Expecting the unexpected in ocular cases
Four patients present with previously undiagnosed conditions.
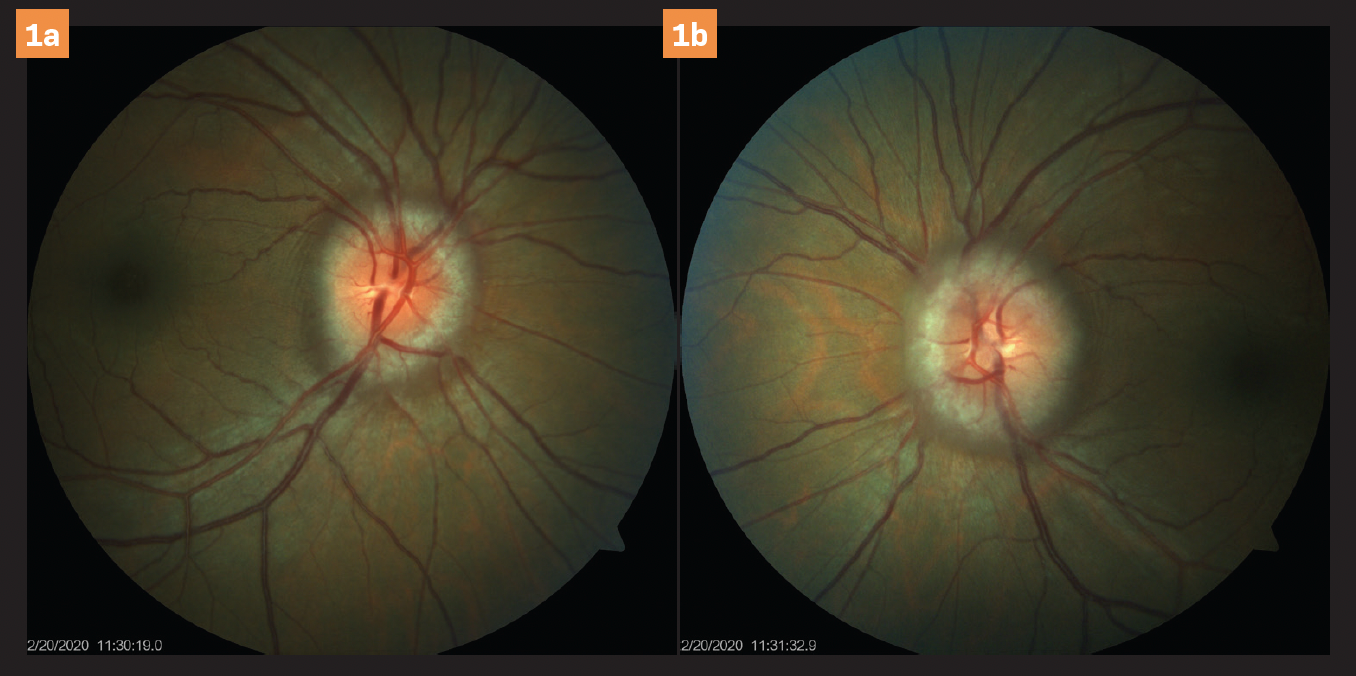
Figure 1 a/b. Significant disc edema OU.
The following are some interesting cases that I saw that were unexpected. These cases are not rare. However, these were also not the diagnoses I expected.
The presentations remind me of the importance of how vigilant optometrists must be as eye care providers by watching not only for unexpected ocular conditions, but systemic manifestations as well.
Case 1
A 43-year-old African American woman presented for a routine eye exam with no visual complaints and wanted a checkup because she had not had one in years.
She visited our practice the week prior while accompanying a family member, was impressed with the staff and office, and decided to schedule an appointment.
