Guideline redefines amniotic membrane’s role in ocular surface disease
Earlier and proactive use is suggested for a variety of corneal diseases
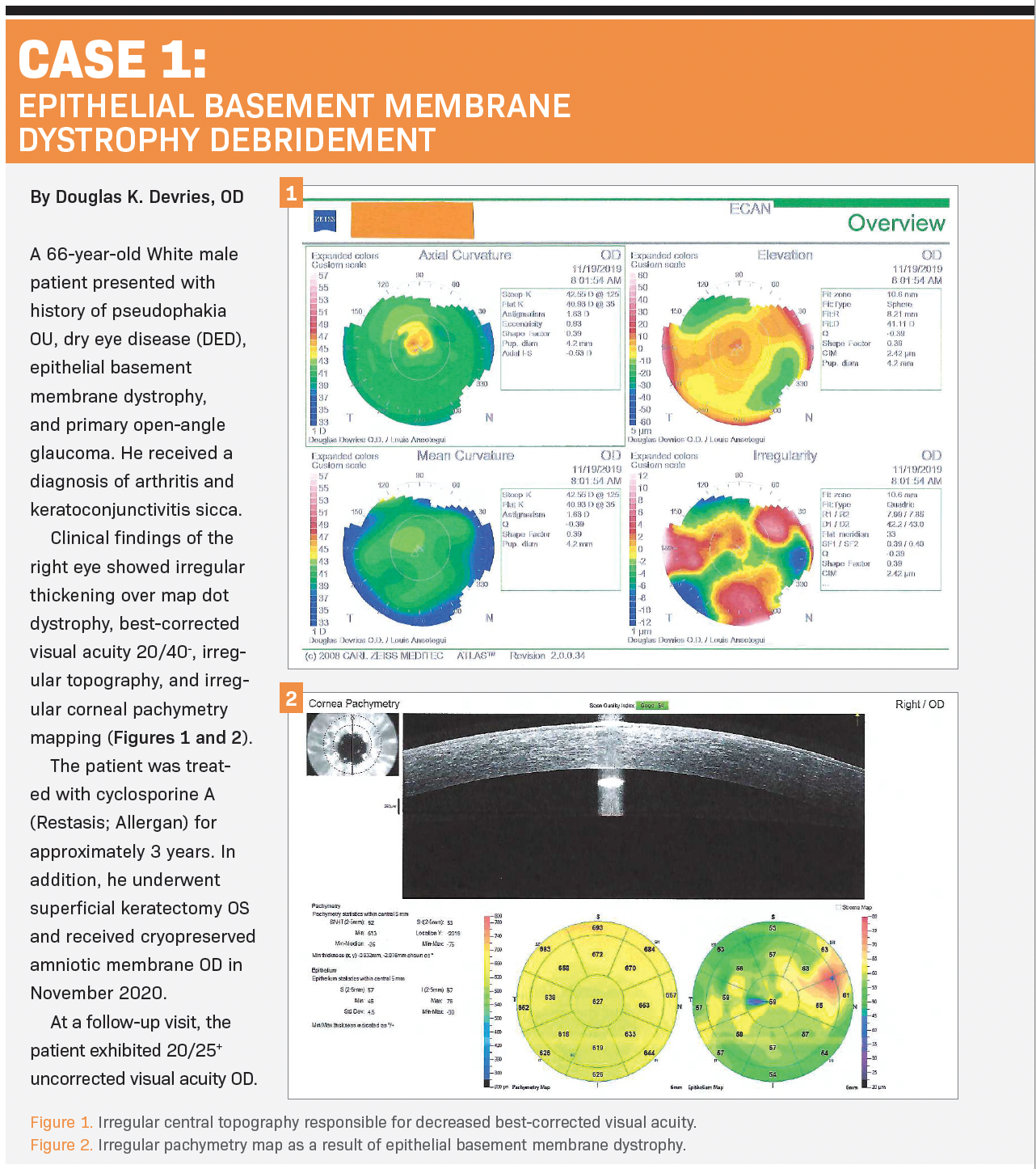
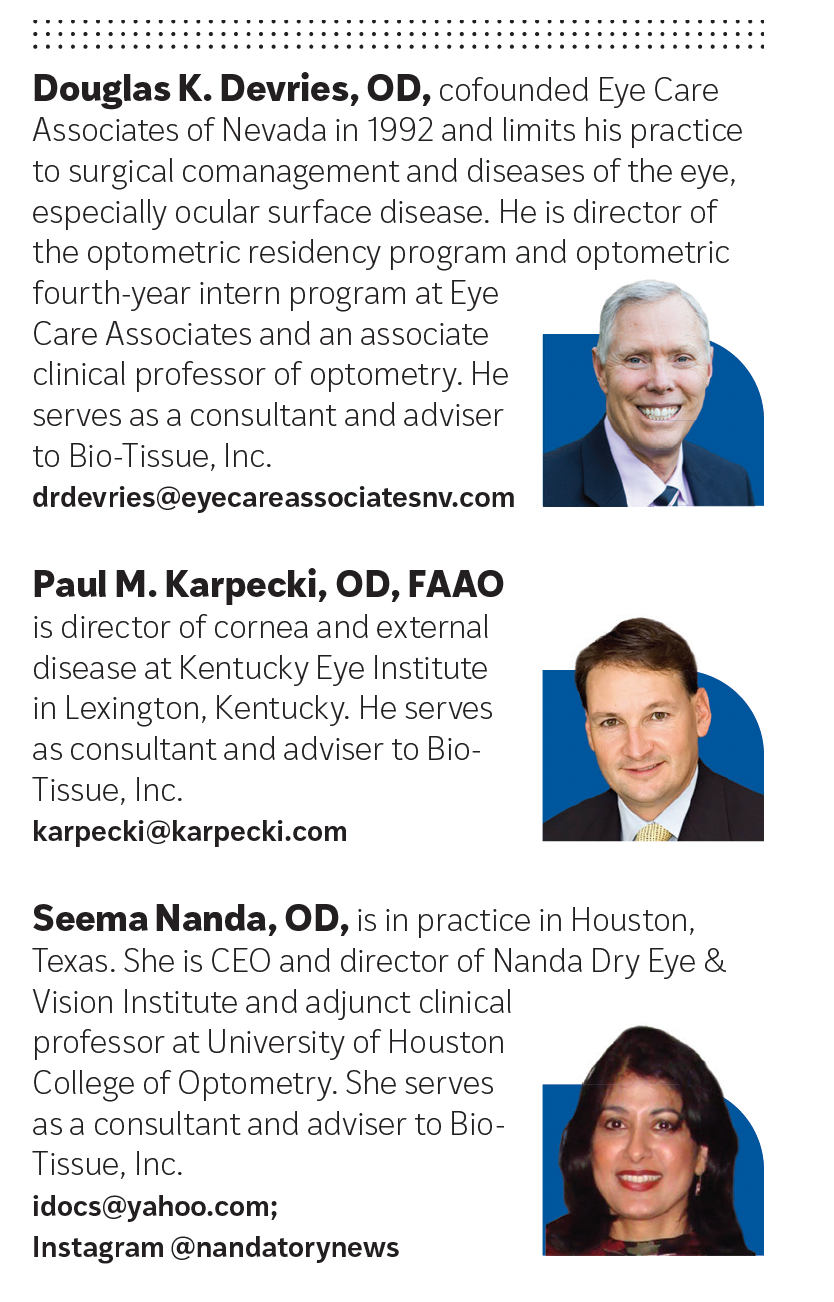
Every day, patients are referred for treatment of corneal-involved ocular surface diseases such as persistent epithelial defect (PED), recurrent corneal erosion (RCE), and epithelial basement membrane dystrophy (EBMD), among others. Many patients have received prior palliative treatments that were initially effective but ultimately insufficient, resulting in a condition that returns worse than before. Fortunately, in many cases, we are able to use cryopreserved amniotic membrane (CAM) to provide permanent relief for these patients.
