When good retinal surgery makes glaucoma go bad
Use of intravitreal biologics, steroids, and improvements to vitreoretinal surgical techniques have improved the prognosis of vitreoretinal conditions. Ocular hypertension, which may lead to secondary open-angle glaucoma, is a common complication both short- and long-term following intravitreal injection of anti-VEGF or steroid agent and PPV—especially when silicone oil is used as a tamponade agent. Understanding these potential risks is key to early detection, diagnosis, and management following vitreoretinal procedures.
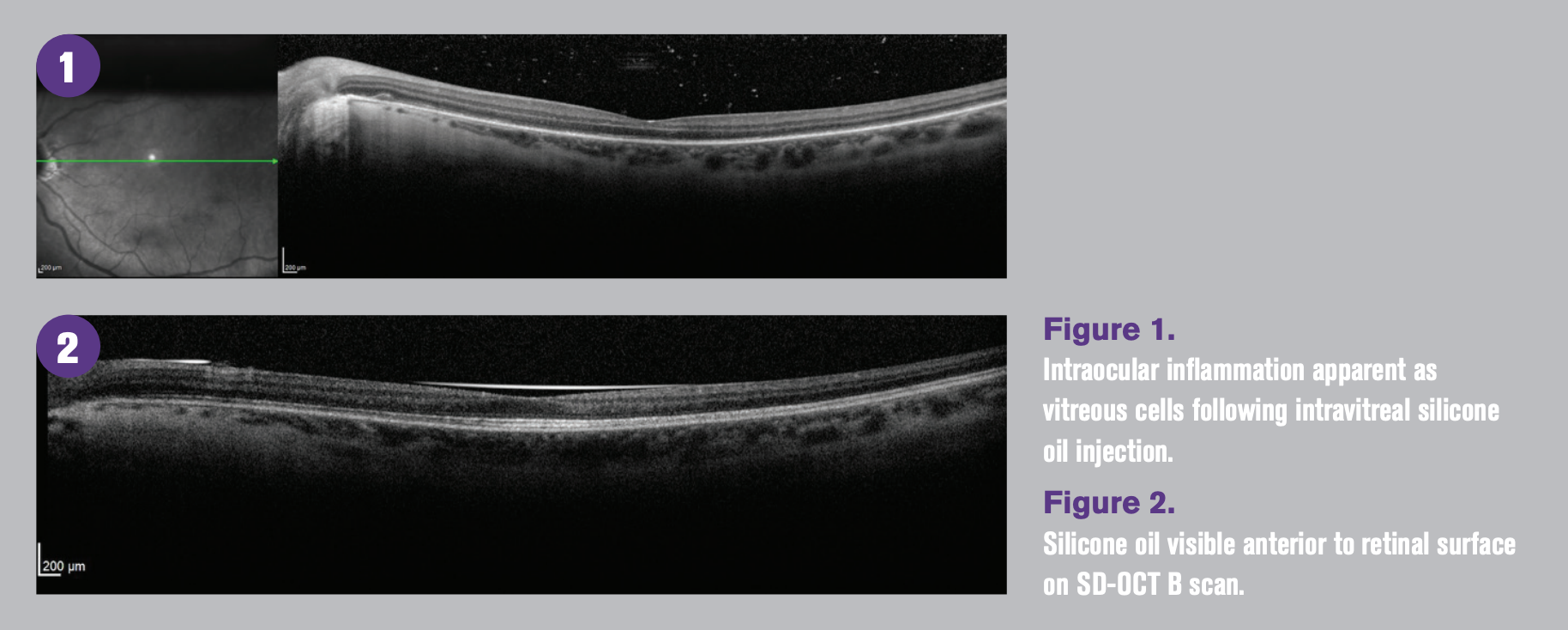
Figure 1. Intraocular inflammation apparent as vitreous cells following intravitreal silicone oil injection. Figure 2. Silicone oil visible anterior to retinal surface on SD-OCT B scan.

The commonality of ocular comorbidities in clinical practice highlights the importance of true primary ophthalmic care and comprehensive eye examinations for the early detection, diagnosis, and management of ocular pathology. Early diagnosis and management with the goal of preventing visual impairment is especially important when managing typically asymptomatic conditions like ocular hypertension and open-angle glaucoma.