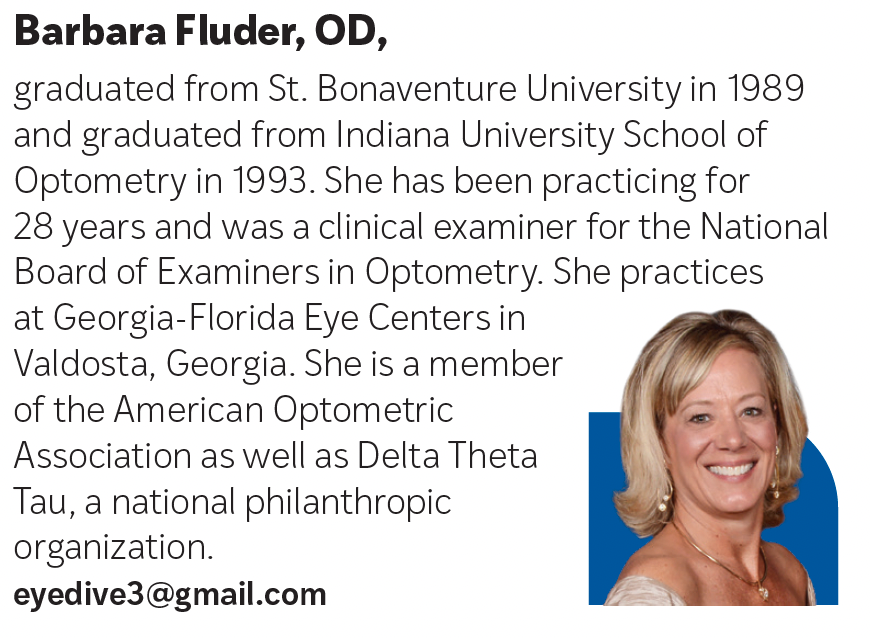
Figure 2. Significant increase in RNFL thickness OU. Click to enlarge.
During the examination, her only complaint was occasional dry eye, for which she used Visine (Johnson & Johnson) as needed. The patient had no history of ocular injuries, infections, or eye surgery.
She did not wear glasses or contact lenses. She had high blood pressure and elevated cholesterol for which she takes losartan (Cozaar), amlodipine (Norvasc), and simvastatin (Zocor). She was 61 in tall, weighed 180 lb, and had a body mass index (BMI) of 34.01.
Her visual acuity was 20/20 OU distance and near. The patient’s refraction was plano OU. Her pupils, confrontations, and extraocular muscles (EOMs) were an unremarkable OU. Intraocular pressures (IOPs) were 18 mm Hg OU.