Our use of CAM for reparative treatment in cases once relegated to palliative care has expanded. As its use becomes increasingly integral to our respective practices, we are in lockstep with ophthalmic corneal surgeons who are incorporating this therapy. Recognition of this expanded role was the impetus for a Consensus Guideline developed by Marguerite McDonald, MD; Neel Desai, MD; Mark Milner, MD; Clifford Salinger, MD; and John Sheppard, MD, MMSc; in conjunction with Bio-Tissue, Inc, manufacturer of CAMs Prokera, AmnioGuard, and AmnioGraft.1
Reexamining the role
The Consensus Guideline reexamines the role of CAM in cornea-involved ocular surface disease (OSD) and notes that for many of these disease states, existing standards rely too heavily on palliative treatments and fail to recommend disease- modifying therapies early in the treatment algorithm.2-4 The guideline authors write that their collective experience with amniotic membrane (AM) for treatment of cornea-involved OSDs and for presurgical optimization of the ocular surface indicates that treatment protocols should include earlier, proactive use of AM.1
Our practice patterns with respect to CAM reflect this and other recommendations. For example, the authors of the guideline indicate that superficial keratectomy followed by application of CAM should be the standard of care for treatment of RCE—and we agree.1 The standards of care for many cornea-involved OSDs—including RCE—routinely recommend bandage contact lenses (BCLs) to passively aid in reepithelialization, but BCLs pose inherent risks, including infectious keratitis, dry eye disease (DED), inflammation, and corneal hypoxia and edema.5
Disease-modifying therapy
Two types of AM are used for ophthalmic purposes: cryopreserved and dehydrated. The guideline authors explain that the cryopreservation process allows CAM to retain heavy chain (HC) peptide covalently conjugated with high molecular weight hyaluronic acid (HA), which is noncovalently complexed with pentraxin-3 (PTX3)—HC-HA/PTX3—and that this biologic matrix is responsible for CAM’s anti-inflammatory and regenerative healing properties.6-9
CAM is distinct from dehydrated AM because CAM provides regenerative healing, characterized by a limited inflammatory and fibrotic response that is maintained in cryopreservation.10 CAM suppresses inflammation by facilitating neutrophil apoptosis, polarizing M1 to M2 macrophages, and suppressing Th1 and Th17 lymphocyte activation; inhibits scarring by preventing myofi broblast differentiation and reprogramming into progenitor cells; and promotes regenerative healing by augmenting mesenchymal stem cell function and maintaining stem cell quiescence.6
Here, we share how we use CAM in our practices, discuss how our efforts reflect the Consensus Guideline, and make recommendations on how to effectively integrate CAM into clinical practice.
Devries on infectious keratitis I have been using CAM for many years to treat OSD, PED, RCE, and EBMD, as well as traumatic corneal injuries, corneal ulcers, and infectious keratitis. I concur with the guideline’s recommendations on when, why, and how to reposition CAM in clinical practice.
For example, the guideline offers examples of situations for which waiting for conventional therapies to fail is not the best practice. In cases of PED, the guideline indicates that the ideal time to use CAM is not after weeks of passive, traditional therapies but instead as the first-line treatment at the point of initial injury. Similarly, the guideline notes that CAM may be an optimal early intervention for epithelial defects in patients with a propensity for poor healing due to concurrent diabetes, a history of herpetic keratitis, or neurotrophic cornea; as well as for patients with exposure keratopathy or a poor blink reflex due to age, neurodegenerative disease, or other factors. These clinical pearls illustrate why I use CAM for corneal ulcers and infectious keratitis:
» Many patients with corneal ulcer or infectious keratitis are candidates for CAM. The Consensus Guideline recommends its use as soon as possible after identifying the origin of the ulcer or keratitis, particularly when the ulcer is central, large, necrotic, or associated with significant inflammation.
» CAM can be used on an active viral or bacterial infection because of its antimicrobial properties and because the infection can be monitored with fluorescein through the amniotic membrane. In patients with active infection, CAM may warrant replacement if it changes from translucent to opaque or dissolves partially or completely.
» In patients with suspected protozoan or fungal keratitis, consider the use of CAM only after a diagnosis can be confi rmed by culture, Gram stain, confocal microscopy—or, more importantly, after a response to topical therapy is observed.
The guideline emphasizes a critical point that influences how I use CAM in my practice. All too often, eye care providers reserve CAM as a last resort when earlier use could have introduced important healing properties and prevented further corneal surface deterioration.

Karpecki on neurotrophic keratitis
In my practice, we have seen many patients who have been let down by treatment with palliative therapeutics. Then we use CAM, and within a very short time they can see and function—it literally changes their lives.
