nicholas S, Wells AP. Pupil ruff atrophy correlations with intraocular pressure and cup-to-disc ratio in a glaucoma clinic population. Ophthalmology. 2012;119(8):1546-1551. doi:10.1016/j.ophtha.2012.02.028
5. Repo LP, Naukkarinen A, Paljärvi L, Teräsvirta ME. Pseudoexfoliation syndrome with poorly dilating pupil: a light and electron microscopic study of the sphincter area. Graefes Arch Clin Exp Ophthalmol. 1996;234(3):171-176. doi:10.1007/BF00462029
6. Khawaja A, Patel AS, Salim S, et al. Pseudoexfoliative glaucoma. American Academy of Ophthalmology: EyeWiki. November 2, 2021. Updated March 23, 2022. Accessed April 5, 2022. https://eyewiki.aao.org/Pseudoexfoliative_Glaucoma
7. Siddiqui Y, Ten Hulzen RD, Cameron JD, Hodge DO, Johnson DH. What is the risk of developing pigmentary glaucoma from pigment dispersion syndrome? Am J Ophthalmol. 2003;135(6):794-799. doi:10.1016/s0002-9394(02)02289-4
8. Kemp PS, Oetting TA. Stability and safety of MA50 intraocular lens placed in the sulcus. Eye (Lond). 2015;29(11):1438-1441. doi:10.1038/eye.2015.105
9. Kastner A, King AJ. Advanced glaucoma at diagnosis: current perspectives. Eye (Lond). 2020;34(1):116-128. doi:10.1038/s41433-019-0637-2

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.