Anterior segment evaluation was completely normal OU. Posterior segment evaluation revealed a cup-to-disc (CD) ratio of 0.15 OU with disc edema 360° around each optic nerve head, with the left nerve slightly more edematous than the right nerve.
See Figures 1a and 1b. The macula and peripheral retina were unremarkable OU.
Optical coherence tomography (OCT) and retinal nerve fiber layer (RNFL) revealed small CD ratios with an average RNFL thickness of 373 µm in the right eye and 325 µm in the left eye. See Figure 2.
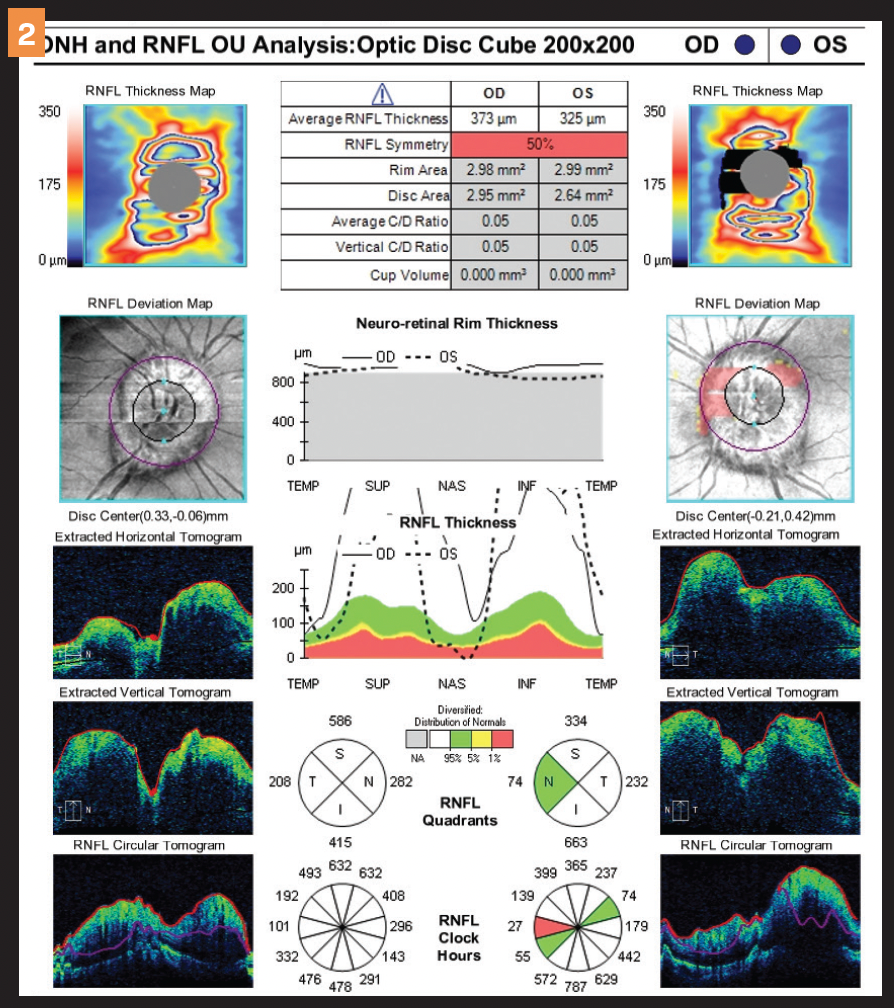
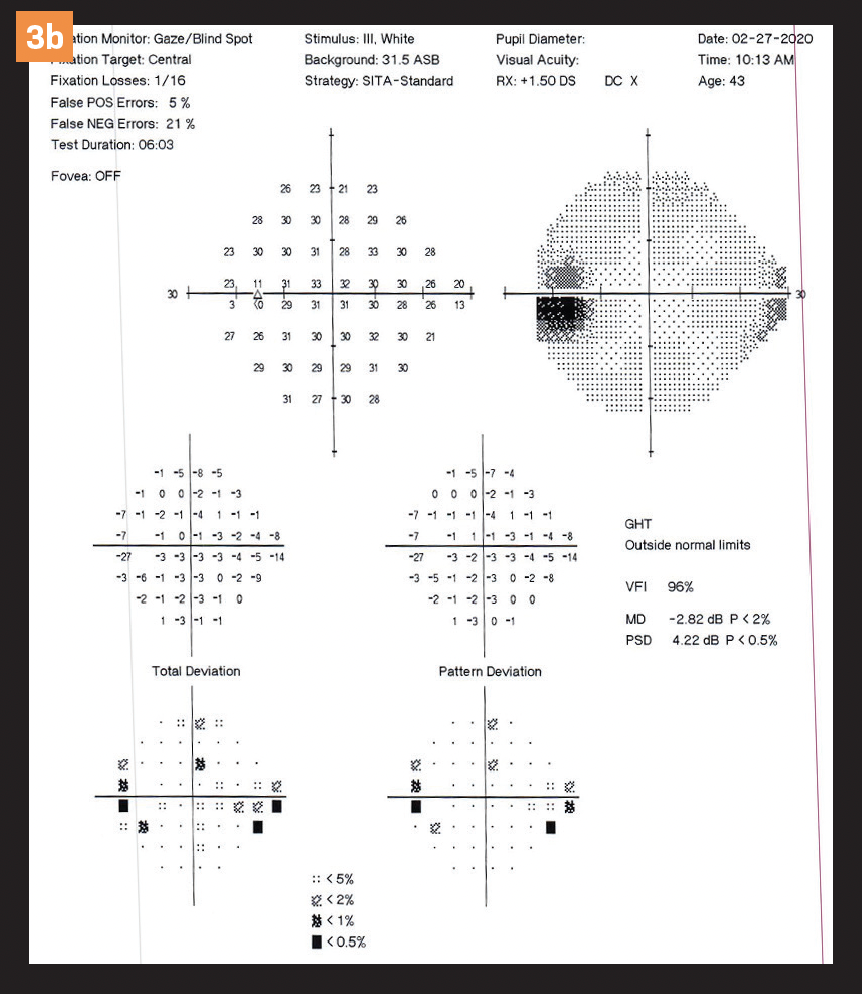
Figure 3 a. Slight enlargement of the blind spot OU. Click to enlarge.