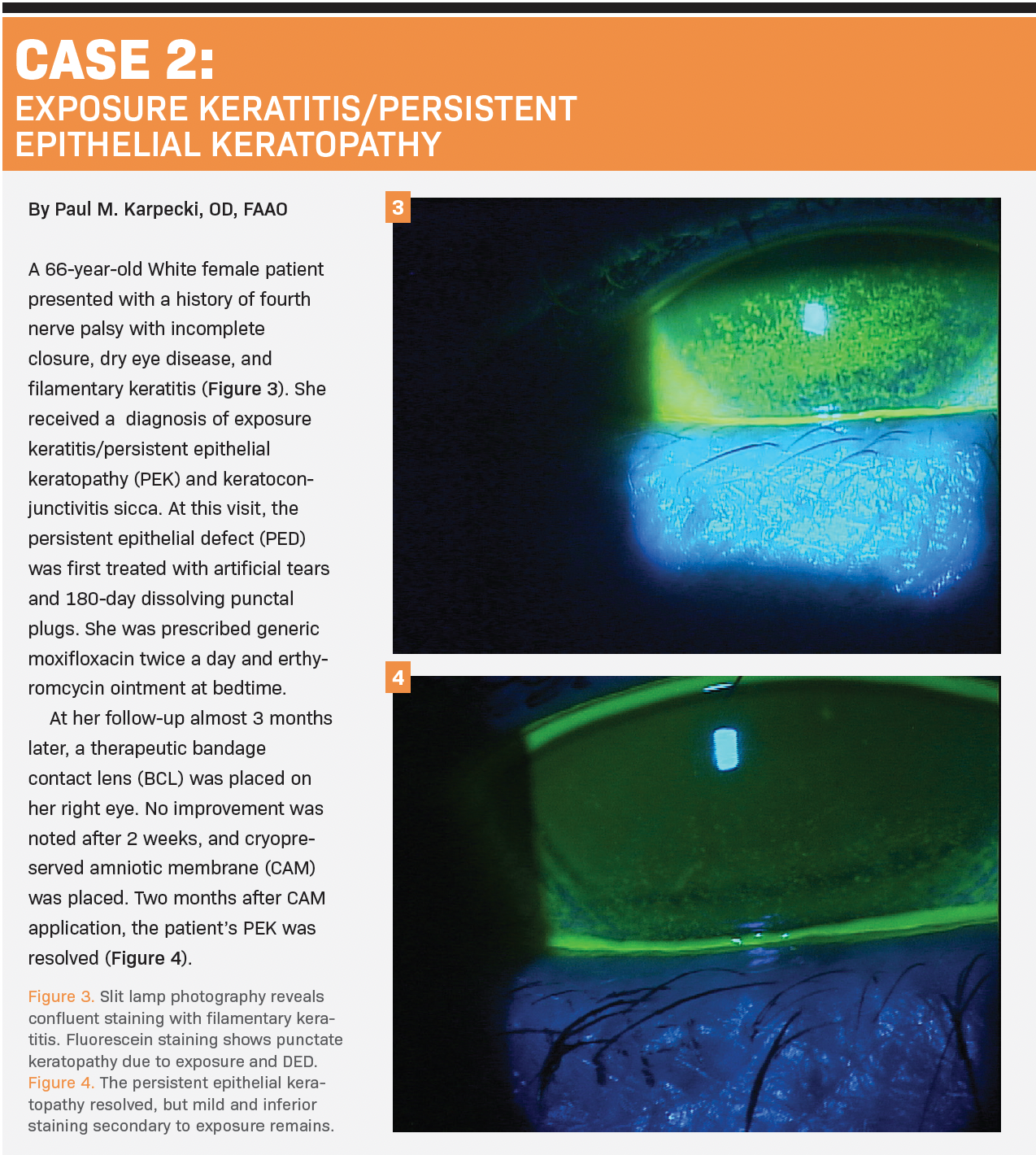
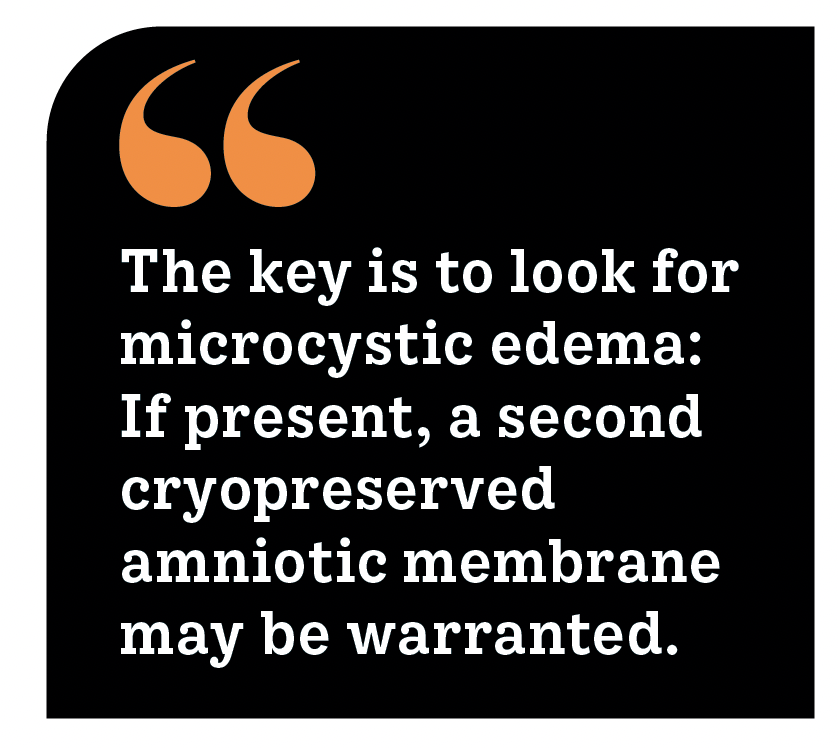
Punctate epithelial keratitis, superficial punctate keratitis related to dry eye, and fi lamentary keratitis are the main dry eye indications for which I use CAM.