When ODs think about identifying risk factors for development of open-angle glaucoma, we typically think about those which have been well-established for primary open-angle glaucoma including family history of glaucoma, advancing age, race, thin central corneal thickness, and increased intraocular pressure (IOP). ODs are less likely to consider risk factors of secondary open-angle glaucoma including history of vitreoretinal procedures such as intravitreal injections and pars plana vitrectomy.1-3
The increasingly widening indications for intravitreal injections and pars plana vitrectomy, along with the increasing myopic population leading to greater incidence of complications including retinal detachment, have made encountering individuals who have undergone, or who are currently undergoing, these procedures more common.2,3
Related: Dr. Casella reviews vitamin B3 for glaucoma management
An understanding of the increased risk that these common vitreoretinal procedures pose to development of ocular hypertension, secondary open-angle glaucoma, or progression of glaucoma is key to appropriate diagnosis, management, and comanagement when these conditions develop.
Intravitreal injections
Intravitreal injections including anti-vascular endothelial growth factor (VEGF) agents and intravitreal steroid agents have developed to be the cornerstone of the management of vitreoretinal disease. Both transient and acute IOP elevation following injection can contribute to development of glaucomatous optic neuropathy and can complicate glaucoma management.3
Immediately following intravitreal injection, a short-term spike of as high as 87 mm Hg can occur due to increased volume in the vitreous cavity which typically normalizes between within one hour.3,4 The acute spike in IOP causes a reduction in macular and peripapillary perfusion, posing risk of occlusion of the central retinal artery.5
It is this rapid reduction in vascular perfusion that accounts for the sudden, temporary vision loss which occurs immediately following an intravitreal injection.5,6 Vision returns when the macula regains perfusion as IOP normalizes.5
The role of vascular dysfunction as one of the underlying mechanisms in the pathogenesis of glaucoma is accepted, but the actual mechanism of elevated IOP and development of optic neuropathy is less clear. Long-term cumulative consequence of repeated, sudden, significant, IOP elevation events on retinal and optic nerve head microcirculation may be an important contributing factor to glaucomatous damage in patients undergoing intravitreal injections.3,5,6
Related: Glaucoma & ocular surface preservation: Key factors for ODs to consider
While topical IOP-lowering medication or oral acetazolamide administered prior to injection has shown a statistically significant reduction of the IOP spike immediately after injection, the clinical benefit of modest IOP reduction is likely insignificant.3,7
Anterior chamber paracentesis is considered to be the most effective way to prevent IOP spike immediately after injection.8 While an increased theoretical risk of complication including endophthalmitis or hypotony exist, there has been insufficient evidence to support that the risk of paracentesis complication outweighs the potential benefit of blunting the IOP spike from intravitreal injection long term.8
Although acute IOP spike immediately after injection due to increased volume in the vitreous cavity may cause long-term damage to retinal and peripapillary microvasculature, based on the lack of difference of IOP between the 2.0 mg and 0.5 mg ranibizumab arms of the HARBOR study, increased intravitreal volume alone does not seem to be the primary driver toward sustained IOP increase over time.9
The mechanism of long-term sustained IOP increase following multiple intravitreal injections has been proposed to be due to one or a combination of 4 major mechanisms leading to reduced trabecular outflow: direct toxicity of the medication to the trabecular meshwork, aggregation of protein or other high-molecular weight compounds including silicone within the trabecular meshwork, low-grade inflammation and trabeculitis, and reduction of nitric oxide.3,6,10,11
Intravitreal silicone particles have been measured in patients who have undergone intravitreal injection with anti-VEGF and corticosteroid agents.3,11
Related: In vivo bulbar conjunctival structures study results in
So, where do these microscopic silicone particles come from?