Visual fields revealed slightly enlarged blind spots OU. See Figures 3a and 3b.
The patient was referred to a neurologist for further evaluation and confirmation of idiopathic intracranial hypertension (formerly called pseudotumor cerebri). The patient was started on acetazolamide 250 mg by mouth twice a day.
Figure 3 b. Slight enlargement of the blind spot OU. Click to enlarge.
She has been scheduled for an MRI of the brain and orbits with and without contrast as well as a lumbar puncture.
Obtaining the patient’s height, weight, and BMI helped me in making a sound clinical decision regarding her diagnosis. We are waiting on a follow-up report.
This patient scheduled an exam simply because she was in my office with her aunt and was so impressed that she wanted to have her eyes checked as well.
I did not expect the findings I did and am glad she is receiving treatment for her undiagnosed asymptomatic condition.
Case 2
A 37-year-old Hispanic man presented for an eye exam because of blurred vision and floaters in the right eye for approximately 1 week.
The patient reported his vision in the left eye had been poor due to traumatic injury in the 1990s. He wore glasses that were over 10 years old for distance vision correction, denied any medical condition, and took no medications.
Figure 4. Clinically significant diabetic retinopathy.

Best corrected visual acuity was 20/20 OD and 20/400 OS. Pupils, confrontations, and EOMs were unremarkable. His IOPs were 9 and 11, respectively.
Anterior segment was unremarkable OU. Posterior segment evaluation revealed a CD ratio of 0.35 OD and 0.40 OS with healthy rim tissue. A preretinal hemorrhage and vitreous hemorrhage were present OD.
Neovascularization in posterior pole was present along with microaneurysms, dot and blot hemorrhages, and exudates OU.
The patient had significant proliferative diabetic retinopathy (PDR) with clinically significant edema OU. A large macular scar was noted OS. See Figure 4.
He was referred to a retinal specialist, and treatment will include panretinal photocoagulation OU along with probable injections.
The patient was also referred to a primary care physician and diagnosed with type 2 diabetes with a presenting blood glucose level of 280 mg/dL. He was placed on metformin.
I was not expecting an otherwise healthy 37-year-old man to have undiagnosed type 2 diabetes as well as PDR.
Through a thorough examination, this patient received a much-needed medical diagnosis, treatment for his diabetes, and sight-saving treatment as well.
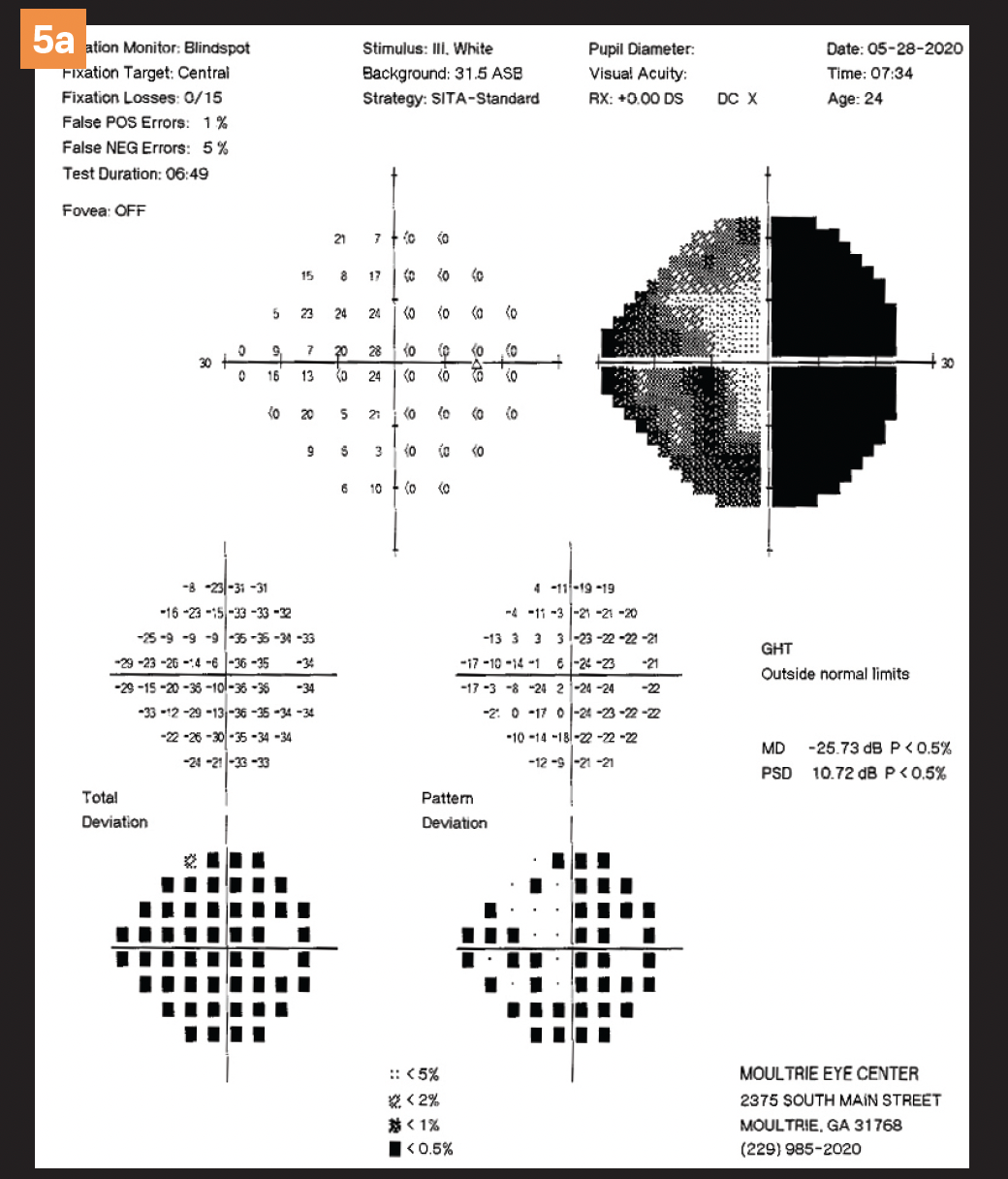
Figure 5 a. Bitemporal visual field defect. Click to enlarge.
Case 3
A 24-year-old Caucasian man presented with a chief complaint of horizontal double vision, pain on movement in extreme gazes, and numbness in his right fingertips for 2 months.