We also use it after debridement of EBMD and RCE, as well as Salzmann nodular degeneration removal. In my experience, it has been successful in removing haze after phototherapeutic keratectomy or superficial subepithelial infiltrate scars. Furthermore, it has become a mainstay for recurrent corneal erosions and neurotrophic keratitis (NK).
These clinical pearls demonstrate why I use CAM for NK:
» Dry Eye Workshop (DEWS) II stresses that DED can lead to neurosensory abnormalities and a neurotrophic cornea.11 Because CAM helps regenerate corneal nerves, it provides a benefit for patients with severe DED, who may have diminished sensation and a reduced blink reflex.
» Strong correlation exists between DED severity and the loss of corneal nerves in NK, a degenerative disease caused by damage to the trigeminal nerve.1
The most common causes of NK are herpetic infections, such as with herpes simplex virus, varicella-zoster virus, diabetes, or previous ocular or facial surgery.
» CAM is an effective treatment for this disease and can be used as fi rst-line therapy. Cenegermin-bkbj (Oxervate; Dompé ), a form of human nerve growth factor approved by the FDA for NK, can be used as an adjunctive maintenance treatment to continue to normalize the cornea once CAM has been applied as induction therapy.
For many cases in which I had previously used a BCL, such as PED and fi lamentary keratitis, I start with CAM. The healing response is greater because CAM actively imparts the anti-inflammatory and regenerative healing properties associated with the HC-HA/PTX3 biologic matrix, and it reduces the risk of complications like infiltrative keratitis that can occur with a BCL and cause it to tighten while over a lesion. CAM has not moved higher on my list of options for early disease, but it has moved up on my of list of options for severe corneal disease. This is how I employ CAM in severe DED:
» The optimal use of CAM for persistent, highly symptomatic, or recalcitrant DED is as an adjunctive intervention after first-line therapies have proven inadequate to control the symptoms and signs of OSD.
» CAM may be used in place of steroids, in addition to steroids, or as a steroid-sparing agent for induction therapy in DED as long-term topical anti-inflammatories begin to work.
Nanda on PED, RCE, and EBMD
Patients who have sustained trauma to the cornea and are at risk of developing persistent epitheliopathies are excellent candidates for CAM as fi rst-line therapy. Every day I see people who have had unsuccessful palliative treatment for corneal wounds. The story is always the same: Other frustrated doctors refer these patients out of sheer desperation because they see corneal wounds that close and then reopen a month later.
In cases of RCE, I debride the cornea if the edges are rough, then I apply CAM, and I see the patient back the next day. At that visit, I stain the cornea with fluorescein, with the CAM in place, which allows me to see the degree of improvement. I follow patients according to the amount of injury to their corneas. In milder cases, the cornea may heal quickly, so follow-up may be a week later. With more tissue damage, the cornea may take longer to mend and need another CAM to aid in wound healing. The key is to look for microcystic edema: If present, a second membrane may be warranted. Watch these corneas because erosions can still occur; however, with CAM, the likelihood can be decreased dramatically. I monitor patients every few months until they are healed.