The most likely source of silicone oil droplets is related to elements of the syringe and needle used for injection. The barrel of the syringe, hub of the needle, tip of the plunger, and stopper of the medication vial all contain microscopic amounts of medical grade silicone oil.11
Because silicone oil is more viscous than the injectable medication, in Luer-lock or Luer-slip syringes, silicone particles are able to collect in the dead space created by the syringe design and then are injected with the medication into the vitreous cavity.11
While silicone oil particles may play a role in directly impeding aqueous outflow, due to their potential to increase intraocular inflammation these particles may also contribute to aqueous outflow reduction due to low-grade trabeculitis.3,11
Patients who undergo a higher number of intravitreal injections with greater frequency are more likely to develop sustained elevated IOP.3,6,10,11
Patients most likely for development of chronic IOP elevation, secondary open-angle glaucoma, and need for incisional surgery are those who have had 20 or more intravitreal injections or who receive 7 or more intravitreal injections per year.3,6
The role of nitric oxide in the signaling pathway leading to relaxation of trabecular meshwork beams and increased trabecular outflow has been extensively studied in glaucomatous and non-glaucomatous eyes and has formed the basis for a novel IOP-lowering medication.10 VEGF upregulates nitric oxide synthase, which leads to an increased concentration of nitric oxide.
Conversely, anti-VEGF agents may decrease nitric oxide in the trabecular meshwork, forming a direct link between anti-VEGF injections and decreased aqueous outflow leading to chronic, sustained elevated IOP.10
What about steroids?
Intraocular steroids including intravitreal triamcinolone, fluocinolone, and dexamethasone all have propensity to increase IOP immediately as a result of increased intraocular volume and longterm by decreasing aqueous outflow, leading to increased risk of ocular hypertension and secondary open-angle glaucoma.
Steroids inhibit trabecular meshwork cell functions, including phagocytosis, resulting in an accumulation of extracellular matrix material. This material clogs the trabecular meshwork and alters cell adhesion and trabecular cytoskeletal molecules, causing a reduction in trabecular outflow and chronic, elevated IOP, especially in younger patients.12
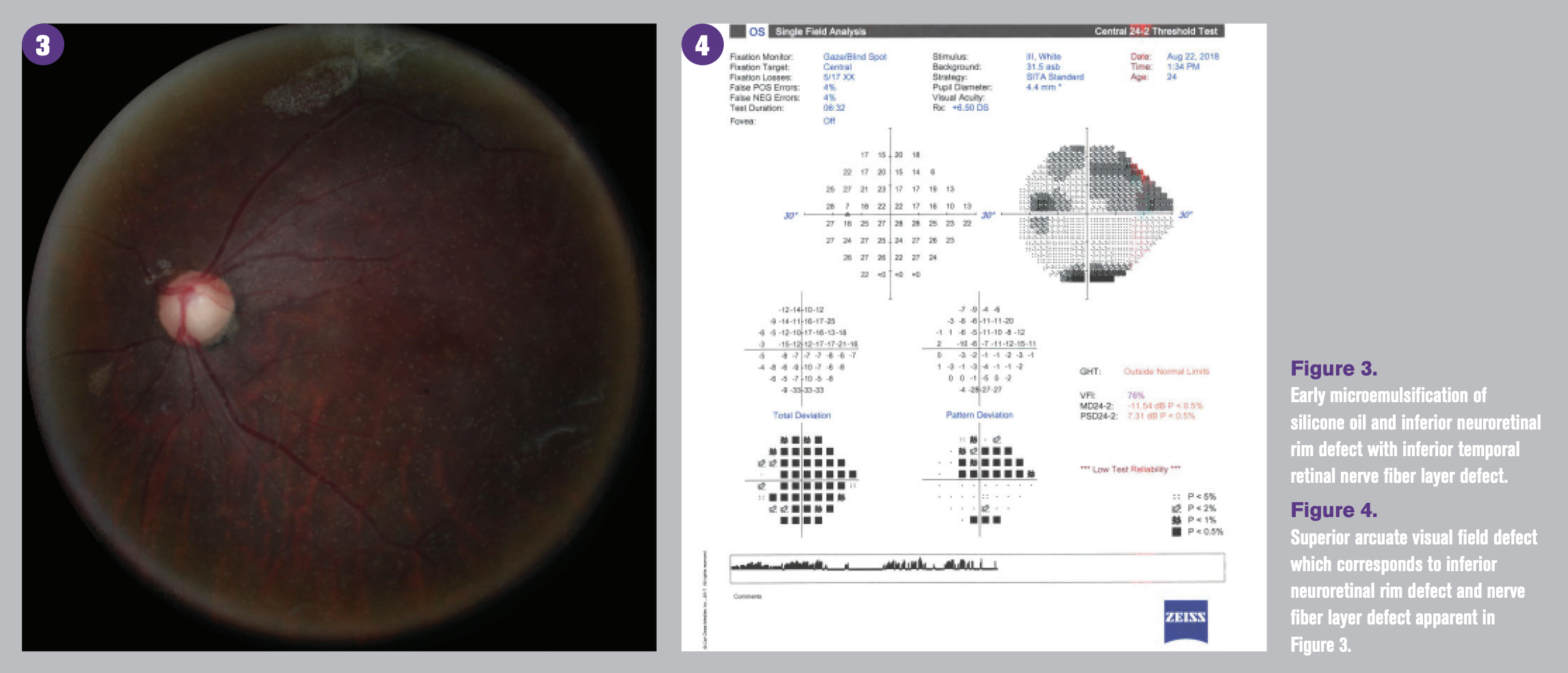
Figure 3. Early microemulsification of silicone oil and inferior neuroretinal rim defect with inferior temporal retinal nerve fiber layer defect. Figure 4. Superior arcuate visual field defect which corresponds to inferior neuroretinal rim defect and nerve fiber layer defect apparent in Figure 3.