The patient’s general health was unremarkable. Best corrected visual acuity was 20/30 OD, 20/25 OS. Pupils were normal to light and accommodation. EOMs were normal.
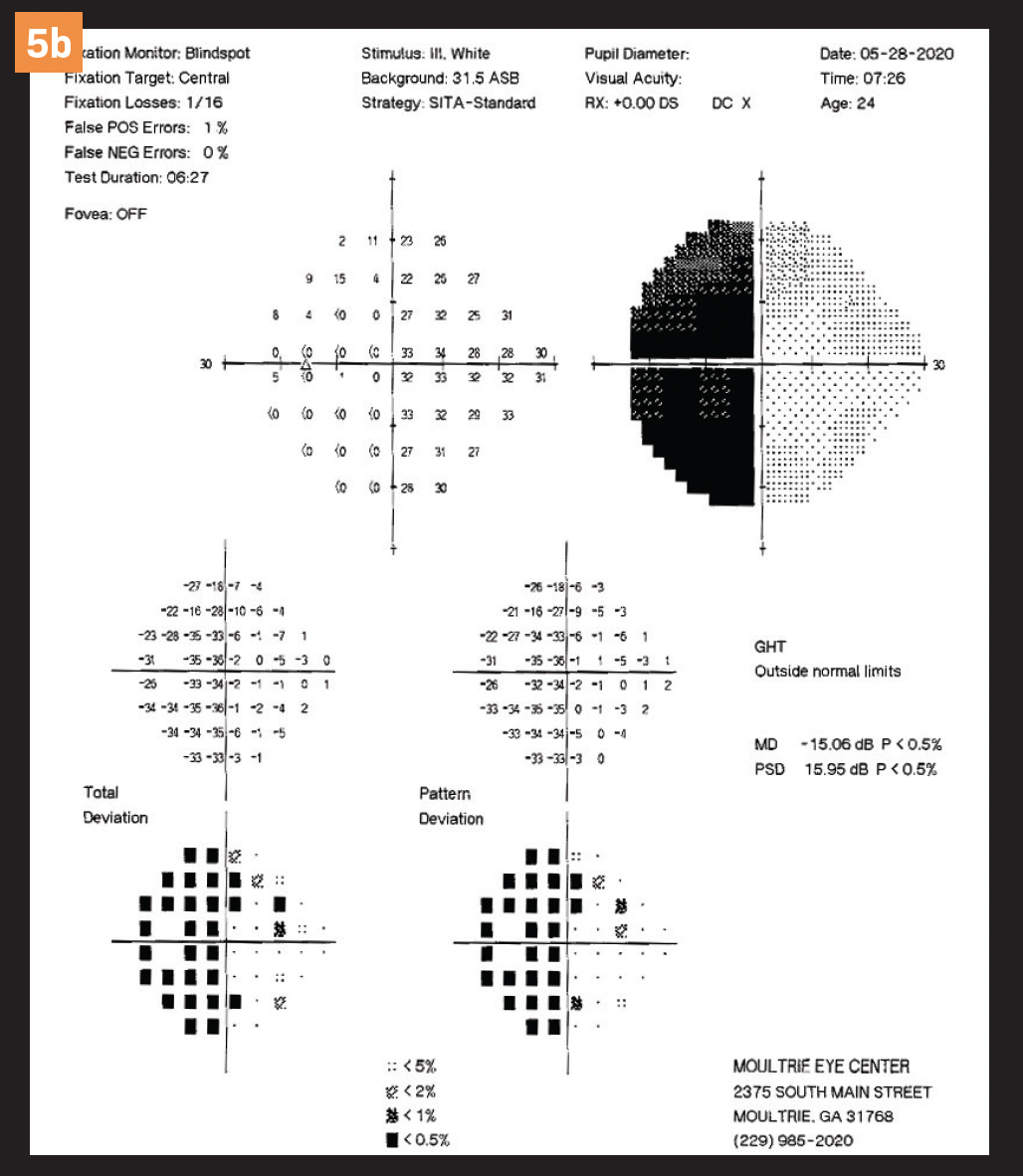
Figure 5 b. Bitemporal visual field defect. Click to enlarge.
Confrontational visual fields showed an inferior temporal defect OD. IOPs were 14 and 19, respectively. Color vision was reduced to 1/7 OD, 3/7 OS. Anterior segment examination was unremarkable OU.
Dilated fundus examination showed a CD ratio of 0.3 and 0.15, respectively, with healthy rim tissue OU. Maculas were normal. Posterior pole and peripheral retina were unremarkable OU.
I diagnosed possible optic neuritis OD. I explained to him that I was concerned about the possibility of multiple sclerosis (MS) and ordered an MRI of the brain and orbits with and without contrast.
A Humphrey visual field test performed a few days later revealed a bitemporal visual field defect. See Figures 5a and 5b. The MRI showed a lobulated circumscribed mass arising from the sella measuring 4.1 cm × 2.6 cm. The differential diagnosis was a pituitary macroadenoma versus meningioma.
I was not expecting to find a pituitary tumor in this patient who clearly showed signs of MS. The patient was referred to a local neurosurgeon, and I am awaiting the results of his evaluation and treatment plan.