As the Consensus Guideline indicates, CAM provides anti-inflammatory and regenerative healing properties that a BCL does not. The application is just as easy, but the results are far superior. Why? The BCL will dehydrate the cornea, causing an increased propensity of infection because patients do not always adhere to the protocol of using antibiotic drops. Chronic conditions such as herpetic lesions, corneal keratitis, and even centrally located epithelial defects from traumatic injuries can be managed effectively and efficiently with CAM.
Here are pearls for use of CAM to treat PED, RCE, and EBMD:
» Any patient with PED is a candidate for CAM.
» CAM should be used first-line for an acute epithelial defect, proximal to the point of initial injury, when the risk of persistency is high.
» CAM should be considered early for epithelial defects that present a high risk for delayed healing and scarring.
» For patients with RCE and a sloughing epithelium (whether EBMD- or trauma-based) debridement and treatment with CAM should be considered early in the disease process.
» CAM can be used without debridement in RCE without a sloughing epithelium, but with moderate topographic abnormalities and DED.
» If RCE presents alongside an active infection, use CAM as soon as possible after identifying the etiology or antimicrobial sensitivities and controlling the infectious process.
» CAM should be used in any patient with visually or topographically significant EBMD.
» Patients whose EBMD appears to be turning into RCE should be treated with CAM.
Conclusion
CAM helps to treat corneal-involved OSD, as well as the sequelae of moderate to severe DED, earlier in the disease process. The Consensus Guideline reexamines the role of CAM in the treatment of corneal-involved OSD and suggests that treatment protocols include more proactive use of AM at earlier stages, with an emphasis on the benefits of such use of CAM because of its anti-scarring, anti-inflammatory, and antiangiogenic properties. The guideline provides an educational tool for eye care providers interested in introducing CAM to their own patients.
References
1. McDonald M, Desai N, Salinger C, Milner M, Sheppard J. Redefining the standard of care: a consensus guideline. The place of cryopreserved amniotic membrane in treatment protocols for cornea-involved ocular surface disease and before refractive cataract surgery. Bio-Tissue. April 2020. Accessed September 30, 2021. https://www.biotissue.com/ consensus-guide/
2. Gupta S, Gupta P, Sayegh R. Healing a persistent corneal epithelial defect. EyeNet. August 2014. Accessed June 14, 2021. https://www.aao. org/eyenet/article/ healing-persistent-corneal-epithelial-defect
3. Weiner G. Confronting corneal ulcers. EyeNet. July 2012. Accessed June 14, 2021. https://www.aao.org/eyenet/article/ confronting-cornealulcers
4. Thakrar R, Hemmati HD. Treatment of recurrent corneal erosions. EyeNet. March 2013. Accessed June 14, 2021. https://www.aao.org/ eyenet/article/ treatment-of-recurrent-corneal-erosions
5. Pathak AK, Rubins D, Feldman BH, et al. Bandage contact lenses after refractive surgery. EyeWiki. Updated September 13, 2021. Accessed September 26, 2021. https://eyewiki.aao.org/Bandage_Contact_ Lenses_ After_Refractive_Surgery
6. Tseng SC. HC-HA/PTX3 purified from amniotic membrane as novel regenerative matrix: insight into relationship between inflammation and regeneration. Invest Ophthalmol Vis Sci. 2016;57(5):ORSFh11-8. doi:10.1167/iovs.15-17637
7. Jirsova K, Jones GLA. Amniotic membrane in ophthalmology: properties, preparation, storage and indications for grafting-a review. Cell Tissue Bank. 2017;18(2):193-204. doi:10.1007/s10561-017-9618-5
8. Rö ck T, Bartz-Schmidt KU, Landenberger J, Bramkamp M, Röck D. Amniotic membrane transplantation in reconstructive and regenerative ophthalmology. Ann Transplant. 2018;23:160-65. doi:10.12659/ AOT.906856
9. Watson CT, Breden F. The immunoglobulin heavy chain locus: genetic variation, missing data, and implications for human disease. Genes Immun. 2012;13(5):363-373. doi:10.1038/gene.2012.12
10. Cooke M, Tan EK, Mandrycky C, He H, O’Connell J, Tseng SC. Comparison of cryopreserved amniotic membrane and umbilical cord tissue with dehydrated amniotic membrane/chorion tissue. J Wound Care. 2014;23(10):465-474, 476. doi:10.12968/jowc.2014.23.10.465
11. Craig JP, Nelson JD, Azar DT, et al. TFOS DEWS II report executive summary. Ocul Surf. 2017;15(4):802-812. doi:10.1016/j.jtos.2017.08.003
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.