Pars plana vitrectomy
Pars plana vitrectomy (PPV) is the third most common ocular surgery following cataract and laser refractive surgery.2 While the operating physician is in the most appropriate position to manage IOP elevation events including pupillary block, displaced gas, or silicone oil into the anterior chamber, or intravitreal gas or silicone oil over-fill within the early postoperative period, late postoperative IOP events and secondary glaucoma are more likely to be identified and managed by comanaging practitioners.
The mechanism of elevated IOP rise following uncomplicated vitrectomy is thought to be due to an increase of oxygen present in the vitreous cavity, resulting in oxidative stress and damage to the trabecular meshwork and therefore decreased aqueous outflow.2,13
Patients who are more likely to develop chronic elevated IOP following vitrectomy are those who have intraoperative use of triamcinolone, a higher pre-operative IOP, and longer axial length, and those who are pseudophakic.2,13
Tamponade agents including expansile gases such as sulfur hexafluoride (SF6), perfluoropropane (C3F8), and silicone oil are common adjuncts used during PPV to increase the likelihood of development of chorioretinal adhesion following retinal reattachment surgery by maintaining adhesion between the retina and retinal pigment epithelium.13 Early postoperative IOP elevation may result from overfill of expansile gas or silicone oil or pupillary block.13-15
While expansile gases including SF6 and C3F8 are naturally resorbed, silicone oil is a long-term, non-resorbable tamponade agent which is typically reserved for patients undergoing complex retinal detachment repair. This includes patients with previous failure of retinal reattachment surgery and development of proliferative vitreoretinopathy, those who need to travel by air, or those who cannot maintain postoperative positioning.15
Chronic postoperative IOP increase leading to glaucomatous optic neuropathy in individuals following PPV and injection of intravitreal silicone oil is common and reported to be as high as 40 percent.14
The mechanism of late postoperative IOP elevation and secondary glaucoma is most commonly related to development of intraocular inflammation or microemulsification and migration of silicone oil into the anterior chamber, which occurs more easily in pseudophakic or aphakic patients. This results in obstruction of the trabecular meshwork with or without synechial angle closure.14-16 Permanent trabecular meshwork damage can occur following anterior segment migration of microemulsified silicone oil, leading to elevated IOP even after silicone oil removal leading to need for medical or surgical management.15-17
Bottom line
The use of intravitreal biologics and steroids as well as improvements to vitreoretinal surgical techniques and surgical adjuncts has greatly improved the prognosis of many vitreoretinal conditions.
Ocular hypertension, which may lead to secondary open-angle glaucoma, is a common complication both short- and long-term following intravitreal injection of anti-VEGF or steroid agent and PPV—especially when silicone oil is used as a tamponade agent.
Considering that IOP elevation is almost always asymptomatic, clinicians comanaging patients undergoing intravitreal injections and those with a history of PPV should periodically evaluate patients, paying careful attention to IOP and clinical optic disc appearance due to increased risk of ocular hypertension and secondary open-angle glaucoma.