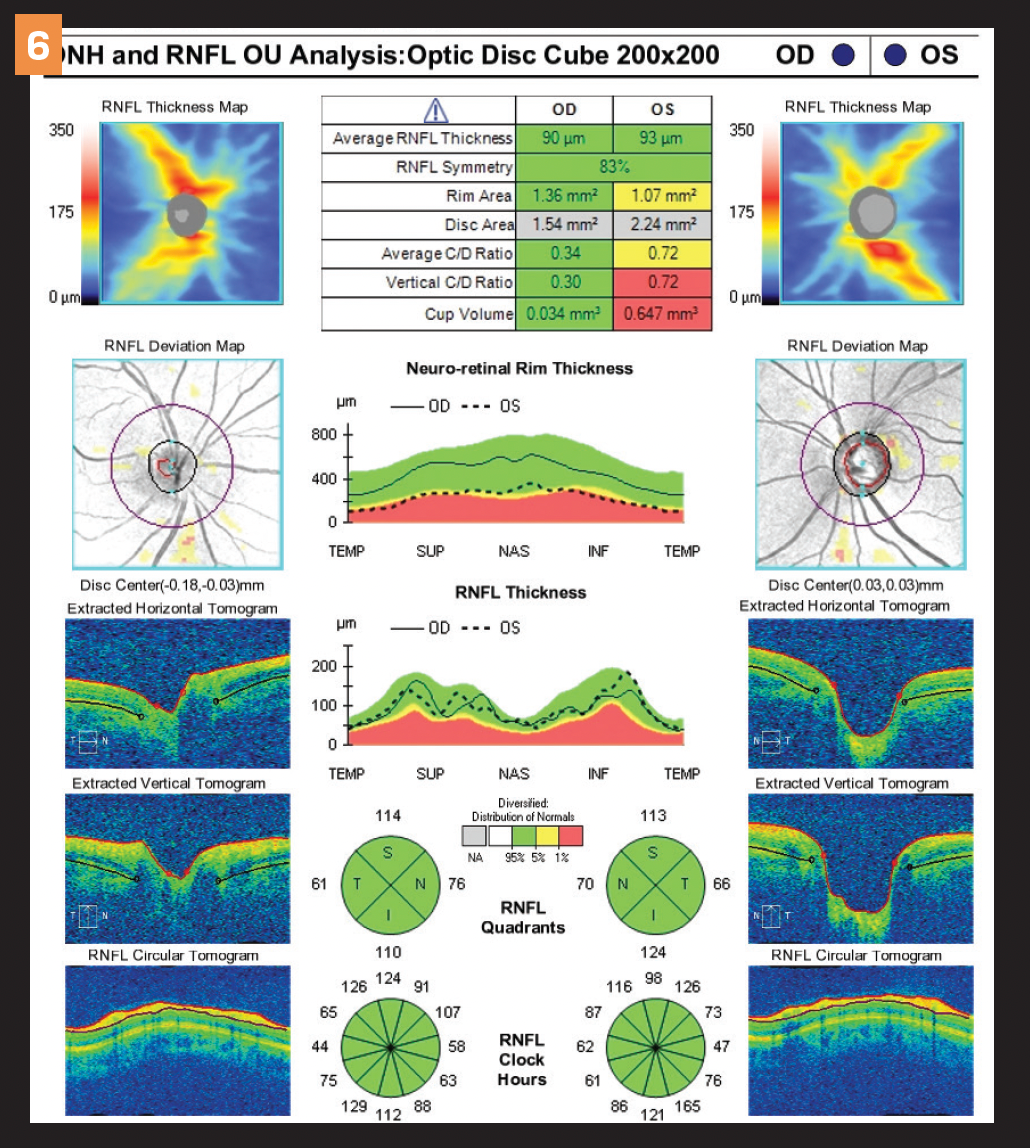
Figure 6.Asymmetric cupping of the nerves with good RNFL OU. Click to enlarge.
Case 4
A 26-year-old Caucasian man presented for a routine eye exam for new glasses because of distance blur. His medical history was unremarkable.
He stated that he had not had worn glasses for 4 years and had tried contact lenses but was unable to tolerate them. However, he stated that he wanted to try them again.
Best corrected visual acuity was 20/25 OD, 20/20 OS. Pupils were equal, round, and reactive to light and accommodation. Confrontational fields were normal OU. IOPs were 27 and 33, respectively. Corneal pachymetry was 556 OD and 547 OS.
Anterior segment examination was unremarkable OU. Dilated fundus evaluation revealed a CD ratio of 0.3 OD and 0.7 OS. The average RNFL thickness on OCT was 90 OD and 93 OS. See Figure 6.