Understanding an individual’s risk for propensity to develop sustained elevated IOP is key to early detection, diagnosis and management.
References
1. Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, Parrish RK 2nd, Wilson MR, Kass MA. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002 Jun;120(6):714-30.
2. Reibaldi M, Avitabile T, Russo A, Bonfiglio V, Mariotti C, Romano MR, Boscia F, Cennamo G, Matteo Fallico 1, Parisi G, Castellino N, Bucolo C, Volti GL, Longo A. Late-onset ocular hypertension after vitrectomy a multicenter study of 6,048 eyes. Retina 2019 Nov;39(11):2107-2115.
3. Bracha P, Moore NA, Ciulla TA, WuDunn D, Cantor LB. The acute and chronic effects of intravitreal anti-vascular endothelial growth factor injections on intraocular pressure: a review. Surv Ophthalmol. 2018 May-Jun; 63(3):281-295.
4. Kim JE, Mantravadi AV, Hur EY, Covert DJ. Short-term intraocular pressure changes immediately after intravitreal injections of anti-vascular endothelial growth factor agents. Am J Ophthalmol. 2008 Dec;146(6):930-934.
5. Barash A, Chui TYP, Garcia P, Rosen RB. Acute macular and peripapillary angiographic changes with intravitreal injections. Retina. 2020 Apr;40(4):648-656.
6. Eadie BD, Atminan M, Carleton BC, Maberley DA, Mikelberg FS. Association of repeated intravitreous bevacizumab injections with risk for glaucoma surgery. JAMA Ophthalmol. 2017;135:363-368.
7. Ozcaliskan S, Ozturk F, Yilmazbas P, Beyazyildiz O. Effect of dorzolamide-timolol fixed combination prophylaxis on intraocular pressure spikes after intravitreal bevacizumab injection. Int J Ophthalmol. 2015 Jun 18;8(3):496-500.
8. Saxena S, Lai TY, Koizumi H, Farah ME, Ferrara D, Pelayes D, Sato T, Meyer CH, Murray T, International Pharmacokinetic Collaboration. Anterior chamber paracentesis during intravitreal injections in observational trials: effectiveness and safety and effect. Int J Retina Vitreous. 2019 Mar 6;5:8.
9. Ho AC, Busbee BG, Regillo CD, Wieland MR, Van Everen SA, Li Z, Rubio RG, Lai P; HARBOR Study Group. Twenty-fourmonth efficacy and safety of 0.5 mg or 2.0 mg ranibizumab in patients with subfoveal neovascular age-related macular degeneration. Ophthalmology. 2014 Nov;121(11):2181-2192.
10. Morshedi RG, Ricca AM, Wirostko BM. Ocular hypertension following intravitreal antivascular endothelial growth factor therapy: review of the literature and possible role of nitric oxide. J Glaucoma. 2016 Mar;25(3):291-300.
11. Sharma A, Kumar N, Bandello F, Loewenstein A, Freund KB. Understanding intravitreal silicone oil droplets due to intravitreal injections. Retina. 2019 Jul;39(7):1233-1235.
12. Kiddee W, Trope GE, Sheng L, Beltran-Agullo L, Smith M, Strungaru MH, Baath J, Buys YM. Intraocular pressure monitoring post intravitreal steroids: a systematic review. Surv Ophthalmol. Jul-Aug 2013;58(4):291-310.
13. Chang S. LXII Edward Jackson lecture: open angle glaucoma after vitrectomy. Am J Ophthalmol. 2006 Jun;141(6):1033-1043.
14. Honavar SG, Goyal M, Majji AB, Sen PK, Naduvilath T, Dandona L. Glaucoma after pars plana vitrectomy and silicone oil injection for complicated retinal detachments. Ophthalmology. 1999 Jan;106(1):169-76; discussion 177.
15. Barca F, Caporossi T, Rizzo S. Silicone oil: different physical proprieties and clinical applications. Biomed Res Int. 2014;2014:502143.
16. Jabbour E, Azar G, Antoun J, Kourie HR, Abdelmassih Y, Jalkh A. Incidence and risk factors of ocular hypertension following pars plana vitrectomy and silicone oil injection. Ophthalmologica. 2018;240(3):129-134.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.