Figure 7 a/b. Normal visual field OU. (All images courtesy of Barbara Fluder, OD)
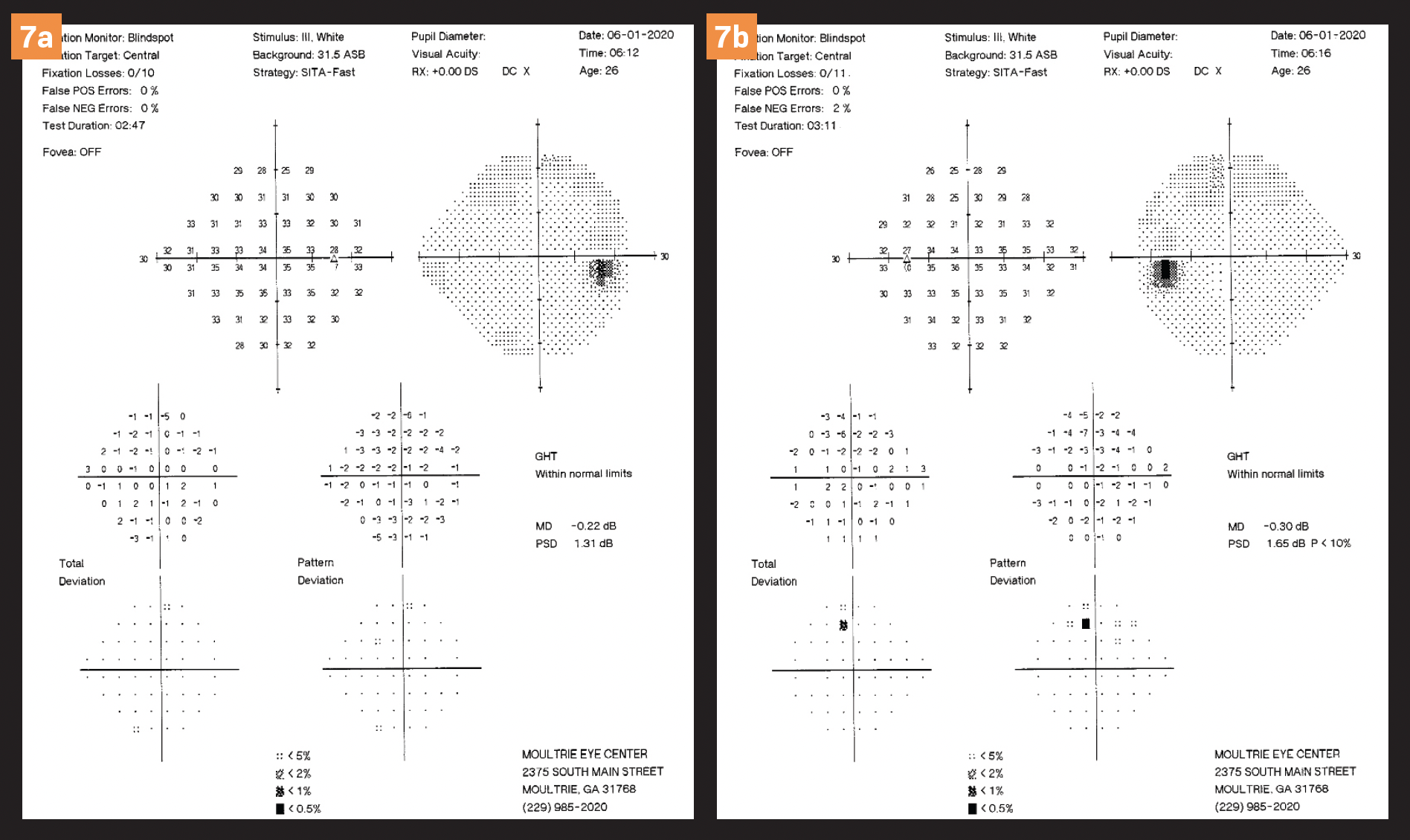
Humphrey visual fields were unremarkable OU. See Figures 7a and 7b. The patient was started on latanoprost at bedtime OU. A follow-up visit showed a reduction in his IOPs to 15 OD and 19 OS.
I did not expect to see primary open-angle glaucoma in a healthy 26-year-old individual coming in for a new prescription for eyeglasses. I was as surprised by these findings as he was.
Fortunately, the patient understood the nature of the disease after seeing his test results and having the findings explained as to what is and is not normal. With continued proper care, this young man will continue to maintain his eyesight for the rest of his life.
It is easy to become settled in our daily routine of fitting eyeglasses and contact lenses. It is noteworthy that all these patients are under the age of 50.
We need to be vigilant and sit up straight in our exam chair saddles so we don’t miss the undiagnosed systemic and/or ocular diseases that afflict many of our patients. Your patients will be eternally grateful for the astute eye care you have given them.

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.